*Note: If you find the text on some of the images blurry or hard to read, right-clicking the image and then selecting “open image in new tab” may improve the issue.
Policy Concerns
- Providing low-income Texans with mental health and/or substance use conditions who are ineligible for Medicaid access to supports and services.
- Expanding Medicaid to ensure individuals with mental health and/or substance use conditions have access to treatment, services, and supports.
- Ensuring adequacy of Medicaid reimbursement rates for mental health, substance use, and primary care services and providers.
- Planning for the discontinuation of Medicaid 1115 Transformation Waiver funding and the sustainability of Delivery System Reform Incentive Payment (DSRIP) projects providing behavioral health services.
- Continuing efforts to enforce mental health and substance use parity within Medicaid and CHIP.
- Addressing Texas having the highest uninsured rate of both adults and children in the country.
- Monitoring and ensuring mental health, substance use, and primary care network adequacy in Medicaid managed care.
- Ensuring access to quality community-based mental health and substance use services through integrated service delivery and managed care models that emphasize recovery, prevention, and continuity of care.
- Protecting state funding for substance use services to keep Texas from being penalized for the required Maintenance of Effort (MOE) requirement for federal block grant funding.
- Addressing mental health and substance use workforce shortage issues, particularly the lack of diverse providers and availability in rural areas.
- Expanding opportunities for peer support specialist, recovery coach, and family partner support services.
- Addressing the Medicaid reimbursement rates for peer services to reflect their importance and incentivize utilization by providers.
- Ensuring the ongoing success and improvement of services for children and youth available through the YES Waiver.
- Monitoring efforts of the state hospital redesign to ensure a comprehensive continuum of supports and services.
- Improving individual outcome performance measures to focus more on behavioral health outcomes and patient-centered recovery, and less on easy-to-measure outputs.
- Expanding access to coordinated specialty care teams for individuals experiencing first episode psychosis.
- Addressing the RTC bed wait list of children experiencing serious emotional disturbances (SEDs) who are at risk of being relinquished into the custody of Child Protective Services in order to receive mental health treatment.
- Coordinating cross-agency efforts to address the mental health needs of individuals with intellectual disabilities.
- Improving access to trauma-informed training across HHSC divisions specific to children and adults with intellectual disabilities.
- Accessing crisis services, including emergency respite.
- Implementing systems-wide trauma-informed care, positive behavior interventions and supports, and person-centered recovery-focused practices.
- Improving mental health and substance use services in state-supported living centers and community-based waiver programs.
- Improving wait list time for inpatient and community-based mental health and substance use services.
- Ensuring access to broadband and needed technology for telehealth and telemedicine
- Ensuring access to mental health and substance use services through telehealth and telemedicine, and across the state, particularly in rural and low-income areas; ensuring parity with in-person services and allowing the use of audio-only telephone
- Addressing the behavioral health needs of pregnant and postpartum women.
- Improving availability to affordable, safe, and supportive housing for individuals living with mental health and/or substance use conditions.
- Ensuring access to appropriate recovery support services for individuals receiving medication-assisted treatment (MAT).
- Monitoring the implementation of the All Texas Access project and its’ regional plans addressing mental health services.
- Expanding eligibility for Medicaid reimbursed peer support services to youth under the age of 21.
- Improving recovery-oriented supports with increased availability of peer recovery coaches, Recovery Community Organizations (RCOs), and community-based aftercare.
- Increasing access to school and community-based substance use prevention programs.
Fast Facts
- The 2020-2021 HHSC appropriation of all funds was over $76 billion and comprised 30 percent of the state’s entire budget.
- In January 2020, 3,870,036 individuals were enrolled in Medicaid and 352,725 enrolled in CHIP in Texas.
- Children without disabilities account for 69 percent of Medicaid enrollment but only 30 percent of program spending on direct healthcare services.
- In 2018, Medicaid covered approximately 53 percent of births, 44 percent of children across the state, and 62 percent of nursing home residents in Texas.
- Texas has 73 Federally Qualified Health Centers (FQHCs) serving over 1.4 million Texans at more than 300 sites statewide.
- The population growth in Texas between 2010 and 2019 (15.3 percent) was more than double the national average (6.3 percent), resulting in increased demand for HHSC-funded services.
- As of June 2020, Texas had only met about 36 percent of the state’s need of mental health professionals and 214 counties were designated as either full or partial Health Professional Shortage Areas for Mental Health (HPSA-MH).
- As of August 2020, Texas has 506 people trained as certified mental health peer specialists (MHPS), 246 certified recovery support peer specialists (RSPS), and 222 peer specialist supervisors (PSS), enabling them to use their lived experiences with behavioral health issues to help recipients of HHSC-funded services.
- In 2018, over 12 million adults in the United Stated were living with a co-occurring substance use and mental health condition.
- Almost half of individuals who live with a mental health condition also live with a substance use condition.
- Over 60 percent of adolescents receiving community-based substance use treatment also meet diagnostic criteria for a mental illness.
- It is estimated that as many as 30 to 40 percent of persons with intellectual disabilities are diagnosed with a mental health condition and are three to five times more likely to have a co-occurring mental health condition than the general population.
- Children with intellectual and other developmental disabilities (IDD) are more likely to have experienced traumatic events when compared to those without disabilities. However, the known rate of abuse may be higher due to underreporting or lack of recognition by family and other caregivers.
- Individuals with IDD who have a dual diagnosis or who present behavioral “challenges” are more likely to be institutionalized and are often the last to be released to a community-based setting. Additionally, community services and supports are frequently incapable of meeting the behavioral health needs of these individuals, leading to less successful outcomes when transitioning into the community.
- Individuals aged 18-25 are at the highest risk of overdose as they are more likely than any other age group to misuse a prescription medication, use an illicit drug, or use heroin.
- As of April 2020, there were 449 individuals waiting for a maximum-security forensic state hospital bed, with the average of 289 days on the waiting list.
- As of April 2020, there were 451 individuals waiting for a non-maximum-security forensic state hospital bed, with the average of 76 days on the waiting list.
HHSC Acronyms
- ACA – Affordable Care Act
- ACT – Assertive Community Treatment
- ANSA – Adult Needs and Strengths Assessment
- APS – Adult Protective Services
- APS PI – Adult protective services provider investigations
- ASD – Autism spectrum disorders
- BHAC – Behavioral Health Advisory Committee
- CANS – Child and Adolescent Needs and Strength Assessment
- CBT – Cognitive Behavioral Therapy
- CHIP – Children’s Health Insurance Program
- CIHCP – County Indigent Health Care Program
- CIL – Centers for Independent Living
- CLOIP – Community living options information process
- CMS – Centers for Medicaid and Medicare Services
- COPSD – Co-occurring psychiatric and substance abuse disorders services
- COVID- 19 – Coronavirus disease of 2019
- CPS – Child Protective Services
- CRS – Comprehensive rehabilitation services
- CSC – Coordinated specialty care
- DADS – Department of Aging and Disability Services
- DARS – Department of Assistive and Rehabilitative Services
- DDS – Disability Determination Services
- DFPS – Department of Family and Protective Services
- DSM-V – Diagnostic and Statistical Manual of Mental Disorders, 5th edition
- DSRIP – Delivery System Reform Incentive Payment
- ECI – Early Childhood Intervention
- IDEA – Individuals with Disabilities Education Act
- FEP – First Episode Psychosis
- FFCC – Former foster care children
- FMAP – Federal medical assistance percentage
- FPG – Federal poverty guidelines
- FPL – Federal poverty level
- FQHC – Federally Qualified Health Center
- GAO – Government Accounting Office
- GR – General revenue
- HCBS-AMH – Home and Community-based Services – Adult Mental Health
- HCS – Home and community-based services
- HCSSA – Home and community support services agency
- HEDIS – Healthcare Effectiveness Data and Information Set
- HHS – Health and Human Services
- HHSC – Health and Human Services Commission
- HPSA – Health professional shortage area
- HPSA-MH – Health professional shortage area for mental health
- ICF/IDD – Intermediate care facility-intellectual and developmental disabilities
- ICM – Intensive case management
- ICR – Inpatient competency restoration
- IDD – Intellectual and other developmental disabilities
- IL – Independent living
- IMD – Institutions for Mental Diseases
- IST – Incompetent to stand trial
- JBCR – Jail-based competency restoration
- LAR – Legally authorized representative
- LBB – Legislative Budget Board
- LBHA – Local behavioral health authority
- LIDDAs – Local intellectual/developmental disability authorities
- LMHAs – Local mental health authorities
- LOC – Level of care
- LOC-A – Level of care-authorized
- LOC-EO – Level of care-early onset
- LOC-R – Level of care-recommended
- LOS – Length of stay
- LTSS – Long-term services and supports
- MAT – Medication-assisted treatment
- MCO – Managed care organization
- MCOT – Mobile crisis outreach teams
- MDCP – Medically Dependent Children’s Program
- MOU – Memorandum of Understanding
- MOE – Maintenance of Effort
- MSU – Maximum security unit
- MTFCY – Medicaid for Transitioning Foster Care Youth
- NQTLs – Non-quantitative treatment limits
- NWI – National Wraparound Initiative
- OCR – Outpatient competency restoration
- ODPC – Office of Disability Prevention for Children
- OSAR – Outreach, screening, assessment, and referral center
- PASRR – Preadmission screening and resident review
- QTLs – Quantitative treatment limits
- RHP – Regional healthcare partnership
- ROSC – Recovery-oriented systems of care
- RSS – Recovery support services
- RTC – Residential treatment center
- SAMHSA – Substance Use and Mental Health Services Administration
- SBIRT – Screening, brief intervention, and referral to treatment
- SCI – Spinal cord injury
- SED – Serious emotional disturbance
- SH – State hospital
- SMI – Serious mental illness
- SNAP – Supplemental Nutrition Assistance Program
- SOC – Systems of care
- SPA – Medicaid state plan amendment
- SPMI – Serious and persistent mental illness
- SSA – Social Security Administration
- SSDI – Social Security Disability Income
- SSI – Supplemental Security Income
- SSLC – State-supported living center
- STAR – State of Texas Access Reform
- STAR Health – State of Texas Access Reform program for children in CPS system
- STAR Kids – State of Texas Access Reform program for children with disabilities eligible for SSI
- STAR+Plus – State of Texas Access Reform program that includes long-term services and supports
- SUD – Substance use disorder
- TANF – Temporary Assistance for Needy Families
- TAS – Transition assistance services
- TBI – Traumatic brain injury
- TCCP – Texas Code of Criminal Procedures
- TDCJ – Texas Department of Criminal Justice
- TDHCA – Texas Department of Housing and Community Affairs
- TDI – Texas Department of Insurance
- TEA – Texas Education Agency
- TJJD – Texas Juvenile Justice Department
- TMHP – Texas Medicaid Healthcare Partnership
- TOPDD – Texas Office of Prevention of Developmental Disabilities
- TRI – Texas Recovery Initiative
- TRR – Texas Resiliency and Recovery
- TVC – Texas Veterans Commission
- TWC – Texas Workforce Commission
- YES Waiver – Youth Empowerment Services Waiver
Texas Health and Human Services System Organizational Chart

Source: Texas Health and Human Services Commission. (2020, October 1). Health and Human Services system organizational chart [PDF file]. Retrieved from https://hhs.texas.gov/sites/default/files/documents/about-hhs/ leadership/hhs-org-chart.pdf
Overview
The Texas Health and Human Services Commission (HHSC) is the umbrella agency providing a multitude of services and programs to Texans. HHSC programs and services include Medicaid, Children’s Health Insurance Program (CHIP), long-term services and supports, Supplemental Nutrition Assistance Program (SNAP) food benefits, temporary assistance for needy families (TANF) cash benefits, mental health and substance use services, and services for older Texans, women, and people with disabilities. Services are delivered through a complex system of programs and benefits. HHSC also oversees certain regulatory functions such as nursing facility licensing and credentialing, licensing of childcare providers, certain professional licensing and certification, and management of state supported living centers and state psychiatric facilities.
The Texas Department of State Health Services (DSHS) is also under the HHSC agency umbrella but operates as a separate department. DSHS focuses on public health functions such as vital statistics, compiling and disseminating health data, prevention of chronic and infectious diseases, maternal and child health, laboratory testing, and licensing and regulating certain facilities and operations.
Over the last 17 years, the Texas Health and Human Services system has undergone extensive reorganization in an attempt to produce a more efficient, effective, and responsive system. The HHSC transformation began in 2003 as the umbrella agency overseeing multiple programs and departments. After the 2015 Sunset Review Commission review and subsequent recommendations through SB 200 (85th, Nelson/Price), reorganization efforts prioritized agency consolidation. Several client services were transferred to HHSC, including state hospital inpatient services, SSLCs, and some regulatory and administrative services. This transfer eliminated both the Department of Assistive and Rehabilitative Services (DARS) and the Department of Aging and Disability Services (DADS). Additionally, behavioral health and regulatory functions (previously administered by DSHS and the Department of Family and Protective Services (DFPS)), the Office of Mental Health Coordination, and the Forensic Director position were transferred to HHSC over the next few years. As transformation continued, DFPS became an independent agency, and the Health and Human Services system consequently became solely comprised of HHSC and DSHS.
Additionally, the HHSC Executive Council was established during the transition. The primary purpose of the council is to obtain public input and to advise the HHSC executive commissioner on policies relating to the health and human services system. Information on the HHSC Executive Council is available at https://hhs.texas.gov/about-hhs/leadership/councils/ health-human-services-commission-executive-council.
Transformation planning and implementation continues within the HHS system and is led by the Transformation, Policy and Performance Office, which reports to the Chief Policy Officer. The Chief Policy Officer reports directly to the executive commissioner and is responsible for innovation, performance management, policy development, and data analysis.
The transformation of the HHS system is overseen by the Joint Health and Human Services Transition Legislative Oversight Committee. The committee is made up of four members of the Texas Senate, four members of the Texas House, three governor-appointed public members, and the HHSC Executive commissioner as an ex officio member. According to Chairwoman Nelson, the committee’s charges are to ensure easier access to services for individuals, remove blurred lines of authority, remove barriers to system-wide improvements, and improve overall efficiency.
Changing Environment
Prior to the Texas Legislature’s 86th session, leadership committed to prioritize major initiatives including school finance reform and local property taxes. Additionally, mental health and substance use continued to garner significant attention, with school safety/mental health and opioid use highlighted as important policy agenda. The Texas Legislature continued to invest resources to improve access to both adult and youth behavioral supports and services, address the mental health workforce shortage, and re-design the state’s hospital system. The investment made to continue the redesign and construction of inpatient mental health services is imperative to ensure that critical mental health services needed by Texans are available.
HB 1 (ZERWAS/NELSON) GENERAL APPROPRIATIONS TO HHSC FOR MENTAL HEALTH AND SUBSTANCE USE FUNDING
HB 1 funding for mental health and substance use supports and services administered by HHSC are allocated in Article II of the state’s budget. Additional funding information can be found in the Funding section of this guide. The legislature made a number of decisions to improve access to mental health and substance use services. Some highlights include:
- An appropriation to reduce waiting lists for mental health community-based services (Rider 20);
- An appropriation to maintain a mental health peer support re-reentry program (Rider 57);
- An increase in funds to women and children’s substance use treatment services (Rider 64);
- Funding to increase the number of RTC beds available to avoid child relinquishment due to the needs of intensive mental health services (Rider 65);
- Continued funding of grants created through HB 13 (85th, Price/Schwertner) and SB 292 (85th, Huffman/Price) focused on mental health supports and services for communities and justice-involved individuals; and
- Continued funding for clubhouses across the state (Rider 65).
SB 500 (NELSON/ZERWAS) – SUPPLEMENTAL APPROPRIATIONS TO HHSC
SB 500 appropriated over $450 million for renovations and construction on state hospitals across the state.
SB 11 (TAYLOR/BONNEN) – TEXAS CHILD MENTAL HEALTH CONSORTIUM
SB 11 was filed to address safe and supportive schools, with mental health as one component of the legislation. It also includes provisions related to school hardening strategies and staff training on how to respond during an emergency.
Additionally, SB 10 (Nelson) was amended onto this bill through swift legislative action near the end of the legislative session. SB 10 created the Texas Children’s Mental Health Care Consortium (Consortium). The goal is to leverage institutions of higher education’s expertise and capacity to enhance collaboration between institutions, improve access to behavioral health care for youth, and address the youth psychiatric workforce shortage. The bill creates four major initiatives: Child Psychiatry Access Network (CPAN), the Texas Child Access Through Telemedicine (TCHATT), Child Psychiatry Workforce Expansion, and Child and Adolescent Psychiatry Fellowship. To implement and establish the initiatives, the Texas Legislature appropriated $99 million.
More details on SB 11 and other school mental health legislation can be found in The TEA Section of this guide, and The Hogg Foundation’s School Climate Legislation from the 86th Legislative Session brief found at https://hogg.utexas. edu/wp-content/uploads/2020/01/FINAL_86th-Lege_Policy-Brief_School-Climate. pdf.
HB 253 (FARRAR/KOLKHORST) POSTPARTUM DEPRESSION STRATEGIC PLAN
HB 253 directs HHSC to create develop and implement a five-year strategic plan to improve access to postpartum depression (PPD) screening, referral, treatment, and support services. The strategic plan is required to include strategies to:
- Increase awareness among state-administered program providers who may serve women who are at risk of or are experiencing PPD about the prevalence and effects of PPD on outcomes for women and children;
- Establish a referral network of community-based mental health providers and support services addressing PPD;
- Increases women’s access to formal and informal peer support services, including access to certified peer specialists who have received additional training related to PPD;
- Raise public awareness of and reduce the stigma related to PPD; and
- Leverage sources of funding to support existing community-based PPD screening, referral, treatment, and support services.
SB 633 (KOLKHORST/LAMBERT) TEXAS ALL ACCESS PROJECT
SB 633 directs HHSC to create regional authority groups of local mental health authorities serving populations of less than 250,000 in order to increase access to mental health services. HHSC is required to develop a mental health services development plan for each local mental health authority group that will increase the capacity in the group to provide access to needed services. The plans are required to focus on reducing the costs of mental health crisis services, transportation costs for those served by the local authorities to mental health facilities, incarceration of individuals with mental illnesses in county jails, and hospital emergency room visits for individuals with mental illnesses.
SB 670 (BUCKINGHAM/PRICE) TELEHEALTH INITIATIVES
SB 670 requires HHSC to encourage health care providers and health care facilities to provide telemedicine medical services and telehealth services, including mental health and substance use services. Requires HHSC to implement a number of changes to ensure that Medicaid managed care organizations reimburse for telemedicine and telehealth services at the same rate as in-person services.
SB 750 (KOLKORST/BUTTON) HEALTHY TEXAS WOMEN’S PROGRAM
SB 750 contains many provisions aimed at improving health care services for women in both the state Medicaid program and the Healthy Texas Women Program, including:
- Prenatal care and postpartum care;
- Both physical health care and behavioral health care services including requiring HHSC to develop statewide initiatives to improve the quality of maternal health care services and outcomes for women in Texas;
- A study to assess the feasibility of providing Healthy Texas Women Program services through managed care; and
- Mental health and substance use services, including provisions for HHSC:
- To apply for federal funding to implement a model of care that improves the quality and accessibility of care for pregnant women with opioid use conditions during the prenatal and postpartum periods, and their children after birth; and
- To develop and implement a postpartum depression treatment network for women enrolled in either program in collaboration with Medicaid managed care organizations.
SB 1177 (KOLKHORST/ROSE) “INLIEUOF” MEDICAID BILL
SB 1177 instructs HHSC to update Medicaid managed care contracts to include language permitting an MCO to offer medically appropriate, cost-effective, and evidence-based services from a list approved by the state Medicaid managed care advisory committee “in lieu of” mental health or substance use conditions services specified in the state Medicaid plan.
HB 2813 (PRICE/NELSON) STATEWIDE BEHAVIORAL HEALTH COORDINATING COUNCIL
HB 2813 establishes the statewide behavioral health coordinating council for a strategic statewide approach to behavioral health services. The bill codifies the council’s requirement to develop and monitor the implementation of a five-year behavioral health strategic plan, develop a biennial expenditure report, and publish an inventory of state-funded services and programs.
HB 3980 (HUNTER/MENENDEZ) SUICIDE PREVENTION EFFORTS ACROSS STATE SYSTEMS
HB 3980 directs HHSC and DSHS to publish a report on the prevalence of suicide in Texas and prevention efforts across state systems and agencies, including:
- Available state and regional data of the prevalence of suicide-related events, including thoughts, attempts, and deaths caused by suicide. Data is disaggregated by county and is longitudinal as able;
- Identification of the highest categories of risk with correlational data;
- State statutes, agency rules, and policies related to suicide prevention, intervention, and postvention; and
- Agency initiatives since 2000 addressing suicide, including funding sources and years of operations.
Additionally, HB 3908 directs the Statewide Behavioral Health Coordinating Council to establish a stakeholder workgroup to assist in preparing a legislative report. The report is required to identify opportunities and make recommendations to improve statewide data collection related to suicide, to use data to guide and inform decisions and policy development, and to decrease suicides while targeting the highest risk categories.
HB 3285 (SHEFFIELD/HUFFMAN) OMNIBUS SUBSTANCE USE BILL
HB 3285 is a comprehensive bill addressing substance use across a number of agencies. While the bill addresses various initiatives, the following are brief descriptions of a few changes requiring HHSC or DSHS involvement. This is not a complete summary of the provisions of the bill:
- Requires the executive commissioner of HHSC to establish a program that increases opportunities and expands access to telehealth treatment for substance use across Texas;
- Requires the Statewide Behavioral Health Strategic Plan to include a subplan for substance use issues;
- Requires DSHS to create an opioid misuse public awareness campaign;
- Requires the executive commissioner of DSHS to ensure the data collection of opioid overdose deaths, co-occurrence of substance use and mental illness, and evaluation of the current treatment capacity for individuals with co-occurring substance use and mental health concerns; and
- Requires Medicaid reimbursement for medication-assisted treatment (MAT) without prior authorization or pre-certification, with the exception of methadone.
Funding
HHSC funding continues to be a major component of the State of Texas biennial budget comprising approximately 30 percent of the total budget for the FY 2020- 21 biennium.27 Mental health and substance use funding has historically been underfunded, including reimbursement rates for providers. This impacts provider willingness to participate in the state Medicaid program which in turn directly impacts access to services. The Texas Legislature has increased mental health funding over the last several biennia, but many programs and services remain underfunded. In the most recent budget, Texas increased substance use funding, however was only a small fraction of HHSC’s request, and was the first increase in the last decade.
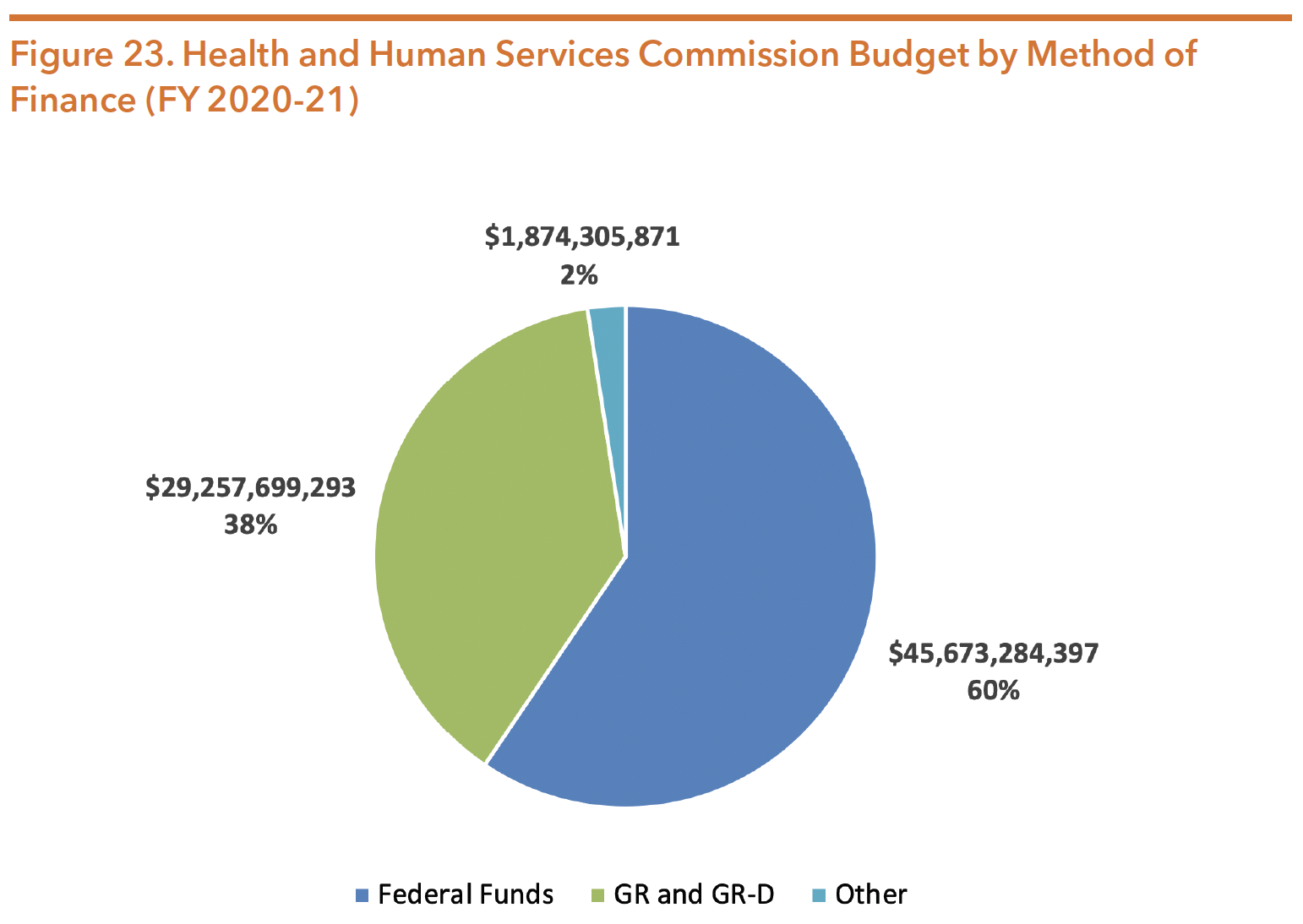
Source: Texas Legislature Online (2019). H.B.1, General Appropriations Act, 86th Legislature, FY 2020-21. Retrieved from https://capitol.texas.gov/tlodocs/86R/billtext/pdf/HB00001F.pdf#navpanes=0
Table 15 below shows the HHSC All Funds funding trends over the last three budget cycles.
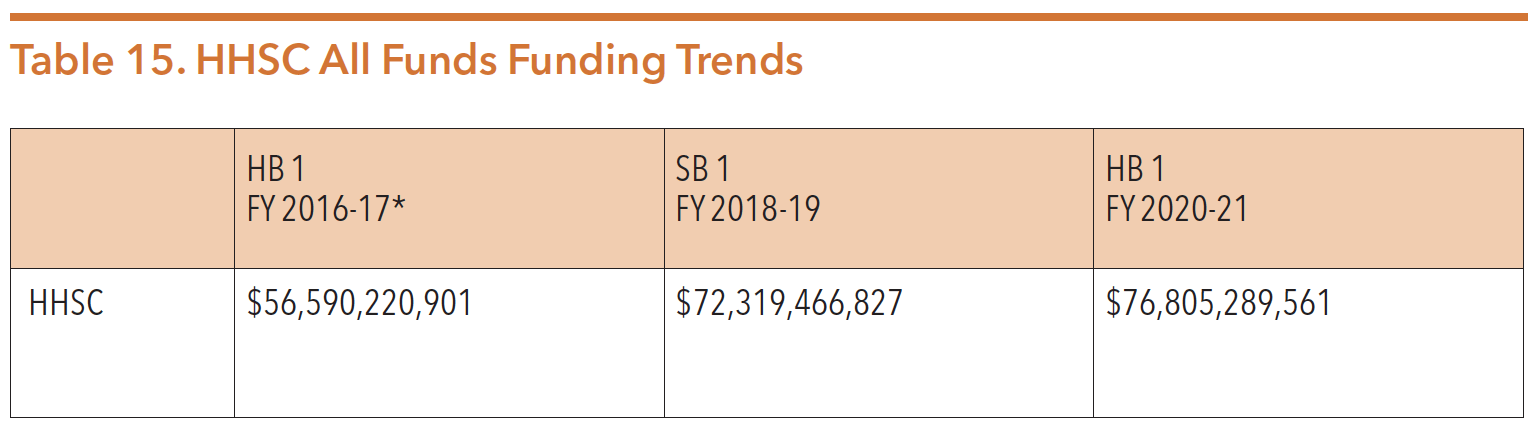
*Note: this amount was prior to the Health and Human Services System Transformation and consolidation of state agencies
Sources: Texas Legislature Online (2019). H.B.1, General Appropriations Act, 86th Legislature, FY 2020-21. Retrieved from https:// capitol.texas.gov/tlodocs/86R/billtext/pdf/HB00001F.pdf#navpanes=0
Texas Legislature Online (2017). S.B.1, General Appropriations Act, 85th Legislature, FY 2018-19. Retrieved from https://capitol.texas.gov/tlodocs/85R/billtext/pdf/SB00001F.pdf#navpanes=0
Texas Legislature Online (2015). H.B.1, General Appropriations Act, 84th Legislature, FY 2016-17. Retrieved from https://capitol.texas.gov/tlodocs/84R/billtext/pdf/HB00001F.pdf#navpanes=0
HHSC Advisory Committees
After the Sunset Commission reviewed all Health and Human Services advisory committees, the continuing committees were re-established in rule; a list is available on the HHSC website at https://hhs.texas.gov/about-hhs/leadership/ advisory-committees.
Several of the continuing committees have a direct impact on mental health and substance use policies, including but not limited to:
- Behavioral Health Advisory Committee
- Drug Utilization Review Board
- E-Health Advisory Committee
- Early Childhood Intervention Advisory Committee
- Medical Care Advisory Committee
- Policy Council for Children and Families Committee
- STAR Kids Managed Care Advisory Committee
- State Medicaid Managed Care Advisory Committee
- Texas Autism Council
- Texas Council on Consumer Direction
- Texas School Health Advisory Committee
HHS Regions
For service delivery administration, the state is divided into 11 HHS regions, displayed in Figure 24. As of August 2019, the HHS system employed over 36,346 full-time employees.
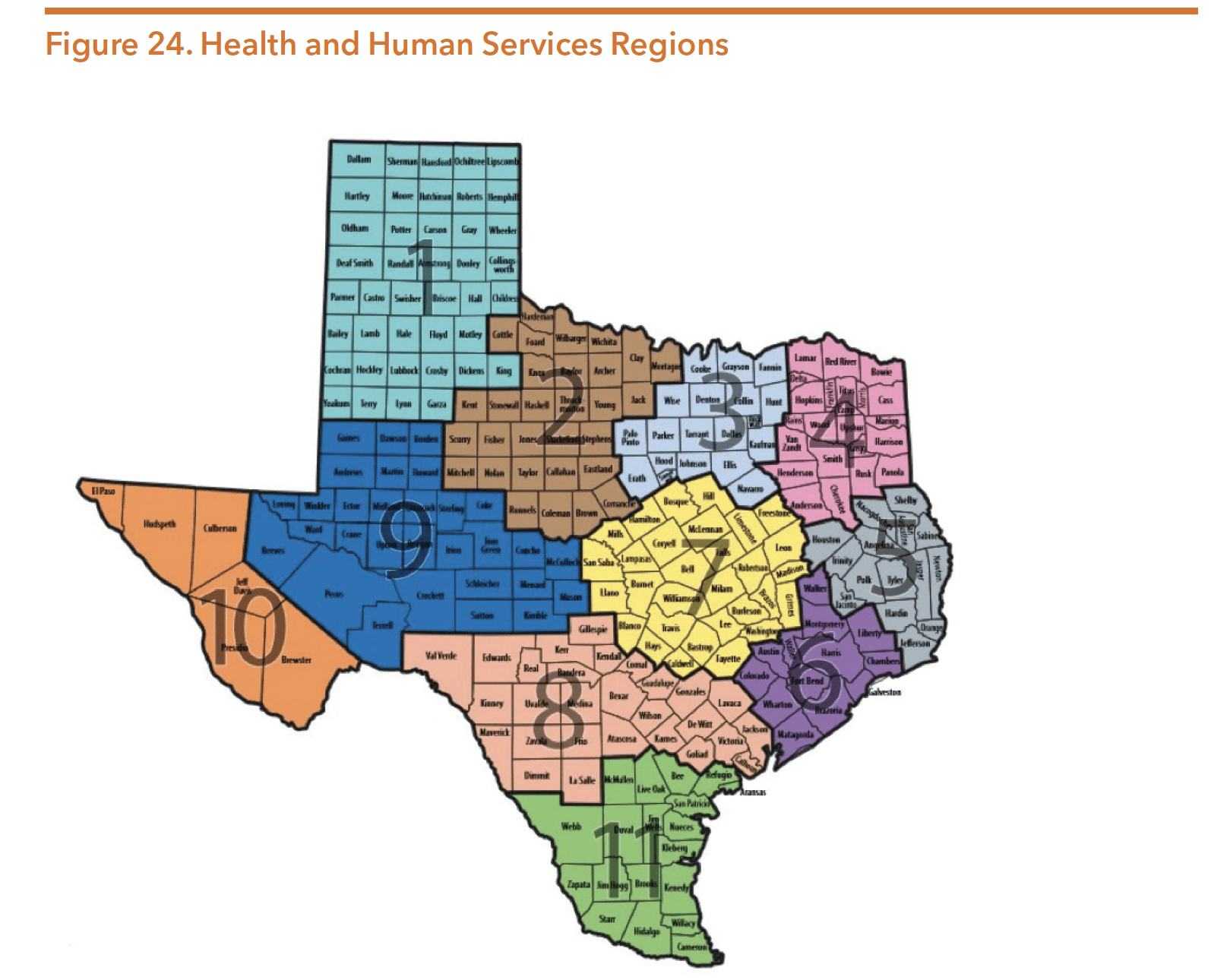
Source: Texas Health and Human Services Commission. (2016). Health and Human Services offices by county. Retrieved from https://hhs.texas.gov/sites/default/files/documents/about-hhs/hhs-regional-map.pdf
Medical and Social Services Division
The Medical and Social Services Division is responsible for:
- Medicaid and CHIP Services
- IDD and Behavioral Health Services Division
- Health, Developmental & Independence Services Division
- Access and Eligibility Services
OFFICE OF MENTAL HEALTH COORDINATION
In recent years, mental health and substance use (often referred to as “behavioral health”) have become major topics of both state and national dialogue. The Texas Legislature took steps to increase and improve cross-agency planning, coordination, and collaboration in effort to be more strategic with behavioral health service delivery and funding. In 2013, the legislature created the Office of Mental Health Coordination tasked with providing broad oversight for state mental health policy as well as managing cross-agency coordination of behavioral health programs, services, and expenditures. The office reports directly to the deputy executive commissioner for IDD & Behavioral Health Services. The office developed a website to provide consumers, families, and providers with up-to-date information on mental health and substance use programs and services. More information is available at http:// www.mentalhealthtx.org.
STATEWIDE BEHAVIORAL HEALTH COORDINATING COUNCIL
In 2015, the legislature established the Statewide Behavioral Health Coordinating Council (SBHCC). The HHSC assistant commissioner, who oversees the Office of Mental Health Coordination at HHSC, serves as chair of the council.30 Agencies and departments work together under the direction of the Office of Mental Health Coordination to ensure a strategic statewide approach to behavioral health services. During the 86th legislative session, Texas lawmakers passed House Bill 2813 (Price/ Nelson), codifying the SBHCC. While other state agencies or institutions may be authorized to serve on the SBHCC, the agencies required to be represented are:
- Texas Health & Human Services Commission
- Office of the Texas Governor
- Texas Veterans Commission
- Texas Department of State Health Services
- Texas Department of Family and Protective Services
- Texas Civil Commitment Office
- University of Texas Health Science Center at Houston
- University of Texas Health Science Center at Tyler
- Texas Department of Criminal Justice
- Texas Correctional Office on Offenders with Medical or Mental Impairments
- Texas Juvenile Justice Department
- Texas Military Department
- Texas Health Professions Council (includes six member agencies)
- Texas Education Agency
- Texas Tech University System
- Texas Commission on Jail Standards
- Texas Workforce Commission
- Texas Department of Housing and Community Affairs
- Texas Indigent Defense Commission
- Texas Court of Criminal Appeals
The SBHCC is responsible for developing and implementing the five-year Statewide Behavioral Health Strategic Plan, a biennial Coordinated Statewide Expenditure Proposal, and publishing an annual inventory of behavioral health programs funded by the state. The Coordinating Council also has a number of goals, and coordinating agencies collaborate on a number of activities shown in Figure 25.
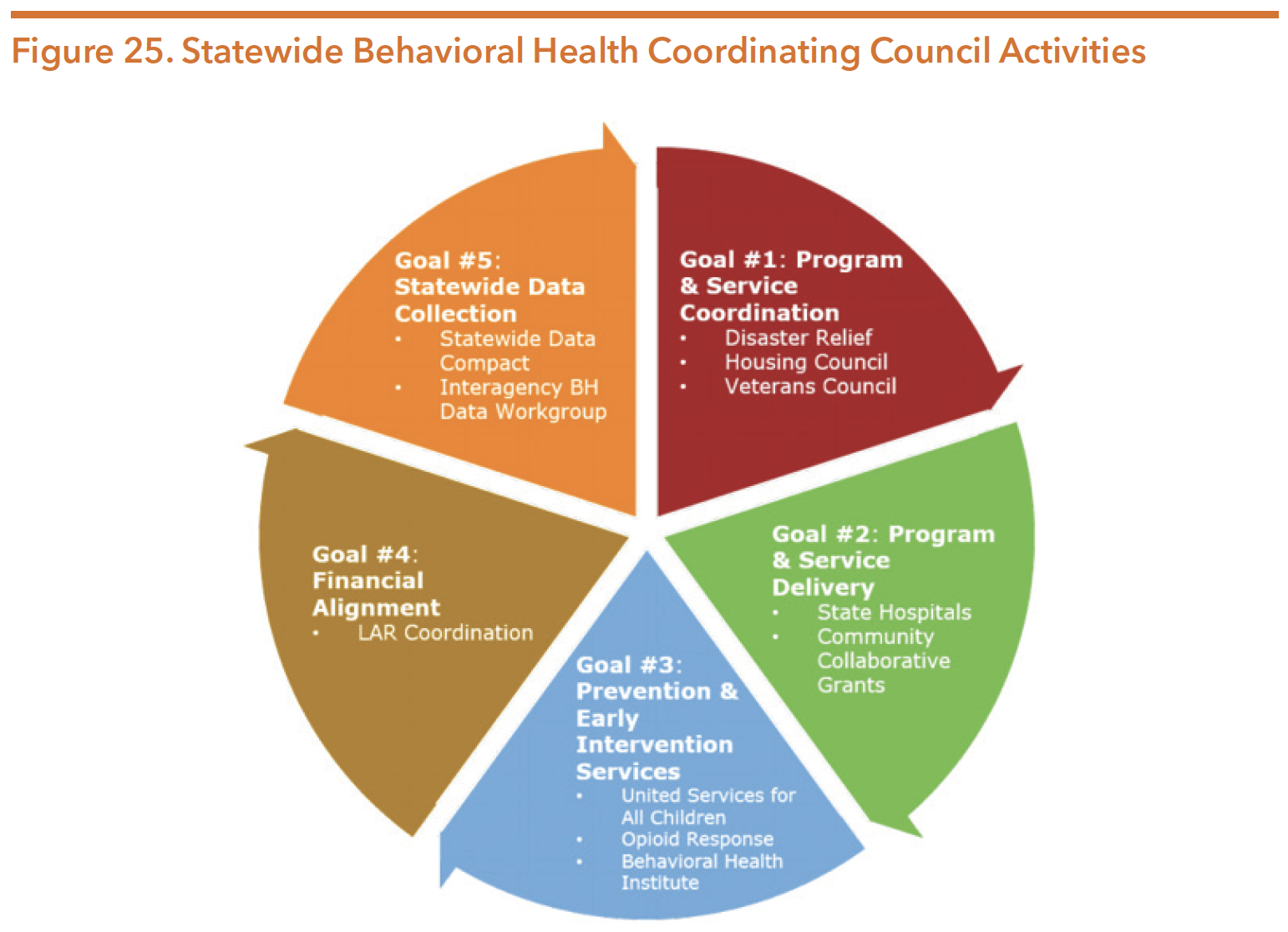
Source: Texas Health and Human Services Commission. (March 2018). Presentation to the Senate Finance Committee: Statewide Behavioral Health Coordinating Council. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2018/leg-presentations/senate-finance-hearing-march-20-2018.pdf
THE STATEWIDE BEHAVIORAL HEALTH STRATEGIC PLAN
The Statewide Behavioral Health Strategic Plan identifies 15 primary gaps in behavioral health services in Texas. The plan’s framework and goals are intended to address gaps and challenges within the behavioral healthcare system, as well as improve access to care and outcomes. The second edition of the plan is available at https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2019/hb1-statewide-behv-hlth-idd-plan-feb-2019.pdf
The most recent progress report as of September 2020 was printed in December 2019 and is available at https://hhs.texas.gov/reports/2019/12/ texas-statewide-behavioral-health-strategic-plan-progress-report-fiscal-year-2019
Chairwoman Jane Nelson has indicated that any legislative proposals directed toward behavioral health should address one or more of these identified gaps. The gaps include:
- Access to appropriate behavioral health services
- Behavioral health needs of public school students
- Coordination across state agencies
- Veteran and military service members supports
- Continuity of care for individuals exiting county and local jails
- Access to timely treatment services
- Implementation of evidence-based practices
- Use of peer services
- Behavioral health services for individuals with intellectual disabilities
- Consumer transportation and access to treatment
- Prevention and early intervention services
- Access to housing
- Behavioral health workforce shortage
- Services for special populations
- Shared and usable data
As a result of the passage of HB 3285 (Sheffield/Huffman), SBHCC is required to create a subplan specifically addressing substance use, including:
- Addressing challenges of existing prevention, intervention, and treatment programs;
- Evaluation of substance use conditions prevalence;
- Identifying substance use treatment services availability and gaps; and
- Collaborating with state agencies to expand substance use treatment service capacity in the state
According to HHSC, as of August 2020, the agency has organized an internal workgroup with plans to engage stakeholders moving forward. The development of the substance use subplan will be developed in tandem with the full Statewide Behavioral Health Strategic Plan to be due December 2021.
THE COORDINATED STATEWIDE BEHAVIORAL HEALTH EXPENDITURE PROPOSAL
The SBHCC develops the Coordinated Statewide Behavioral Health Expenditure Proposal. The proposal identifies the total behavioral health funding proposed by each agency for the upcoming fiscal year. Expenditures are linked to various strategies in the strategic plan to demonstrate how state appropriations will be used to further its goals during the fiscal year. The full proposal is available at https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2019/hb1-behavioral-health-expenditure-proposal-fy20.pdf
HHSC compiles a consolidated report of behavioral health funding across agencies, a summary of which can be found in the funding section of this guide.
VETERAN SERVICES DIVISION
The Veteran Services Division within HHSC was created in 2013 to coordinate, strengthen, and enhance veteran services across state agencies. The division’s focus is to review and analyze current programs, engage the charitable and nonprofit communities, and create public-private partnerships to benefit these programs. The Veterans Services Division is an active participant in the Texas Coordinating Council for Veterans Services. The HHS Enterprise offers Texas veterans services through several agencies including but not limited to the Department of State Health Services, Texas Veterans Commission (TVC), and Texas Workforce Commission. More information on veterans can be found in the TVC section of this guide.
Medicaid & CHIP Service
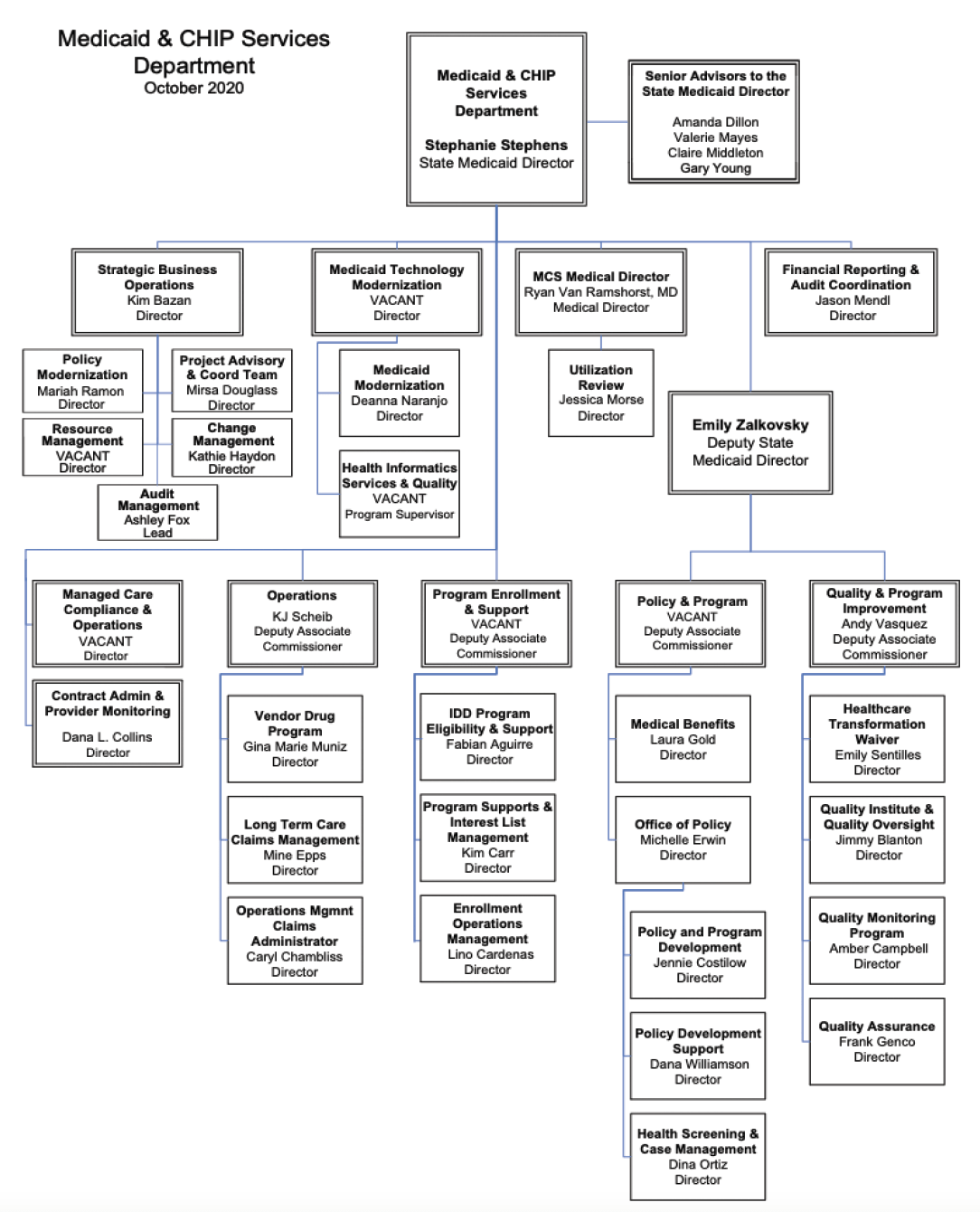
Source: Texas Health and Human Services Commission. (October 2020). Public Information Request, October 2020.
MEDICAID
Medicaid is a jointly funded federal and state health care program authorized in Title XIX of the Social Security Act. It was created to provide health care benefits primarily to children in low-income families, pregnant women, and people with disabilities. The Texas Medicaid Program was first established in Texas in 1967. In January 2020, total Texas Medicaid and CHIP enrollment was 3,870,036 with 3,176,504 child enrollees.
Medicaid is an entitlement program, meaning that anyone who meets the eligibility criteria has a right to receive needed services and cannot be placed on waiting lists. Medicaid primarily serves low-income individuals who meet certain financial and non-financial criteria to be eligible for services. Neither the federal government nor states can currently limit the number of eligible persons who enroll in the program.
The federal government defines the mandatory services that state Medicaid programs must provide and required eligible populations. States have the option to expand both the services offered and eligible populations through State Plan Amendments (SPAs), Medicaid waivers, and the Affordable Care Act (ACA). As of September 2020, 38 states and Washington, D.C. have adopted Medicaid expansion. Texas is one of 12 states that has chosen not to adopt this expansion. As federal requirements and state policies change over time, updates are made via SPAs. States can choose to submit SPAs to make changes to their programs; for example, to change a provider payment methodology or add coverage of an optional service. States can also make programmatic and eligibility changes by participating in Medicaid waiver programs to waive basic federal Medicaid requirements. Waivers can allow flexibility with mandated eligibility or required benefits in order to develop service delivery alternatives that improve cost efficiency or service quality. States can participate in three types of Medicaid waivers:
- Research and Demonstration 1115 Waivers give the state leniency to experiment with new service delivery models.
- Freedom of Choice 1915(b) Waivers allow the state to require clients to enroll in managed care plans and use the cost savings to enhance the Medicaid benefits package.
- Home and Community-based Services 1915(c) Waivers allow the state to provide community-based services to individuals who would otherwise be eligible for institutional care.
STATE MEDICAID AGENCY
HHSC has been the designated state Medicaid agency since 1993, administering the program and acting as a liaison between Texas and the federal government on related issues. The federal government establishes most Medicaid guidelines but grants several important tasks to the states, including:
- Administering the Medicaid State Plan, which functions as the contract between the agency and the federal government;
- Establishing Medicaid policies, rules, and provider reimbursement rates; and
- Establishing eligibility beyond the minimum federal eligibility groups
MEDICAID MANAGED CARE
Since the early 1990s, Texas has offered Medicaid coverage through two service models: fee-for-service (FFS) and managed care. In a traditional FFS model, providers receive payment for each individual service delivered. The FFS model is now limited to very few Medicaid participants, primarily those who are dually eligible for Medicaid and Medicare. As of November 2019, approximately 94.4 percent of Medicaid services in Texas were provided through managed care. In a Medicaid managed care system, individuals access services through a Managed Care Organization (MCO), also known as a health plan. HHSC contracts with MCOs and pays them a monthly amount (capitated rate) per Medicaid enrollee to coordinate health services for each member enrolled in their health plan. All CHIP services are delivered through managed care.
MCOs are responsible for creating a network of public and private providers to ensure that adults and children receiving Medicaid can access needed services. MCOs are responsible for service authorization and reimbursement to service providers. With support from the Medicaid 1115 Transformation Waiver, Texas has incrementally expanded its Medicaid managed care system to include more services and populations.
In a managed care system, the Medicaid member selects a health plan and identifies a primary care physician from that plan’s provider network. Individuals have a choice between two or more health plans in each HHS service region. Members have the option to change plans if they are unsatisfied. In addition to contractual requirements and state monitoring, members’ ability to switch plans generates some level of competition between health plans that is intended to result in higher quality services.
Managed care programs in Texas include:
- STAR: serves children, newborns, pregnant women, and some families and children;
- STAR+PLUS: serves individuals with a disability and who are older than 65 (including those with dual eligibility for Medicare), and women with breast or cervical cancer;
- STAR HEALTH: serves children who receive Medicaid through DFPS and former foster care youth;
- STAR Kids: serves children and young adults 20 years of age and younger with a disability; and
- CHIP: serves children in families who do not meet income requirements for Medicaid, but who are unable to afford private health insurance.
Recently, more Texas Medicaid clients have enrolled in managed care, an increase from 86 percent in 2016 to approximately 94 percent in July 2019. This is in large part due to the implementation of SB 7 (83rd, Nelson/Raymond), which expanded mandatory participation in the existing STAR+PLUS managed care program beginning in September 2013. STAR+PLUS is specifically for people who have disabilities or are age 65 or older. People in STAR+PLUS get Medicaid healthcare and long-term services and support.
Senate Bill 7 directed the design and implementation of a comprehensive system of acute care and long-term services and supports for adults and children, including those with disabilities. The bill generated immediate system delivery changes in Medicaid by expanding STAR+PLUS to serve all areas of the state, as well as transitioning nursing facility services and acute care services for individuals with IDD into STAR+PLUS.
Many of the changes instituted by SB 7 address coverage for individuals with IDD, who are three times more likely to experience a mental health condition than the general population. To advise HHSC through the system redesign of transitioning long-term services and supports (LTSS) to Medicaid managed care, the IDD System Redesign Advisory Committee was created. More information on the advisory committee can be found at https://hhs.texas.gov/about-hhs/leadership/advisory-committees/ intellectual-developmental-disability-system-redesign-advisory-committee.
Between 2014 and 2016, HHSC completed the transition of acute services from Medicaid FFS to STAR+PLUS, STAR Kids, and STAR Health managed care programs for all eligible recipients of Medicaid IDD waiver programs and intermediate care facilities (ICFs) for individuals with IDD. STAR Kids provides Medicaid managed care to children and adults 20 and younger who have disabilities, while STAR Health provides services for children and youth in the foster care system, including youth up to age 26 who have aged out of care.
In early 2019, HHSC completed and published evaluations to inform managed care on the transition of LTSS to managed care for individuals with IDD. Prior to the 86th legislative session, SB 7 required these services to be provided through managed care by 2020-21. However, HB 4533 (Klick/Kolkhorst) passed, extending the transition timeframe for TxHmL to 2027, CLASS to 2029, and HCS and DBMD to 2031. Additionally, HB 4533 requires HHSC to establish a pilot program prior to the transition, as well as establishes a Pilot Program Workgroup to provide assistance in developing and advising HHSC on the operation of the pilot program.
In addition to expanding care in STAR+PLUS, SB 7 established a new managed care program for children with disabilities called STAR Kids which launched in November 2016. Figure 26 depicts the growth of Medicaid managed care in Texas from 2000 through 2017.
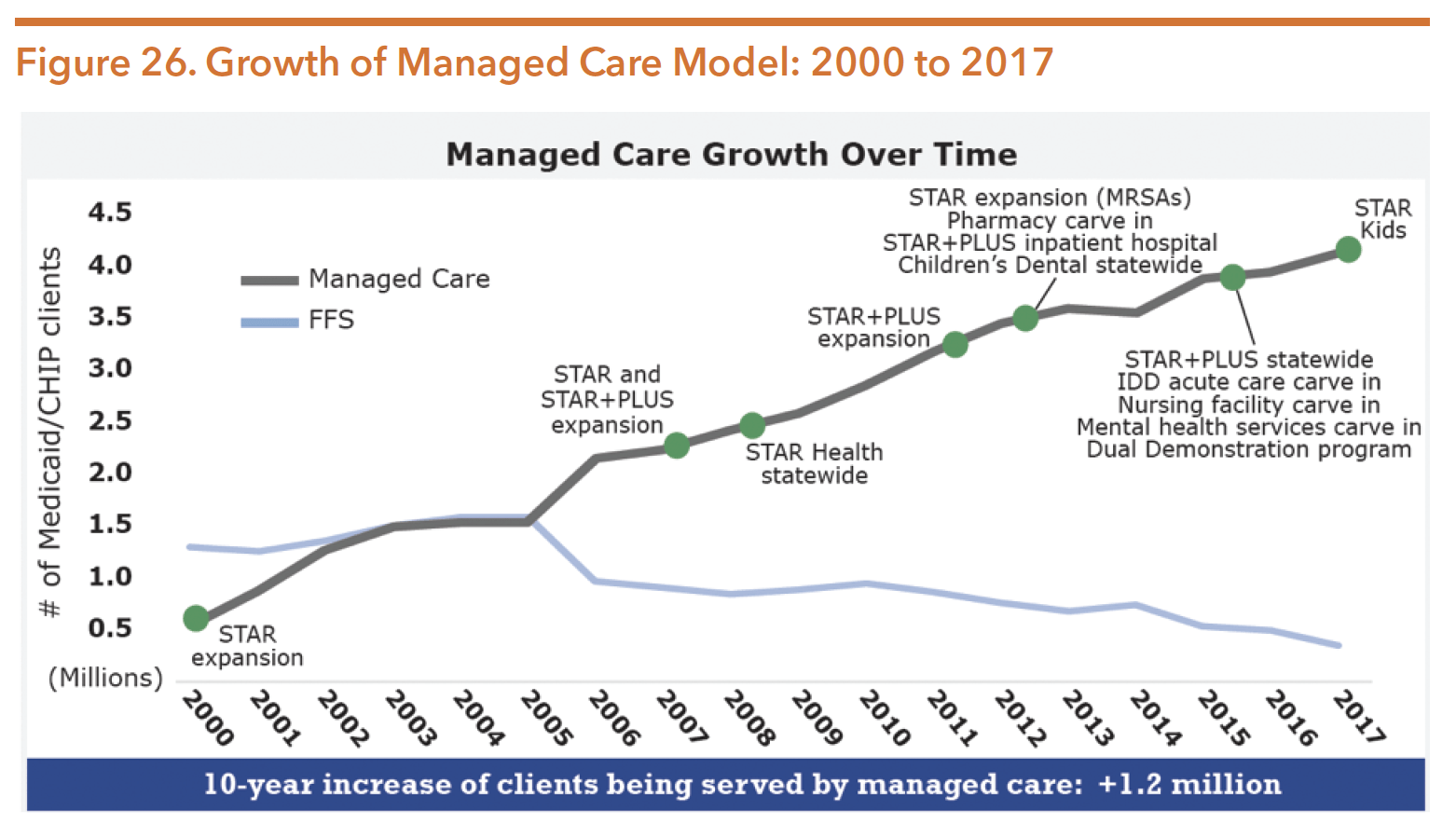
Source: Texas Health and Human Services Commission. (2018). Texas Medicaid and CHIP in perspective twelfth edition. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2018/ medicaid-chip-perspective-12th-edition/12th-edition-complete.pdf
Table 16 describes the four Texas Medicaid and the CHIP managed care programs.
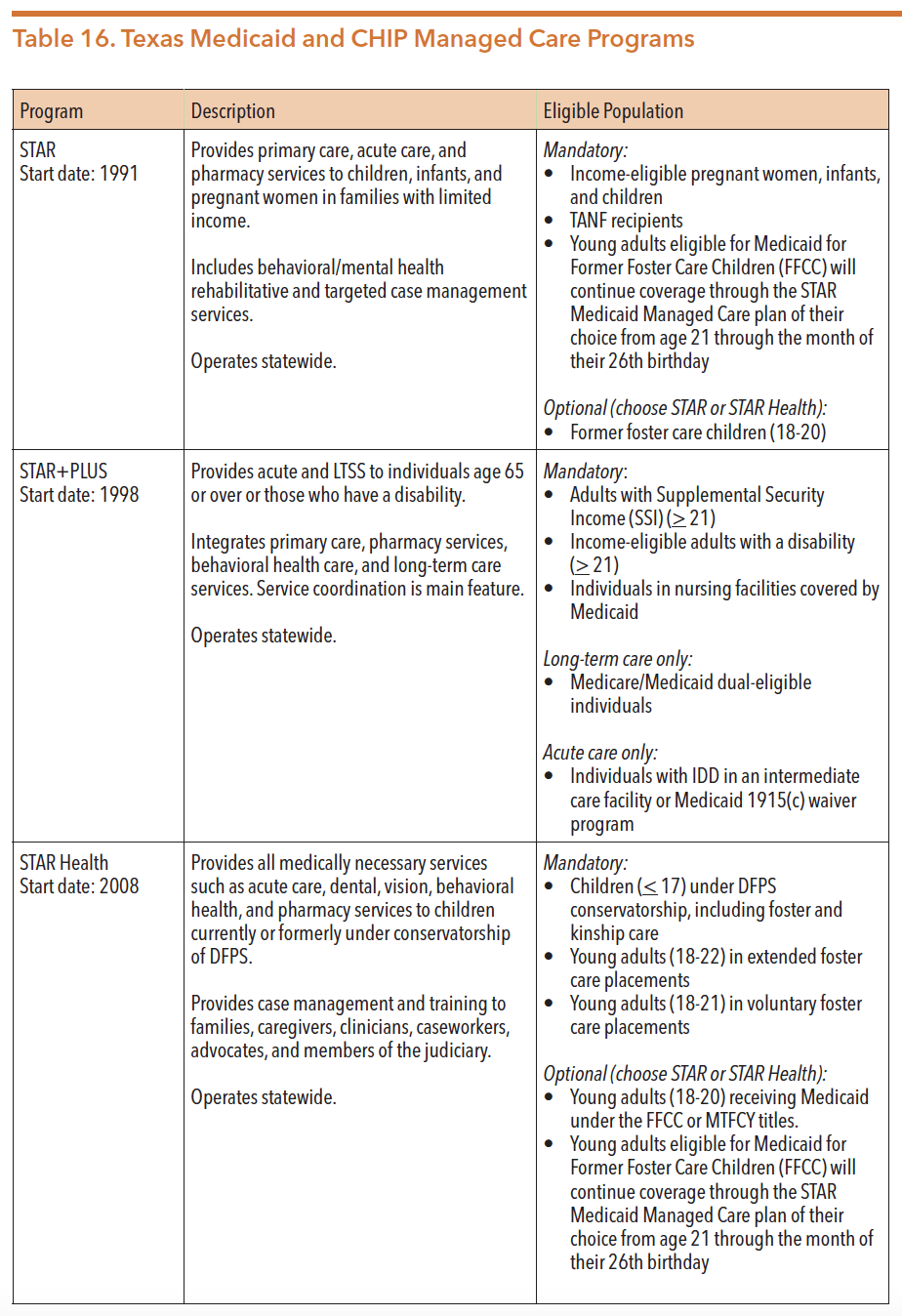
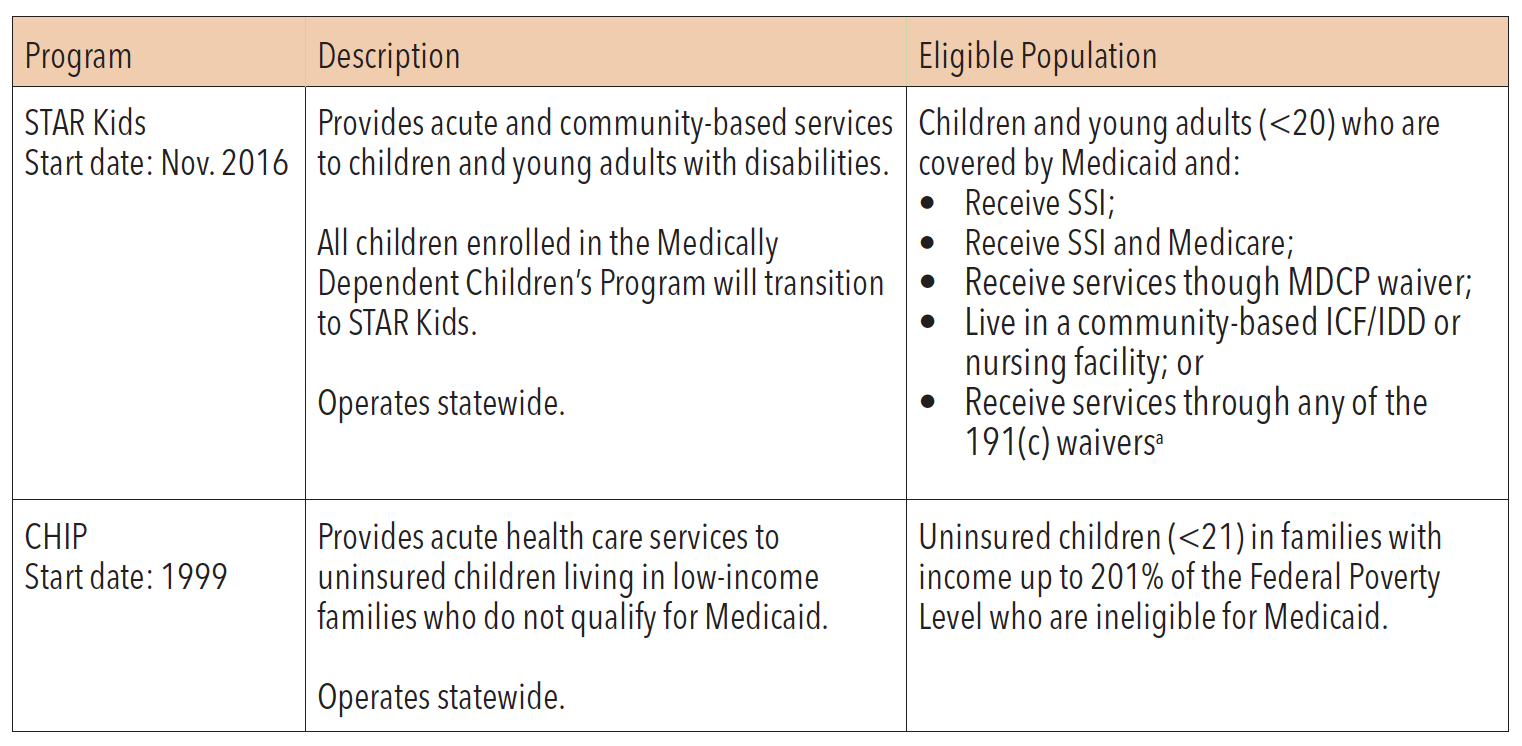
*Medicaid 1915(c) waiver programs for adults and children include Home and Community-based Services (HCS), Community Living Assistance & Support Services (CLASS), Texas Home Living (TxHmL), and Deaf Blind with Multiple Disabilities (DBMD). Youth Empowerment Services (YES) serves children and youth.
Sources: Institute for Child Health Policy at the University of Florida. (2016). Texas Medicaid managed care and Children’s Health Insurance Program, summary of activity and trends in healthcare quality, Contract Year 2016. Retrieved from https://hhs.texas. gov/sites/default/files/documents/about-hhs/process-improvement/quality-efficiency-improvement/ External-Quality-Review/tx-medicaid-mngd-care-chip-eqro-contract-yr-2016.pdf
Texas Department of Family and Protective Services. (n.d.). STAR Health – a guide to medical services at CPS. Retrieved from https:// www.dfps.state.tx.us/Child_Protection/Medical_Services/default.asp
Texas Health and Human Services Commission. (n.d.). STAR+PLUS. Retrieved from https://hhs.texas.gov/services/health/ medicaid-chip/programs/starplus
Texas Health and Human Services Commission. (n.d.) STAR+PLUS expansion. Retrieved from https://hhs.texas.gov/services/ health/medicaid-chip/provider-information/expansion-managed-care/starplus-expansion
Texas Health and Human Services Commission. (n.d.). STAR Kids. Retrieved from https://hhs.texas.gov/services/health/ medicaid-chip/programs/star-kids
Texas Health and Human Services Commission. (n.d.). Medicaid Managed Care quality strategy 2012-2016. Retrieved from http://texasrhp9.com/uploads/public/documents/Texas%20Medicaid%20Managed%20Care%20Quality%20 Strategy%202012-2016.pdf
Traylor, C. & Ghahremani, K. (August, 2014). Presentation to the Senate Health and Human Services Committee: SB 7 implementation. Texas Health and Human Services Commission. Retrieved from https://hhs.texas.gov/reports/2014/08/ presentation-senate-health-and-human-services-committee-sb-7-implementation
Texas Health and Human Services Commission. (2017). Texas Medicaid and CHIP in perspective eleventh edition. Retrieved from https://hhs.texas.gov/sites/default/files//documents/laws-regulations/reports-presentations/2017/ medicaid-chip-perspective-11th-edition/11th-edition-complete.pdf
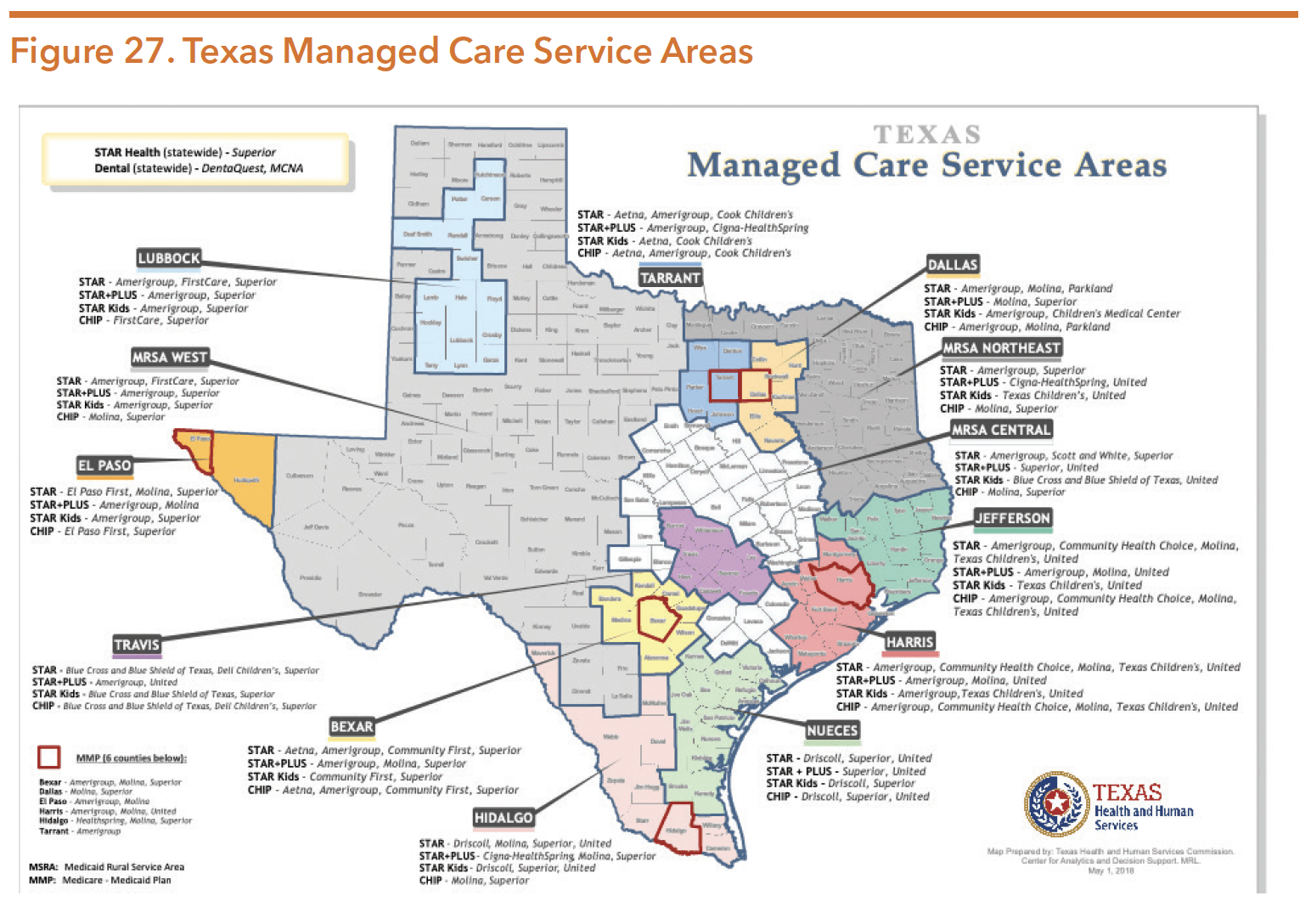
Eighteen MCOs and two dental maintenance organizations (DMOs) provide services to Texas Medicaid and CHIP enrollees. Texas administers services in STAR, STAR+PLUS, STAR Kids, and CHIP in 13 service areas across the state illustrated in Figure 27.
Source: Texas Health and Human Services Commission. (December 2019). Annual report on quality measures and value-based payments. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/ reports-presentations/2019/hb-1629-quality-measures-value-based-payments-dec-2019.pdf
MEDICAID FUNDING
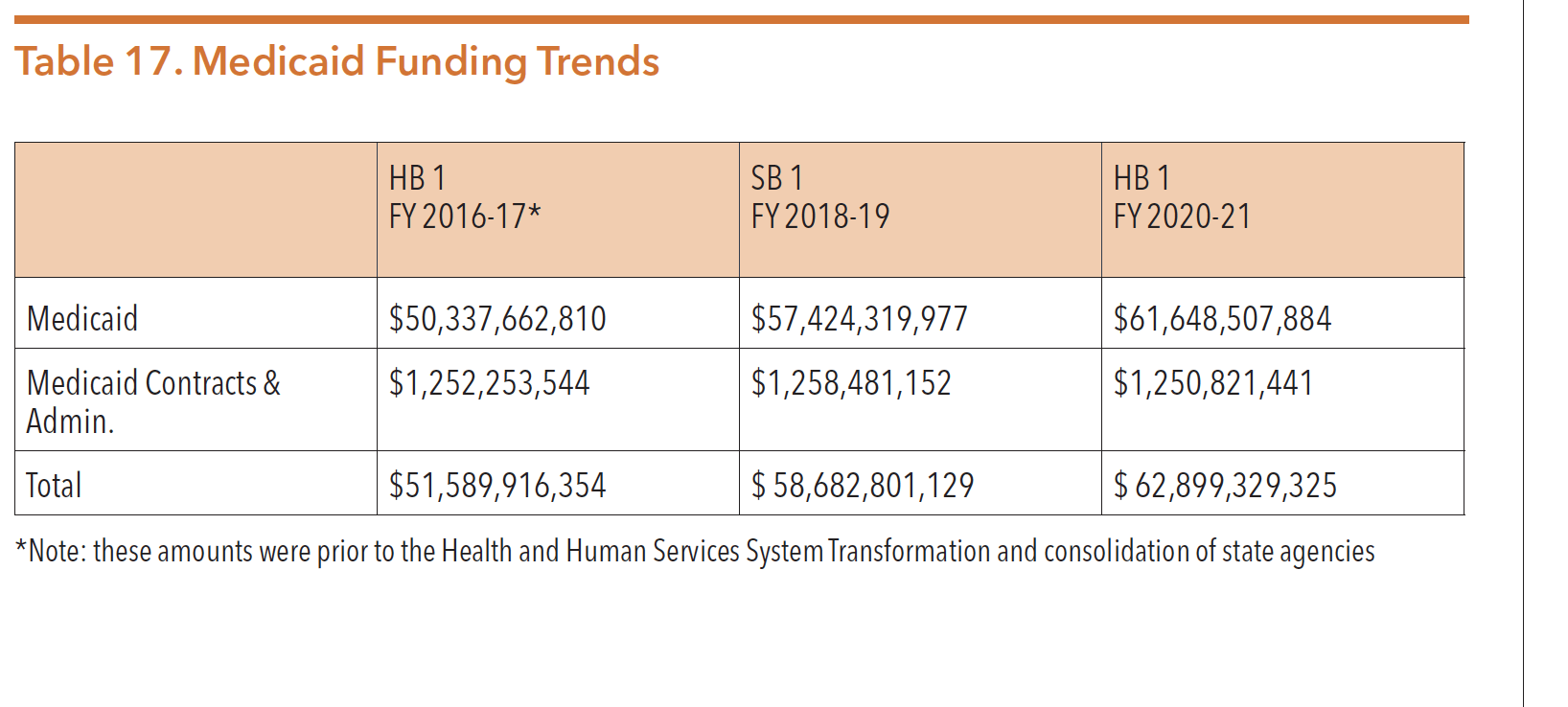
The Texas Medicaid program is jointly funded by the state and the federal government. Medicaid is the largest source of public funding for mental health services nationwide, comprising a quarter of all public behavioral health expenditures.
Table 17 below shows Medicaid funding trends over the last three budget cycles.
Sources: Texas Legislature Online (2019). H.B.1, General Appropriations Act, 86th Legislature, FY 2020-21. Retrieved from https:// capitol.texas.gov/tlodocs/86R/billtext/pdf/HB00001F.pdf#navpanes=0
Texas Legislature Online (2017). S.B.1, General Appropriations Act, 85th Legislature, FY 2018-19. Retrieved from https://capitol.texas.gov/tlodocs/85R/billtext/pdf/SB00001F.pdf#navpanes=0
Texas Legislature Online (2015). H.B.1, General Appropriations Act, 84th Legislature, FY 2016-17. Retrieved from https://capitol.texas.gov/tlodocs/84R/billtext/pdf/HB00001F.pdf#navpanes=0
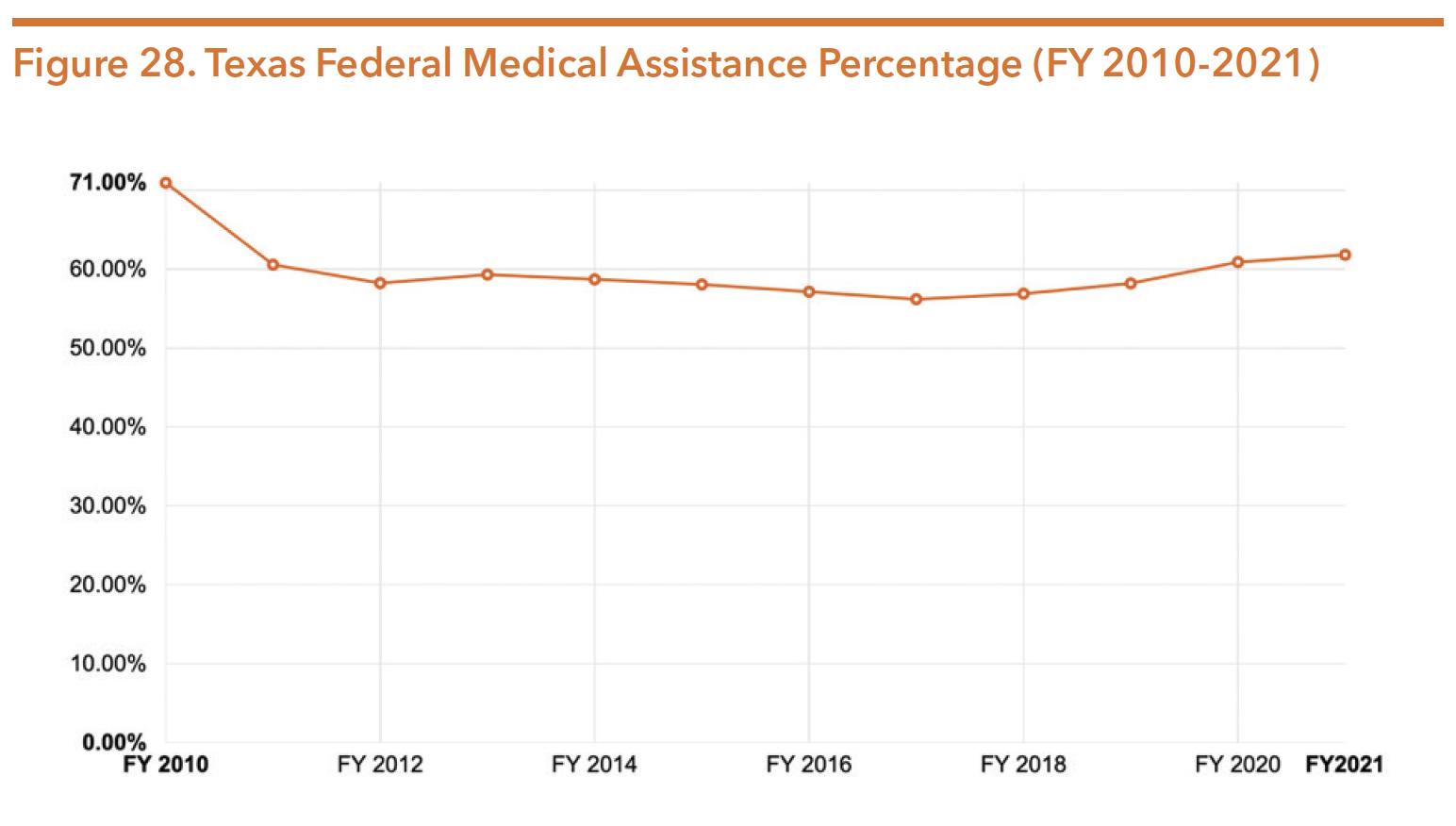
The federal share of the Medicaid program, known as the federal medical assistance percentage (FMAP), is determined on an annual basis and by a formula that takes into account each state’s income per capita compared to the U.S. average. Medicaid is one of the five grant programs administered by the U.S. Health and Human Services that uses the FMAP to determine reimbursements and payments to states.
The FMAP rate is also in-part calculated based on the U.S. Census count completed every 10 years. Small changes in the FMAP can result in millions of dollars in funding fluctuations. Anticipating the next census count to occur following the 86th legislative session, lawmakers filed bills to create a statewide census outreach committee. This initiative failed to pass, as did efforts to include dedicated funds in the budget for grants targeting local outreach efforts. In effort to address concerns from lack of coordinated state efforts, non-profit organizations, grassroots groups, and local governments have partnered on local outreach to ensure Texas has an accurate census count.49 On August 26, 2020, the Texas secretary of state’s office announced an allocation of $15 million from federal funding meant to address COVID, toward an advertising campaign to urge residents to completed the census.
On April 13, 2020, The U.S. Department of Commerce Secretary and the U.S. Census Bureau Director announced a 2020 Census operational plan adjustment due to COVID-19. The announcement stated the new plan “would extend the window for field data collection and self-response to October 31, 2020, which will allow for apportionment counts to be delivered to the President by April 30, 2021, and redistricting data to be delivered to the states no later than July 31, 2021.” However, on August 3, 2020, the Census Bureau Director released a contradictory plan stating field data collection would end by September 30, 2020.
In response, a lawsuit was filed by voting and civil rights groups, as well as local governments, challenging the Trump administration’s order to complete the census count by the end of September. On September 5, 2020, a temporary restraining order was issued by U.S. District Judge Lucy Koh which required the Census Bureau and Commerce Department to continue operations as planned until a later hearing. Despite this injunction, the Commerce Department announced an October 5th end date. As of October 2, 2020, Judge Koh directed the 2020 census counting to continue until October 31st. Additionally, she directed the Census Bureau to send all employees a text message “stating that the October 5, 2020 ‘target date’ is not operative, and that data collection operations will continue through October 31, 2020.” She cited contradictory messages from some supervisors of field employees as the reason for the wide message and that releasing an October 5th ‘target date’ violated her order.
Texas’ Medicaid federal matching rates for FY 2020 and 2021 are 60.89 percent and 61.81 percent; in other words, the state must pay 39.11 percent and 38.19 percent of all costs, respectively. In Texas, Medicaid represents over 25 percent (over $62 billion) of the state budget for 2020-2021.
To illustrate Texas’ trend of federal Medicaid funding, Figure 28 below shows Texas’ FMAP from 2004 to 2021.
Source: Kaiser Family Foundation, State Health Facts. (2020). Federal Medical Assistance Percentage (FMAP) for Medicaid and multiplier (Timeframe: FY 2010-2020).
On March 18, 2020 the federal government passed the Families First Coronavirus Response Act (FFCRA) in response to COVID-19. FFCRA immediately increased states’ FMAP percentage by 6.2 percent. This increase is expected to be active through the end of the quarter in which the federal emergency ends and was retroactively applied from January 1, 2020.57 For Texas, this increase resulted in an FMAP of 67.09 percent. In order for Texas to keep the funding, MOE provisions were required, including:
- Refrain from cutting Medicaid eligibility standards or imposing enrollment procedures that are more restrictive;
- Keep all Medicaid enrollees covered who were eligible and receiving services as of March 18, 2020 or who newly enroll during the public health emergency; and
- Cover COVID-19 testing services and treatment in Medicaid, including vaccines, specialized equipment, and therapies, without cost-sharing.
MEDICAID ELIGIBILITY
Medicaid was originally only available to recipients of cash assistance programs such as Temporary Assistance for Needy Families (TANF) and Social Security Income (SSI). However, during the late 1980s and early 1990s, the federal government decoupled Medicaid eligibility from the receipt of cash assistance and expanded the program to meet the needs of a broader population, including pregnant women, older adults, and people with disabilities.
In determining program eligibility, Texas considers a variety of factors such as income and family size, age, disability, pregnancy status, citizenship, and state residency requirements. To be eligible for Medicaid in Texas, an individual must meet income and categorical eligibility requirements. Categorical eligibility requires that beneficiaries be part of a specific population group.
There are multiple Medicaid eligibility categories in Texas. Some of the primary categories include:
- Children age 18 and under
- Pregnant women and infants
- Families receiving TANF
- Parents and caretaker relatives
- Individuals receiving SSI
- Adults over age 65 and people with disabilities
- Children and pregnant women who qualify as medically needy
- Former foster youth under 26 years old
- Individuals receiving Medicaid 1915(c) waiver services
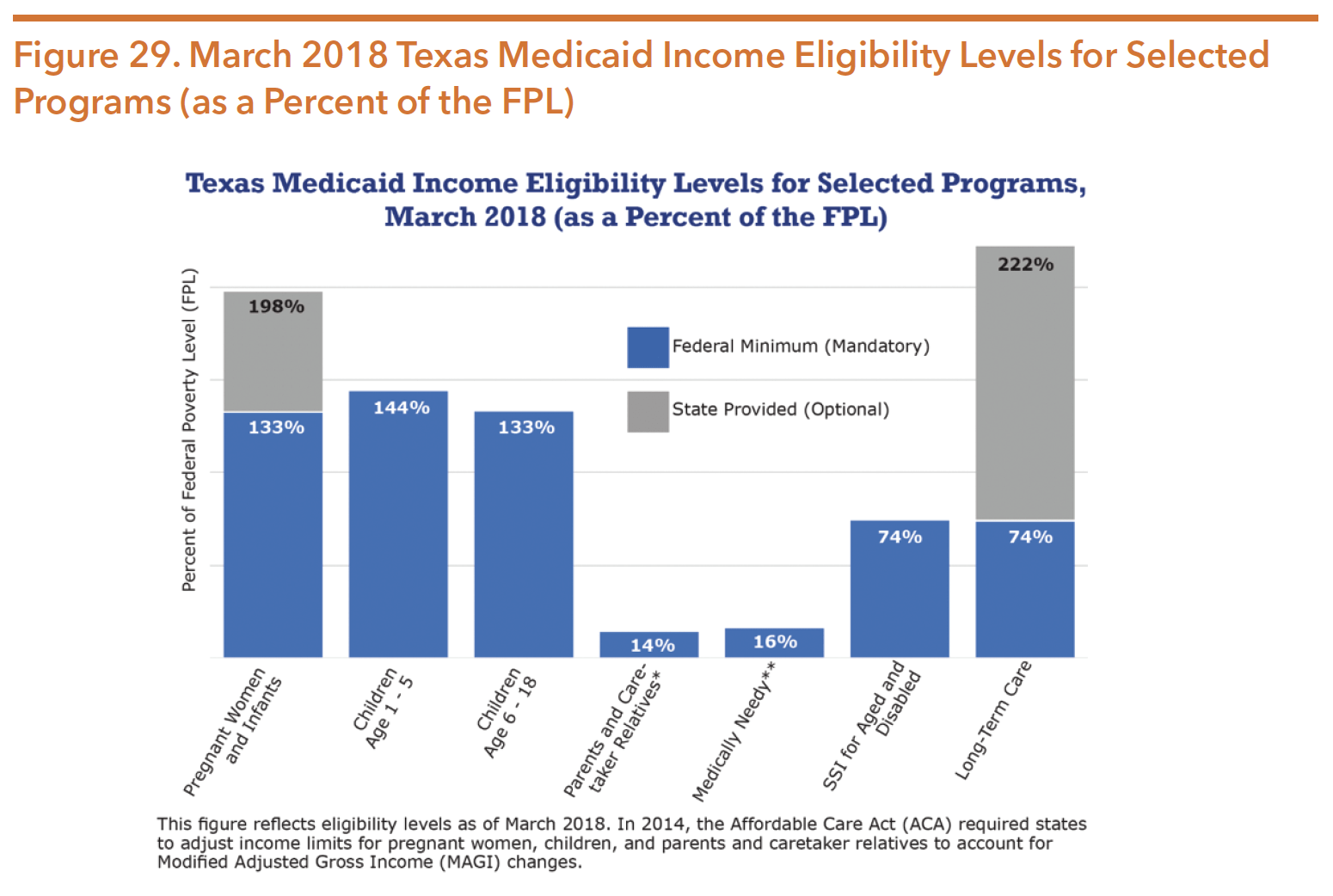
As of January 2019, extremely low-income parents are eligible to receive Medicaid only if their household income is 17 percent of FPL or below, about $307 per month for a family of three. Federal law requires states to cover certain groups and allows states the option to expand eligibility beyond minimum federal standards. Texas Medicaid covers a limited number of optional groups. Because Texas chose not to expand Medicaid eligibility through the Affordable Care Act, the program does not serve the majority of low-income, working adults. Thus, childless adults who are below age 66 and do not have a disability are currently ineligible for Medicaid. Figure 29 shows the income eligibility requirements for each Medicaid category.
Source: Texas Health and Human Services Commission. (2017). Texas Medicaid and CHIP in perspective eleventh edition. Page 4. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/ reports-presentations/2018/medicaid-chip-perspective-12th-edition/12th-edition-complete.pdf
*For Parents and Caretaker Relatives, the maximum monthly income limit in SFY 2018 was $230 for a family of three (one-parent household), which is the equivalent of approximately 14 percent of the FPL.
**For Medically Needy pregnant women and children, the maximum monthly income limit in SFY 2018 was $275 for a family of three, which is the equivalent of approximately 16 percent of the FPL.
Table 18 below shows the 2020 federal poverty level guidelines for families of households of different sizes.
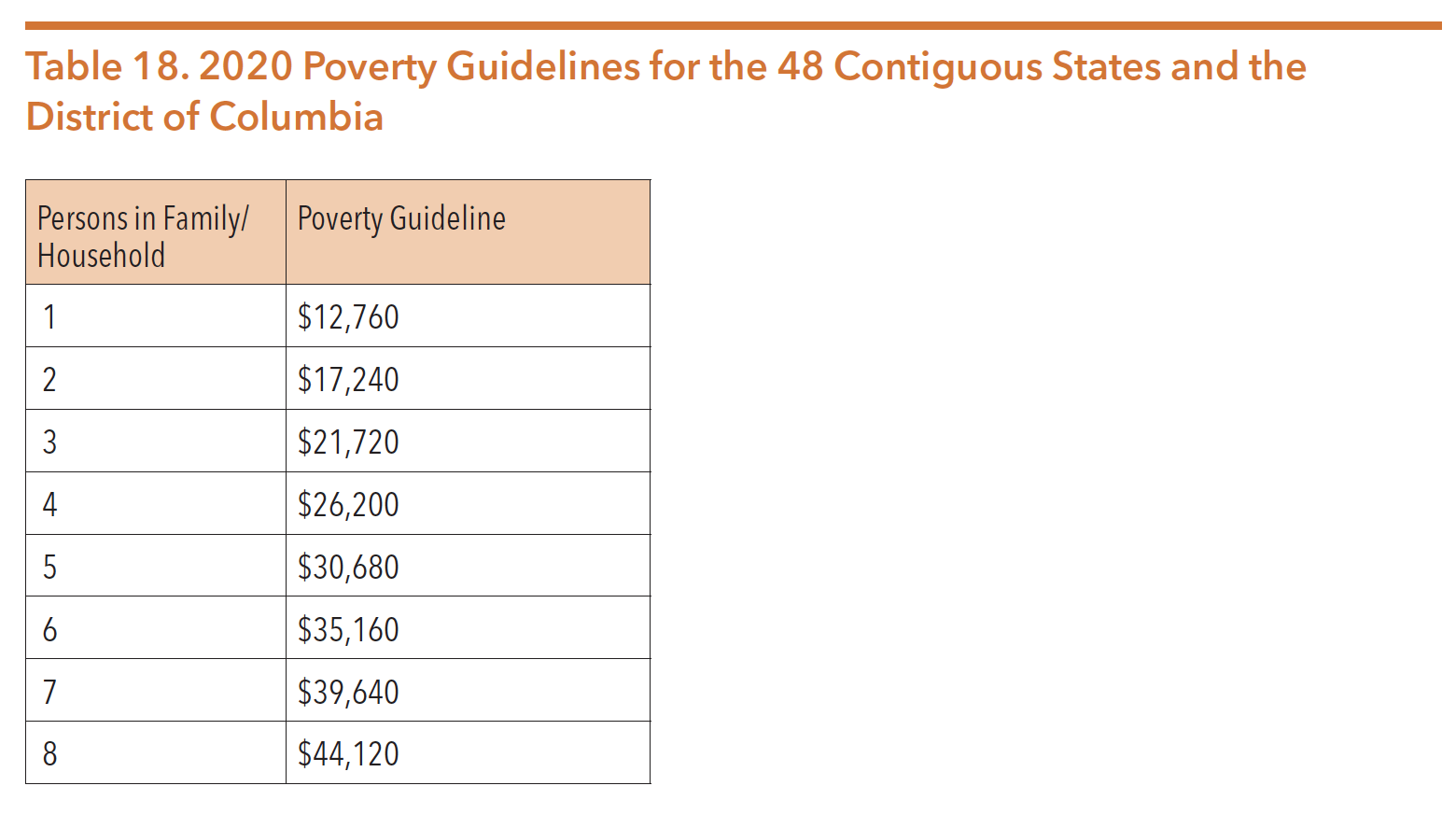
Source: U.S. Department of Health & Human Services, Office of the Assistant Secretary for Planning and Evaluation. (2020). U.S. federal poverty guidelines used to determine financial eligibility for certain federal programs. Retrieved from https://aspe. hhs.gov/poverty-guidelines.
MEDICAID SERVICES
Medicaid recipients, both adults and children, have access to the mental health and substance use services included in the Medicaid State Plan, such as psychiatric services, counseling, medication, and medication management. Medicaid also funds rehabilitative and targeted case management services by approved providers, primarily the local mental health authorities (LMHAs) operating under HHSC. In addition, HHSC administers several Medicaid-funded waiver programs that offer behavioral health or long-term services and supports to specialized populations. These services and eligibility criteria are further described later in this section.
Behavioral health screening services are an important component of services offered. Following are approved screening services:
- Health and Behavior Assessment and Intervention (HBAI) – eligible to youth 20 and younger designed to identify psychological, behavioral, emotional, cognitive, and social factors that contribute to preventing, treating, or managing physical symptoms. This screening is available to individuals who have underlying physical illness or injury. HBAI services are provided through licensed practitioners of the healing arts (LPHAs) co-located in the same building or office as the PCP to promote integrated care.
- Screening, Brief Intervention and Referral to Treatment (SBIRT) – eligible to individuals 10 years of age and older who are at risk of, or who have a substance use concern. Prevention and early intervention services are eligible to be delivered in community-based services and hospitals.
Approved Medicaid mental health treatment services include:
- Psychiatric diagnostic evaluations and psychotherapy performed by psychiatrists, psychologists, licensed clinical social workers, licensed professional counselors, and licensed marriage and family therapists;
- Psychological and neuropsychological testing performed by psychologists and physicians;
- Inpatient psychiatric care in a general acute care hospital;
- Inpatient care in psychiatric hospitals (for persons age 20 and younger, and age 65 and older);
- Psychotropic medications and pharmacological management of medications;
- Rehabilitative and targeted case management services for people with severe and persistent mental illness or children with severe emotional disturbances;
- Peer Support Services provided by a Certified Peer Specialist;
- Care and treatment of behavioral health conditions provided by a primary care physician; and
- Comprehensive community services for YES waiver participants (see YES waiver information later in this section).
Approved Medicaid substance use services include:
- Assessments to determine an individual’s need for services;
- Individual and group outpatient substance use counseling;
- Outpatient detoxification;
- Residential detoxification;
- Ambulatory detoxification;
- Residential treatment; and
- Peer Support Services provided by a Certified Recovery Coach.
Medication-assisted therapy (MAT) services are approved to be delivered by licensed chemical dependency treatment facilities (CDTFs), opioid treatment programs, or qualifying practitioners. During the 86th legislative session, SB 1586 (West/Klick) expanded prescribing ability. The legislation aligned Texas Medicaid policy with federal law by using the federal definition of “qualifying practitioner,” which includes physicians, physician assistants, nurse practitioners, clinical nurse specialists, certified registered nurse anesthetists, and certified nurse midwives. MAT is primarily used for opioid use conditions but can be provided for alcohol use conditions through the pharmacy benefit. Medications used for MAT are FDA-approved, recommended by the Texas Drug Utilization Review Board, approved by the HHSC Executive Director, and contained in the Preferred Drug List (PDL). Updated PDL and coinciding prior authorization criteria can be found here: https:// www.txvendordrug.com/formulary/prior-authorization/preferred-drugs.
DEMOGRAPHICS OF MEDICAID RECIPIENTS
As of January 2020, 3.5 million Texans across the state received services through Medicaid. A large number of Medicaid recipients are children and young adults, with 27 percent of enrollees are ages 0-5, 35 percent are ages 6-14, and 15 percent are ages 15-20. Non-disabled children make up 69 percent of Medicaid’s client caseload and 30 percent of Medicaid spending. In contrast, individuals who are elderly, blind, or have a disability account for 24 percent of the Medicaid population, but represent 61 percent of total estimated expenditures. Figure 30 displays the population of Medicaid enrollees and program expenditures by age and disability status.
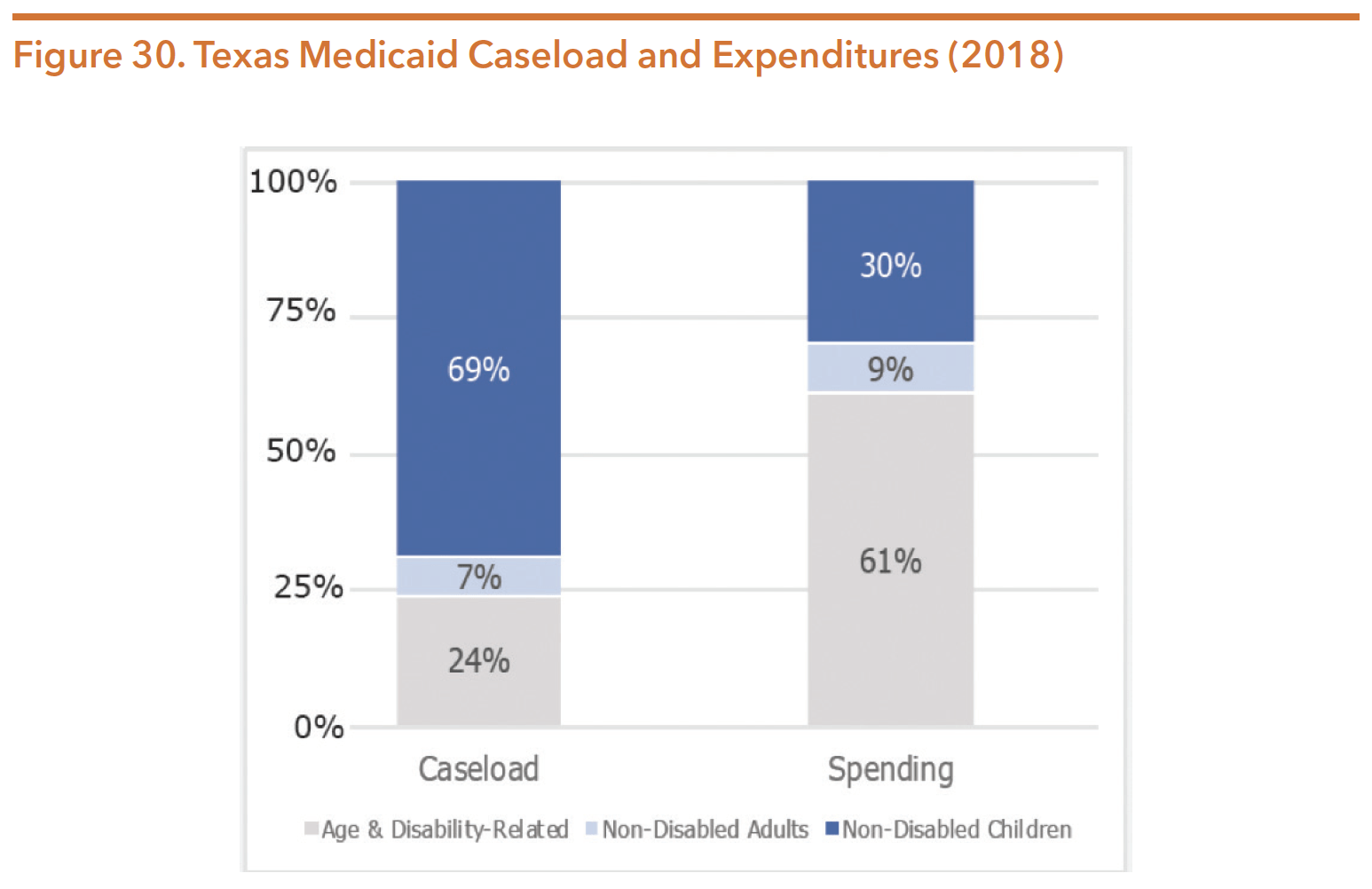
Source: Texas Health and Human Services Commission. (2018). Texas Medicaid and CHIP in perspective twelfth edition. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2018/medicaid-chip-perspective-12th-edition/12th-edition-complete.pdf
For more information regarding Medicaid, consult HHSC’s latest edition of Texas Medicaid and CHIP in Perspective, commonly known as the “Pink Book”, available at https://hhs.texas.gov/reports/2018/12/ texas-medicaid-chip-reference-guide-twelfth-edition-pink-book
TEXAS MEDICAID AND HEALTHCARE PARTNERSHIP
The Texas Medicaid and Healthcare Partnership (TMHP) is a group of subcontractors operating under the consulting firm Accenture, which contracts with HHSC to administer the state’s Medicaid fee-for-service claims payments and all Medicaid enrollment activities. All Medicaid managed care providers must first be enrolled in Medicaid through TMHP before they can be credentialed and part of an MCO network. TMHP does not process claims for services provided by MCOs, but it does collect encounter data from MCOs to use for the evaluation of quality and utilization of managed care services.
CHILDREN’S HEALTH INSURANCE PROGRAM (CHIP)
The federal government created the Children’s Health Insurance Program (CHIP) in 1997 under Title XXI of the Social Security Act. As with Medicaid, CHIP is jointly funded by state and federal governments. State participation in CHIP requires that the state develop a state CHIP plan for approval by the Centers for Medicaid and Medicare Services (CMS). While CMS allows states to combine their Medicaid and CHIP programs under a single administrative umbrella, Texas administers these programs separately. In September 2017, federal funding for CHIP expired. Initially in 2018, Congress extended CHIP funding for six years as part of a short-term resolution. Later during budget negotiations, Congress extended CHIP funding further through fiscal year 2027. Funds have been allocated for the first six years of the extension. Specific allotments were not included for FY 2024-27, but instead specifies that “such sums” as necessary will be available. Changes made that will impact the future of the program include:
- A decrease in the enhanced FMAP (as provided by ACA) from the current 23 percentage point enhancement to 11 in 2020 and down to traditional FMAP levels in 2021 and beyond;
- On October 1, 2019, states with CHIP eligibility levels above 300 percent FPL will have the option to lower eligibility to 300 percent FPL. States with CHIP eligibility levels below 300 percent (including Texas, 201 percent FPL) must maintain current eligibility levels until September 30, 2027; and
- Beginning in FY 2024, states will be required to annually report a set of core pediatric quality measures to CMS that were previously voluntary, including performance of primary care access and preventative care and behavioral health care.
CHIP FUNDING
Table 19 below shows CHIP funding trends over the last three budget cycles.
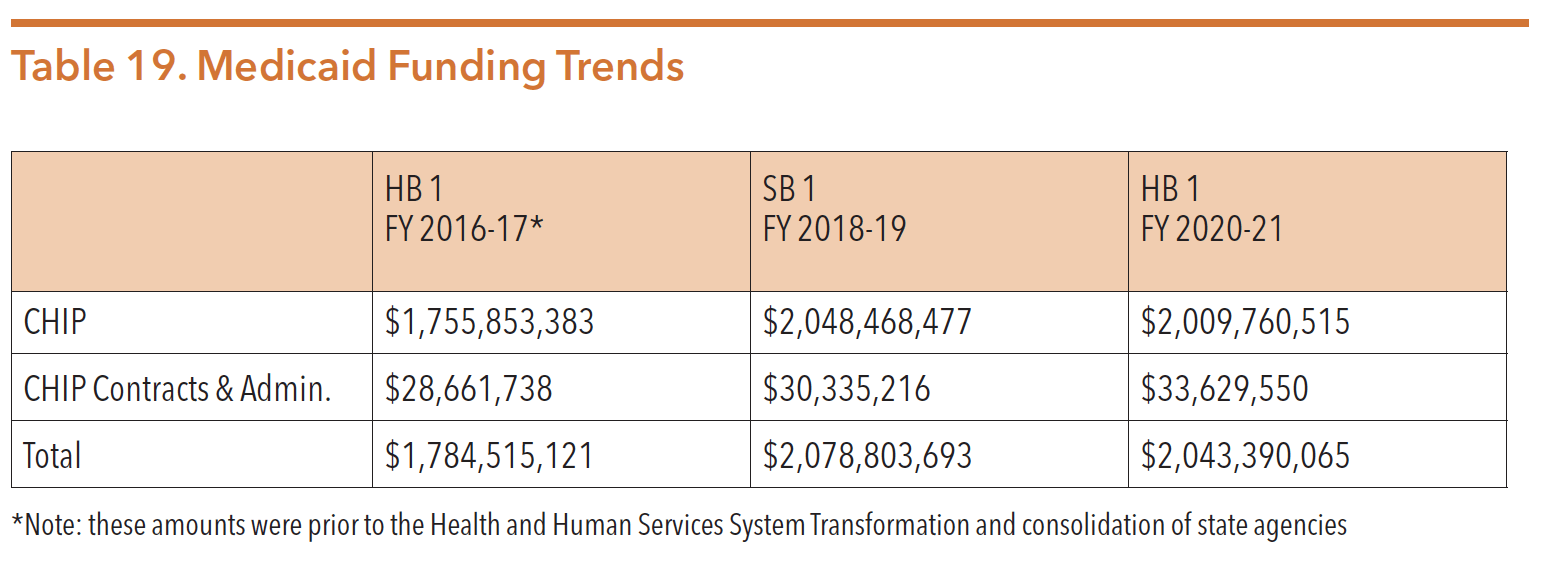
Sources: Texas Legislature Online (2019). H.B.1, General Appropriations Act, 86th Legislature, FY 2020-21. Retrieved from https://capitol.texas.gov/tlodocs/86R/billtext/pdf/HB00001F.pdf#navpanes=0
Texas Legislature Online (2017). S.B.1, General Appropriations Act, 85th Legislature, FY 2018-19. Retrieved from https://capitol.texas.gov/tlodocs/85R/billtext/pdf/SB00001F.pdf#navpanes=0
Texas Legislature Online (2015). H.B.1, General Appropriations Act, 84th Legislature, FY 2016-17. Retrieved from https://capitol.texas.gov/tlodocs/84R/billtext/pdf/HB00001F.pdf#navpanes=0
CHIP ELIGIBILITY
The federal government developed CHIP to provide a health insurance coverage option for children whose families had too much income or too many assets to qualify for Medicaid, but not enough to afford private insurance through their employer or through the individual market. CHIP is available to children under age 19 who are ineligible for Medicaid, who are living in households with an income at or below 201 percent of the FPL, and who have been uninsured for at least 90 days or have a good cause exemption. For these children, CHIP provides access to health care, including inpatient and outpatient mental health and substance use services. In contrast to Medicaid, CHIP requires cost sharing through enrollment fees and co-payments based on a family’s income. Families may pay up to a $50 enrollment fee for a 12-month period. Texas also opted to administer a CHIP perinatal program which covers perinatal services, including labor, delivery, and postpartum care for women and their unborn child with household incomes of up to 202 percent of the FPL. The majority of CHIP clients are over age five, with 11 percent being between the ages of 6 and 14, and 41 percent between the ages of 15 and 18.
The table below provides monthly household income limits for CHIP eligibility in Texas.
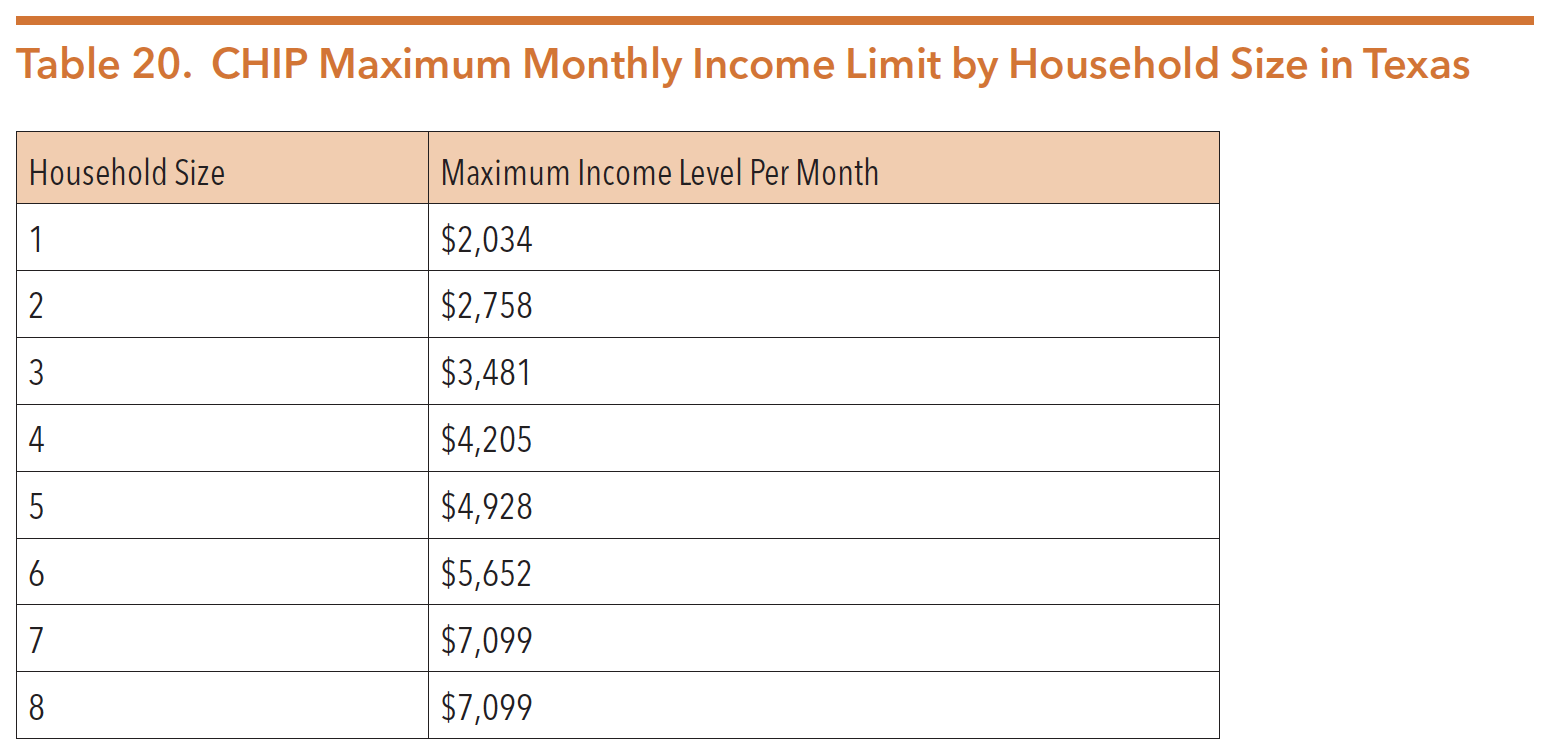
Source: Texas Health and Human Services Commission. (2018). Texas Medicaid and CHIP in perspective twelfth edition. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2018/ medicaid-chip-perspective-12th-edition/12th-edition-complete.pdf
Figure 31 below shows the monthly CHIP enrollment numbers in Texas from 2015 to 2020.
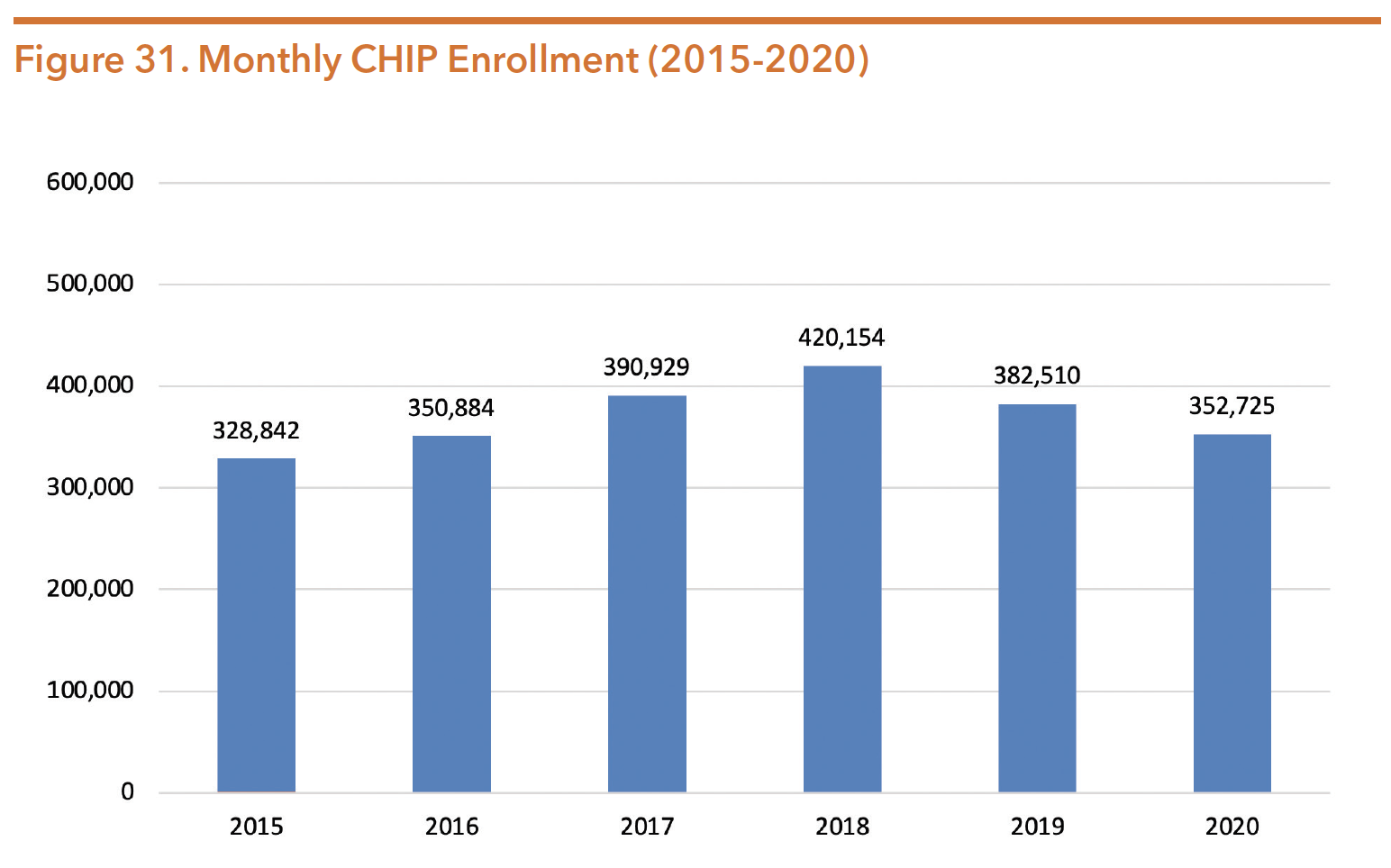
Note: Data is from January of each year.
Source: Texas Health and Human Services Commission. (September 2020). CHIP monthly enrollment detail (September 2014-June 2020) (XLS) [data file]. Retrieved from https://hhs.texas.gov/about-hhs/records-statistics/data-statistics/healthcare-statistics
CHIP SERVICES
The CHIP program offers many of the same services to children as those enrolled in Medicaid, including mental health care and substance use services.
Mental health treatment services include:
- Neuropsychological and psychological testing;
- Medication management;
- Rehabilitative day treatments;
- Residential treatment services;
- Sub-acute outpatient services (partial hospitalization or rehabilitative day treatment)
- Skills training; and
- Inpatient mental health services in a free-standing psychiatric hospital, psychiatric unit of a general acute care hospital, or state-operated facility.
Additionally, the following substance use treatment services are available to CHIP members:
- Inpatient treatment, including detoxification and crisis stabilization;
- Outpatient treatment services, including group and individual counseling;
- Intensive outpatient services;
- Residential treatment;
- Partial hospitalization; and
- Prevention and intervention services by physician and non-physician providers.
- Medication assisted treatment (MAT) is not a covered benefit through CHIP, however can be provided as a prescription drug benefit
HHSC QUALITY OF CARE REVIEW AND THE HEALTHCARE QUALITY PLAN
Texas contracts with the University of Florida Institute for Child Health Policy as the external quality review organization (EQRO) to review the Texas Medicaid Managed Care programs. The annual quality of care evaluation compares Texas’ performance to the national Healthcare Effectiveness Data and Information Set standards, or alternatively to benchmarks that HHSC establishes. The national Healthcare Effectiveness Data and Information Set (HEDIS) standards are used across the country to measure performance within health care, including behavioral health services.
The latest review of Texas managed care programs for FY 2018 was released in May 2019. The report found that HHSC has done significant work to improve the quality of care within behavioral health. HHSC asked the EQRO to complete quarterly topic reports examining the following:
- Factors leading to potentially preventable service use among Medicaid members with co-occurring behavioral and physical health conditions,
- Ways to integrate behavioral and physical health services, and
- Investigations of opioid prescribing measures.
The review also included evaluations and surveys of STAR, STAR+PLUS, STAR Health, and STAR Kids. A number of behavioral health findings offer the opportunity for improvement including:
- In all programs, the rates of members who were hospitalized for mental illness and received follow-up visits (within 30 days and within 7 days) were low compared to national benchmarks and state standards.
- Among health plans, the percentage of in-network providers excluded from members’ lists to schedule an appointment due to “no answer after three attempts” or “wrong number/unreachable provider” ranged from 48 percent to 61.1 percent.
- Providers identified psychiatric care as the most difficult referral type for both children and adult patients, with referrals for both children and adults frequently taking longer than one month.
- MCOs noted that issues of network access or adequacy included shortages of behavioral health providers and other specialists.
- Based on the findings, the report offered a number of recommendations including:
- Programs should give considerable attention to efforts to establish, improve, and monitor behavioral and physical health care integration practices.
- Recruitment of specialized providers should include negotiating reasonable and appropriate payment rates.
- MCOs should improve access to care through transportation assistance and telemedicine services in rural areas where shortages of behavioral health and specialist providers are common.
Improved performance, improved measurement of performance, and payment mechanisms based on performance appear to be a priority for both the legislature and HHSC. There are six strategic priorities incorporated in the HHSC Healthcare Quality Plan as required by SB 200 (84th, Nelson/Price) including:
- Keeping Texans healthy
- Providing the right care in the right place, at the right time
- Keeping patients free from harm
- Promoting effective practices for chronic disease
- Supporting patients and families facing serious illness
- Attracting and retaining high performing providers and other healthcare professionals
SB 200 (84th, Nelson/Price) granted the HHS Executive Commissioner authority to establish the Value Based Payment and Quality Improvement Advisory Committee. The Committee submits a report to the Texas Legislature and to HHSC each December, including recommendations on “value-based payment and quality improvement initiatives to promote better care, better outcomes, and lower costs for publicly funded health care services.” The committee’s report to the 86th legislature included the following behavioral health recommendations:
- Sustaining innovative behavioral health models, including DSRIP projects funded through the 1115 waiver and use of the Certified Community Behavioral Health Clinics (CCBHC) model;
- Expanding substance use treatment;
- Studying value-based options for substance use identification; and
- Recommend Medicaid to evaluate bundle rates for MAT for more efficiency. (Note: The SAPT block grant reimbursement rate includes counseling in addition to medication, whereas Medicaid has separate reimbursement for medication and counseling).
More information on the committee can be found at https://hhs.texas.gov/about-hhs/leadership/advisory-committees/ value-based-payment-quality-improvement-advisory-committee
In addition to the Value Based Payment and Quality Improvement Advisory Committee, HHSC has a number of value-based care programs and initiatives, including:
- MCO/DMO Pay-for-Quality (P4Q)
- MCO Alternative Payment Models (APM)
- Hospital Quality Payment Program
- DSRIP Program
- Nursing Home Quality Incentive Payment Program (QIPP)
- Uniform Hospital Rate Increase Program (UHRIP)
- Network Access Improvement Program (NAIP)
- HHS Quality Webpage
- Texas Healthcare Learning Collaborative Portal
- Advisory Committees and Workgroups
The Texas Legislature continues to direct HHSC to prioritize value and transparency in the Medicaid program. Among the budget riders included in Article II of HB 1, Rider 43 required HHSC to implement an incentive program that automatically enrolls a greater percentage of Medicaid recipients who have not selected a managed care plan into a plan based on quality of care, efficiency, and effectiveness of service provision and performance. Appropriations for FY 2021 were contingent on HHSC implementing this program by September 1, 2020
Intellectual and Developmental Disabilities & Behavioral Health Services Division
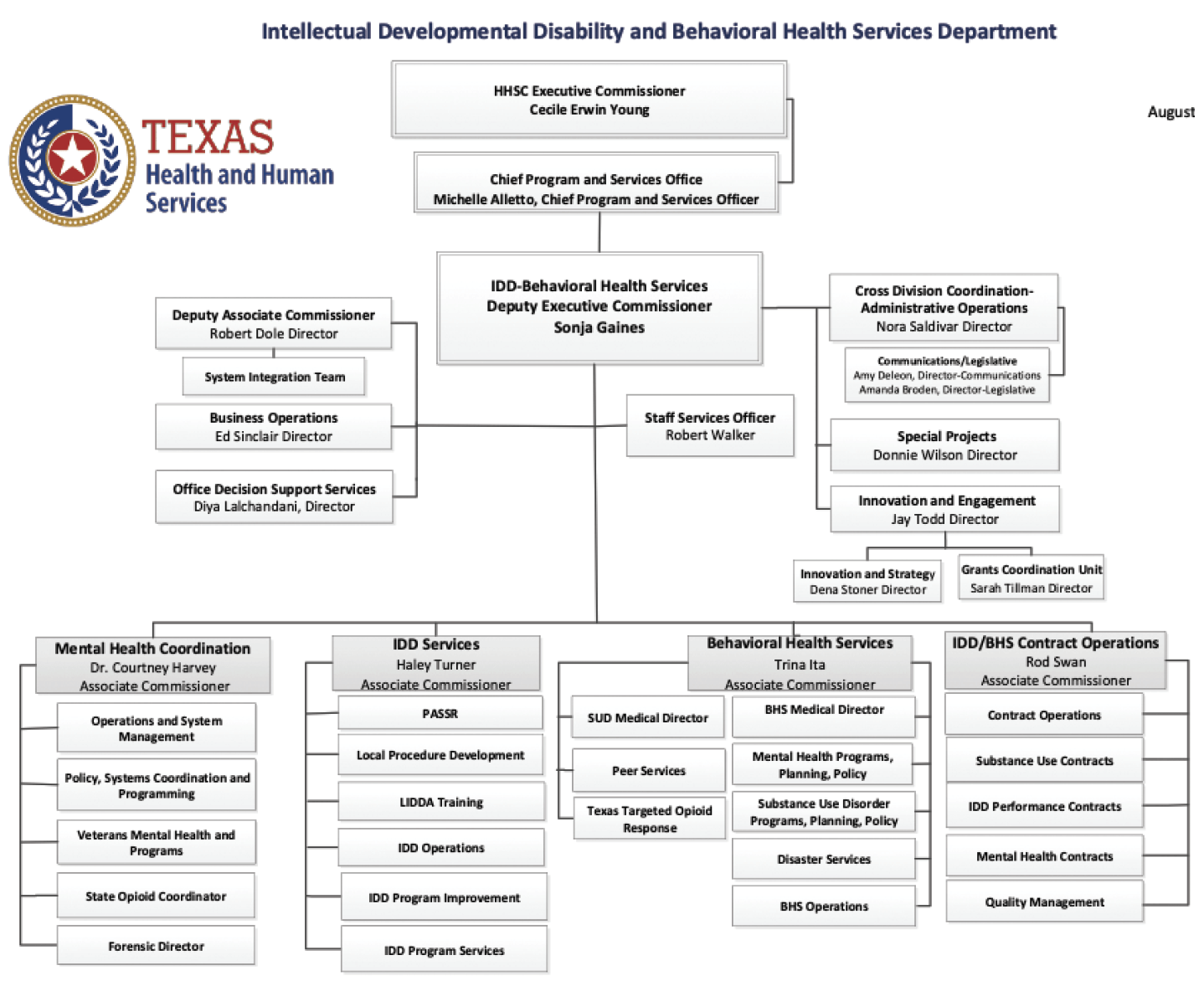
Source: Texas Health and Human Services Commission. (August 2020). Public Information Request, October 2020.
The Intellectual and Developmental Disabilities and Behavioral Health Services Department combines responsibility for community services for individuals with intellectual and other developmental disabilities and those living with mental health and substance use conditions under one deputy executive commissioner authority.
Public behavioral health services are mainly comprised of community mental health, substance use, and inpatient psychiatric services. These services are provided to residents through the 39 local mental health authority (LMHA) regions and 20 Regional Health Partnerships (RHPs) in all of Texas’ 254 counties. The Medical and Social Services Division has oversight responsibility for community behavioral health services while the Health and Specialty Care has oversight of state-run and contracted inpatient services.
MENTAL HEALTH
HHSC prioritizes access to treatment and services for individuals with a serious mental health condition, who are eligible for Medicaid, determined to be indigent, or who fall under the priority populations criteria (major depression, bipolar, and schizophrenia). Resources, eligibility for services, and service delivery systems are the primary determinants of the accessibility and quality of services. Texas continues to seek ways to improve access so that individuals with mental health and substance use conditions can receive the level of care and support that are clinically appropriate for their level of need. HHSC maintains a central website, www.mentalhealthtx. org, to improve access to information. Individuals can enter their zip code and find available mental health and substance use services in their area.
Since November 2018, leadership from leadership from Intellectual and Developmental Disability and Behavioral Health Services, the Health and Specialty Care System, Medicaid, Regulatory, and Aging Services Coordination have worked together to form the HHSC Continuum of Care Workgroup. The Workgroup is responsible for addressing issues and solutions to improve the continuum of care within behavioral health services across the human services system. The objectives of the work group include:
- Ensuring the most effective and efficient communication and coordination between state hospitals and local mental health authorities (LMHAs), to provide seamless care;
- Identifying gaps and barriers to continuity of care, and more specifically to successful discharge from state hospitals; and
- Identifying short-term and long-term goals to address the identified gaps and barriers.
As of October 2019, the Workgroup made progress on several initiatives to meet these goals including:
- Transitioning the nine state hospital patients with IDD who had been hospitalized for over one year to a less restrictive settings in the community;
- Address licensing barriers to provide integrated Co-occurring psychiatric and substance abuse disorders COPSD) services by working to revise substance use treatment standards of care in the Texas Administration Code Title 25, Chapter 448;
- Beginning in FY 2020, LMHAs/local behavioral health authorities (LBHAs) will be required to have a dedicated Continuity of Care Worker as outlined in their FY 20 performance contracts. The worker will be solely responsible for ensuring effective transitions from inpatient or residential care to the community; and
- Creating collaborative clinical review teams at HHSC hospitals responsible for reviewing individuals who have be in inpatient care for more than a year and are deemed to no longer meet criteria for inpatient level of care.
MENTAL HEALTH FUNDING
Mental health services are provided through a number of programs across multiple state agencies. Efforts to provide these services can lead to diverse funding and often unclear delineation. HHSC has attempted to better identify and monitor funding for mental health services through the Statewide Behavioral Health Coordinating Council and a statewide consolidated expenditure report. For a more in-depth overview of the expenditure report and behavioral health funding across state agencies, please refer to the Funding section of this guide.
This section is meant to provide historical context to funding and show trends. The information provided in this section refers only to the funding appropriated to the behavioral health section of the Medical and Social Services Division.
Much of the increased demand for behavioral health services in Texas is due to the state’s rapidly growing population from 25,145,561 in 2010 to 28,995,881 in 2019. The population growth rate in Texas was 15.3 percent between 2010 and 2019, more than double the national average of 6.3 percent.
While the amount of funding per person has improved as a result of recent increases in mental health appropriations, the preceding decade of stagnant funding has been unable to keep pace with the increased cost of services and the continued state population growth. This culmination has resulted in less service options and a decreased rate of persons receiving services. Table 21 below shows historical trends and appropriated amounts of all funds for mental health services over the last three budget cycles.
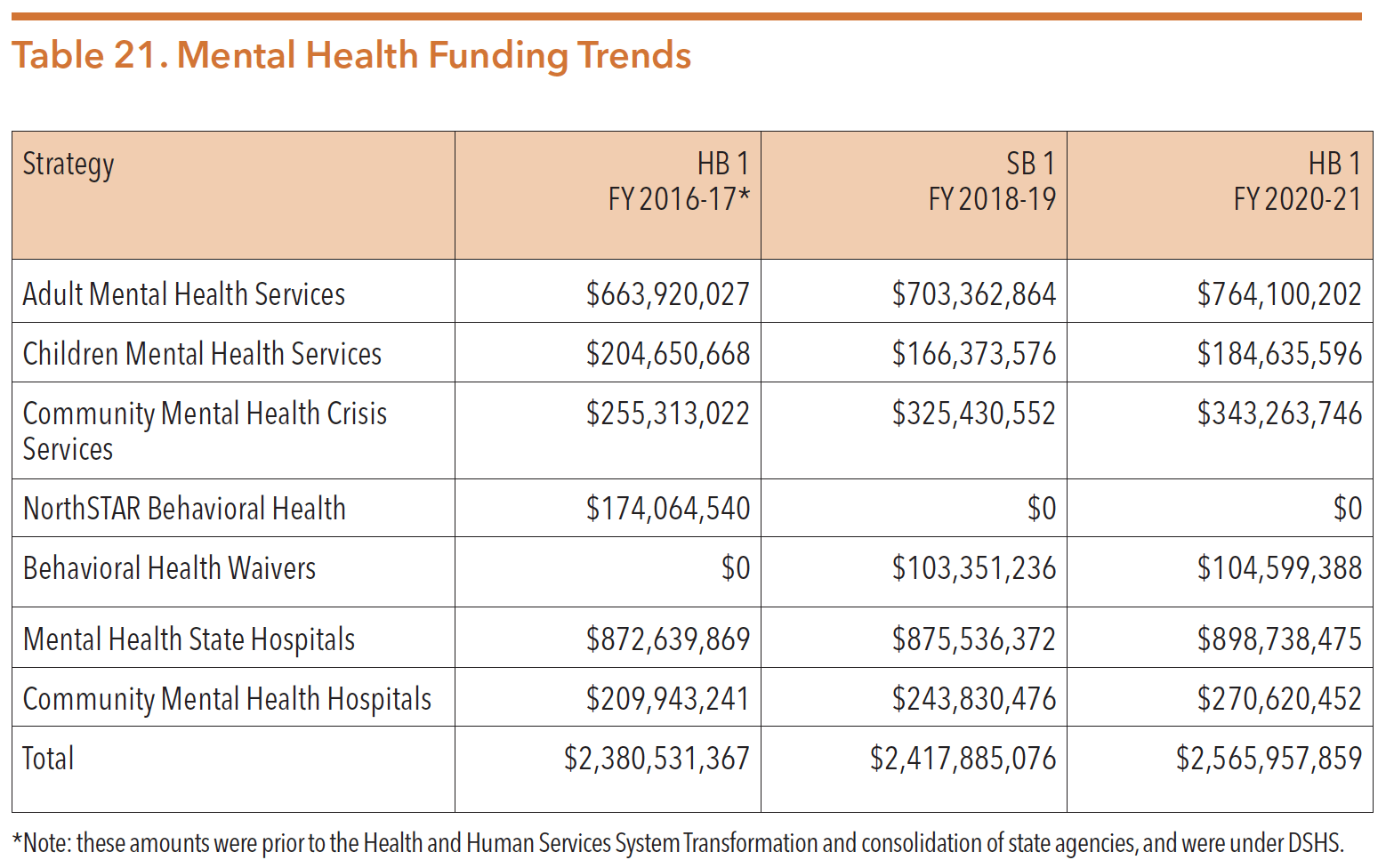
Sources: Texas Legislature Online (2019). H.B.1, General Appropriations Act, 86th Legislature, FY 2020-21. Retrieved from https://capitol.texas.gov/tlodocs/86R/billtext/pdf/HB00001F.pdf#navpanes=0
Texas Legislature Online (2017). S.B.1, General Appropriations Act, 85th Legislature, FY 2018-19. Retrieved from https://capitol.texas.gov/tlodocs/85R/billtext/pdf/SB00001F.pdf#navpanes=0
Texas Legislature Online (2015). H.B.1, General Appropriations Act, 84th Legislature, FY 2016-17. Retrieved from https://capitol.texas.gov/tlodocs/84R/billtext/pdf/HB00001F.pdf#navpanes=0
SERVICE PROVIDERS
Publicly funded mental health services in Texas are provided by three types of service providers:
- Medicaid Managed Care providers;
- Federally Qualified Health Centers (FQHCs) and other community health centers; and
- Local mental health authorities (LMHAs).
Medicaid Managed Care Providers
Medicaid is the largest funder of behavioral health services in Texas. Texas continues to expand the managed care model within the Medicaid system state-wide, including for behavioral health services.
Prior to 2013, public mental health services in Texas were available through contracts between the Department of State Health Services (DSHS) and the network of local mental health authorities (LMHAs). SB 58 (83rd, Nelson/Zerwas) directed the integration of physical health and behavioral health services into the managed care system. SB 58 (83rd, Nelson/Zerwas) allowed targeted case management and rehabilitative services to be delivered through Medicaid managed care by private comprehensive providers outside of LMHAs. However, the requirement to offer a full array of comprehensive services limited the number of providers able to bill for these services. Local authorities continue to serve as the primary providers of rehabilitative services and targeted case management for the majority of people in managed care.
Rehabilitative services coordinated through targeted case management include:
- Crisis intervention services;
- Medication training and support services;
- Skills training; and
- Developmental services and day programs for acute care.
Federally Qualified Health Centers
In addition to state-funded LMHAs/LBHAs and Medicaid managed care providers, individuals in Texas may also receive behavioral health services from federally qualified health centers (FQHCs) or other non-federally funded community health centers. The goal of FQHCs is to provide underserved communities with comprehensive healthcare, and some centers offer additional services such as mental health or substance use treatment. While the FQHC benefit was first added to Medicare in 1991, the passage of the ACA allocated $11 billion in new funding to build and expand health centers nationwide. FQHCs have since become a central component of the ongoing shift toward integrating behavioral health services with primary healthcare. In Texas, there are 73 FQHCs with more than 300 service delivery sites statewide. Additionally, there are 3 “FQHC-lookalikes,” that provide similar services without the benefits of a FQHC status.
FQHCs often provide healthcare services to Texans who are indigent, underinsured or uninsured. Services are provided to Medicare, Medicaid, and CHIP recipients, as well as insured and uninsured individuals. Individuals may be eligible for services based on their family income and on a sliding fee schedule. FQHCs receive federal grants through Section 330 of the Public Health Services Act. Section 330 of the Public Health Service Act created and authorized the health center program and permits the Health Resources and Services Administration (HRSA) to make grants to health centers.
FQHCs also play an important role in providing comprehensive health care services to individuals with public health insurance such as Medicaid and CHIP. FQHCs receive enhanced reimbursements for providing services to individuals enrolled in Medicaid and Medicare. These reimbursements are designed to cover the additional costs associated with providing comprehensive care to those who are uninsured and publicly funded. As a result of policy changes in 2010 made by the ACA, many FQHCs are transforming their practices to place individuals within health homes or comprehensive medical homes to improve the coordination and integration of care for h multiple chronic conditions, including mental health and substance use concerns.
Being certified as an FQHC brings a number of benefits, including:
- Cost-based (enhanced) payment for recipients of Medicare and Medicaid;
- Access to medical malpractice coverage through the Federal Tort Claims Act;
- 340b (reduced) drug pricing; and
- The ability to participate in the National Health Service Corps (NHSC).
Beyond the basic certification requirements of providing comprehensive services and having a quality assurance program, FQHCs must also meet the following requirements in order to receive federal funding under Section 330 of the Public Health Service Act:
- Serve an underserved area or population;
- Offer a sliding fee scale (i.e., individuals do not get turned away for inability to pay); and
- Have a governing board of directors with the majority of members receiving care at the FQHC.
Finally, many community health centers in Texas are affiliated with charitable, nonprofit organizations or hospitals, and typically serve as the public health safety net for individuals who are uninsured, underinsured, do not have the financial means to pay for services, or are in geographic locations where access to care is severely limited. While the central mission of most community health centers is to provide effective and affordable primary healthcare, many community health centers have started to partner with LMHAs/LBHAs and other providers to offer behavioral health services in their clinics. Due to FQHCs funding methods, there is less mandated reporting on client outcomes compared to LMHAs/LBHAs and Medicaid managed care providers. Thus, FQHCs are quickly becoming an integral part of the health safety net in many parts of Texas.
Local Mental Health Authorities and Local Behavioral Health Authorities
Public mental health services are primarily provided through HHSC contracts with 37 designated LMHAs and two LBHAs, often referred to as LMHAs, community mental health centers, or local authorities. The HHS System contracts with these authorities to provide or arrange for the delivery of both crisis and ongoing community mental health and substance use services for:
- Children, adolescents, and adults meeting medically indigent criteria;
- Individuals with a priority population diagnosis (schizophrenia, bipolar depression and major depressive order); and
- Any individuals eligible for Medicaid who reside in that LMHA’s designated geographic area, shown below in Figure 32.
. 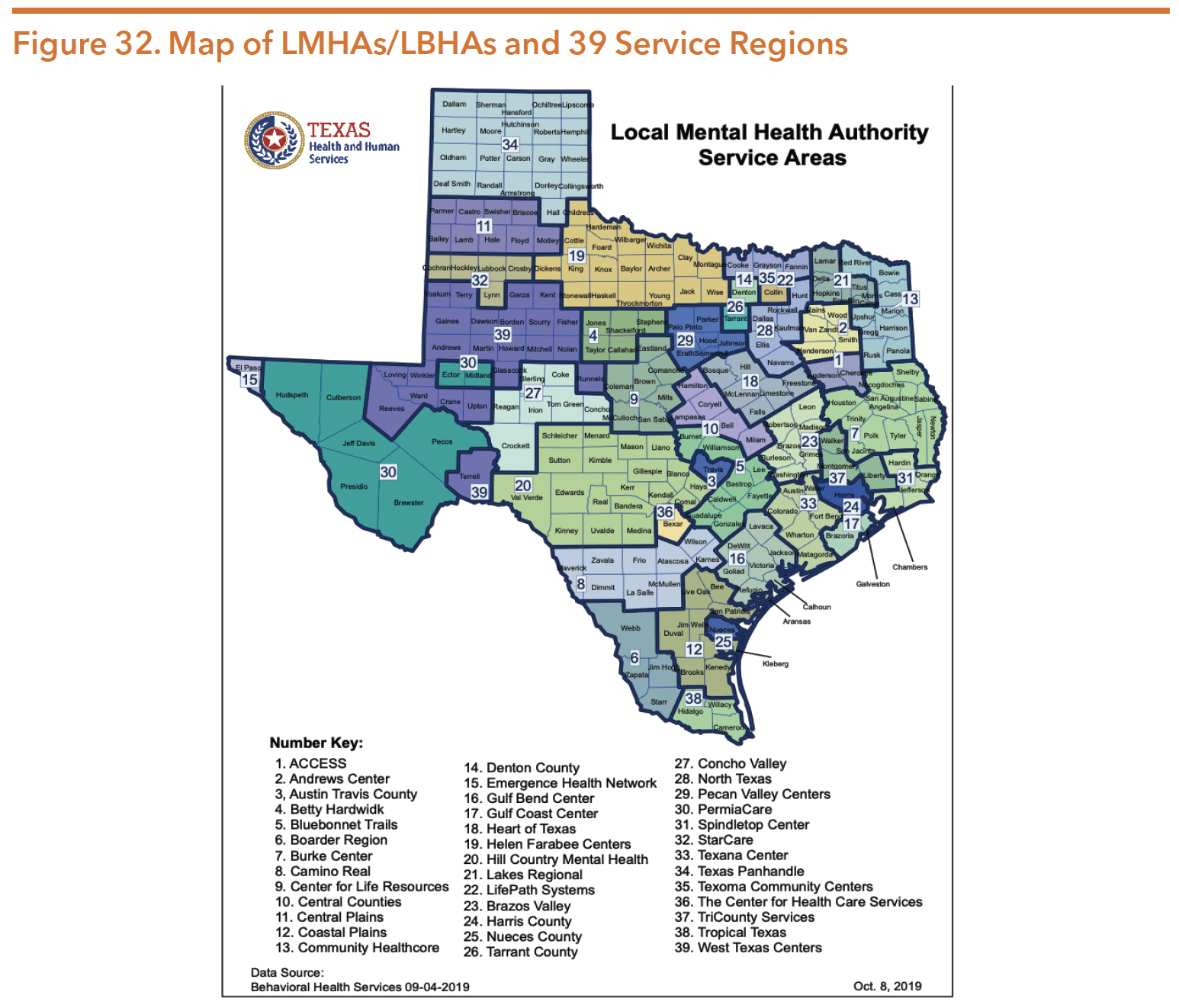
Source: Texas Health and Human Services. (2019.). Local mental health authority service areas. Retrieved from https://hhs.texas.gov/sites/default/files/documents/services/mental-health-substance-use/local-mental-health-authority-service-areas.pdf
All Texas Access
During the 86th legislation session, SB 633 (Kolkhorst/Lambert) was passed, creating the All Texas Access project. SB 633 directed HHSC to create regional authority groups of LMHAs to improve access to mental health care in rural areas. HHSC divided the LMHAs into seven regional areas aligned with the state hospital catchment areas depicted in Figure 33. While SB 633 only directed LMHAs in counties with a population of 250,000 or less to be assigned to a regional group, all 39 LMHAs across the state opted to be a part of this initiative. Each regional group is required to develop plans to increase the region’s capacity for mental health services with goals to reduce:
- Local government spending in providing mental health crises services;
- Transportation from LMHAs to mental health facilities;
- Incarceration of individuals in county jails due to a mental illness; and
- Emergency room (ER) visits as a result of a mental illness.
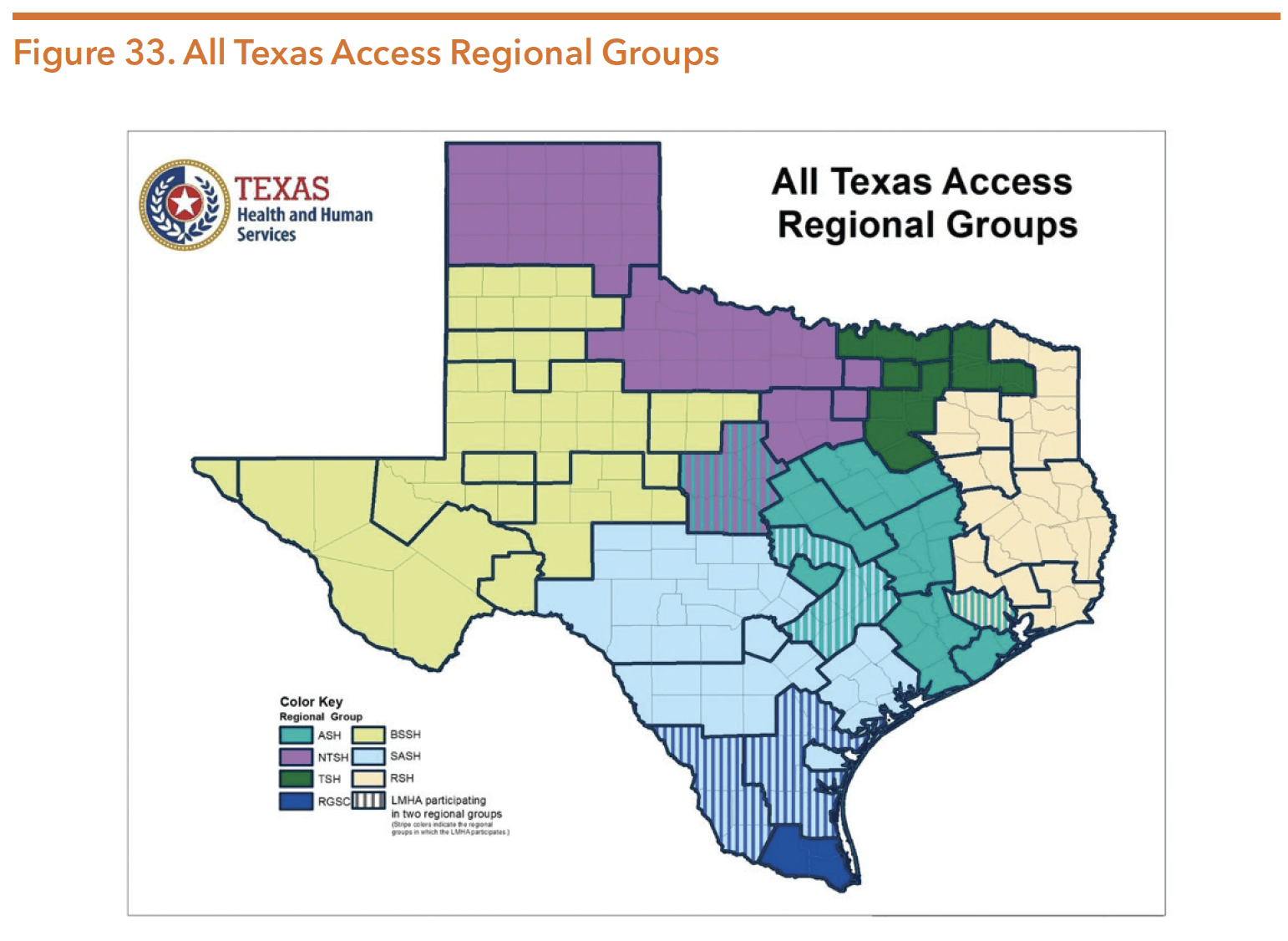
Source: Texas Health and Human Service Commission.(2020). HHSC All Access Texas presentation to the Behavioral Health Advisory Committee, June 23, 2020.
In addition to the plan development, each region is responsible for assessing the regional group’s capacity to provide needed services. HHSC and each region will evaluate:
- If (or to what degree) increasing the regions’ capacity to provide mental health services would offset costs to state or local government due to transportation, inpatient hospitalizations, ER visits and incarceration;
- Whether or not available state or grant funding could be used to carry out the regions’ plans; and
- How each plan aligns with the statewide behavioral health strategic plan and the comprehensive inpatient mental health plan.
Beginning in early 2020, HHSC began the process of developing the regional plans through focus groups, administration of a statewide input survey, discussions with LMHAs, and system mapping. Through the regional conversations and system mapping, themes emerged across the state including: the need for community education on how to access services, increased access to care, community and agency collaboration, transportation, telehealth, and housing. The statewide survey garnered over 2,600 respondents and key findings included rural Texans need basic access to mental health services. The direst service needs identified were counseling, crisis services, and transportation. Additionally, the top three barriers identified were lack of services in rural areas, transportation, and lack of community awareness of available services. HHSC planning timeline anticipates the All Access Texas report to be published online by December 1, 2020.
Additionally, HHSC worked to estimate the mental health costs to state or local government due to transportation, inpatient hospitalizations, ER visits and incarceration. Figure 34, Figure 35, and Figure 36 illustrates the estimation of costs HHSC determined.
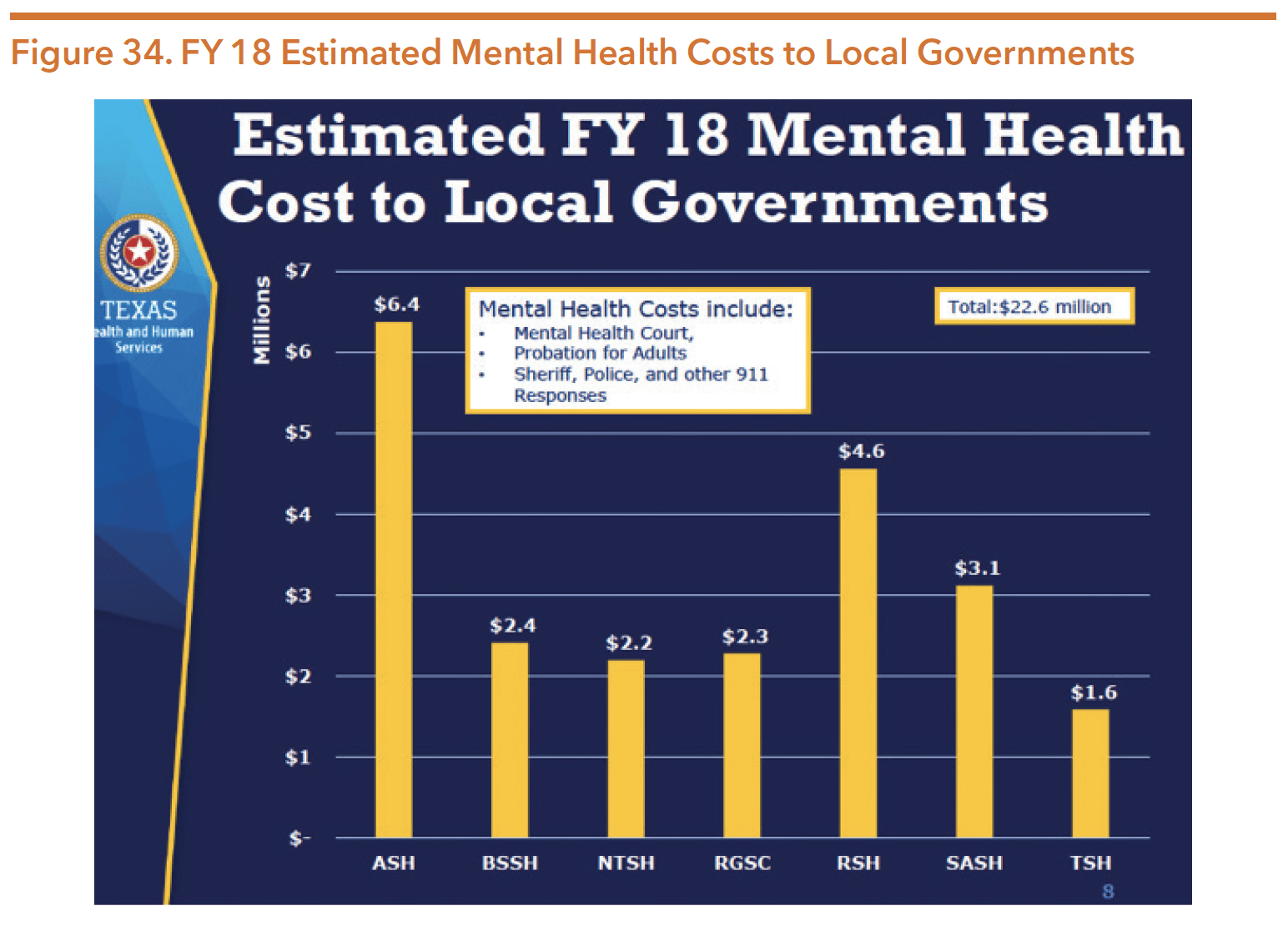
Source: Texas Health and Human Service Commission. (2020). HHSC All Access Texas presentation to the Behavioral Health Advisory Committee, June 23, 2020
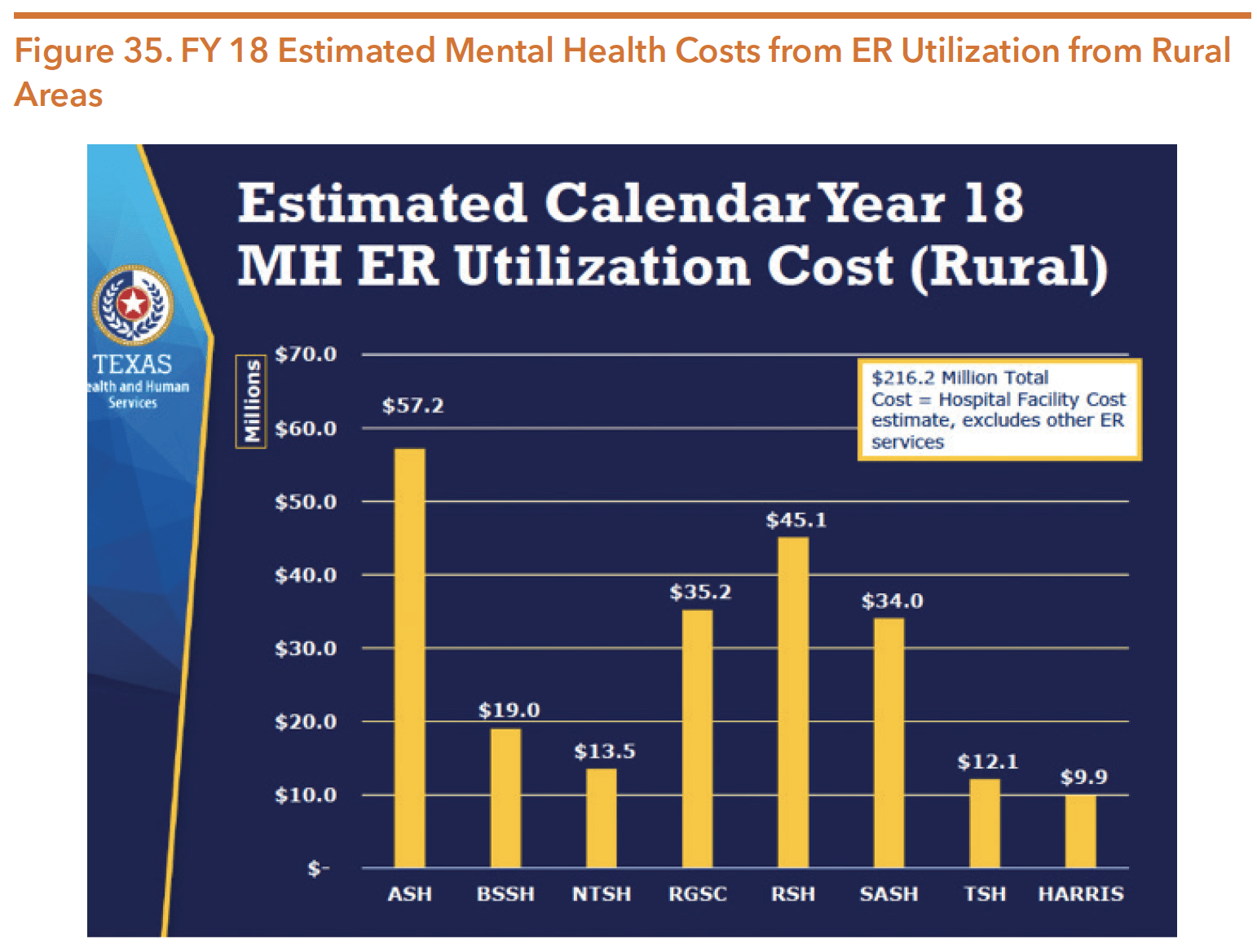
Source: Texas Health and Human Service Commission. (2020). HHSC All Access Texas presentation to the Behavioral Health Advisory Committee, June 23, 2020.
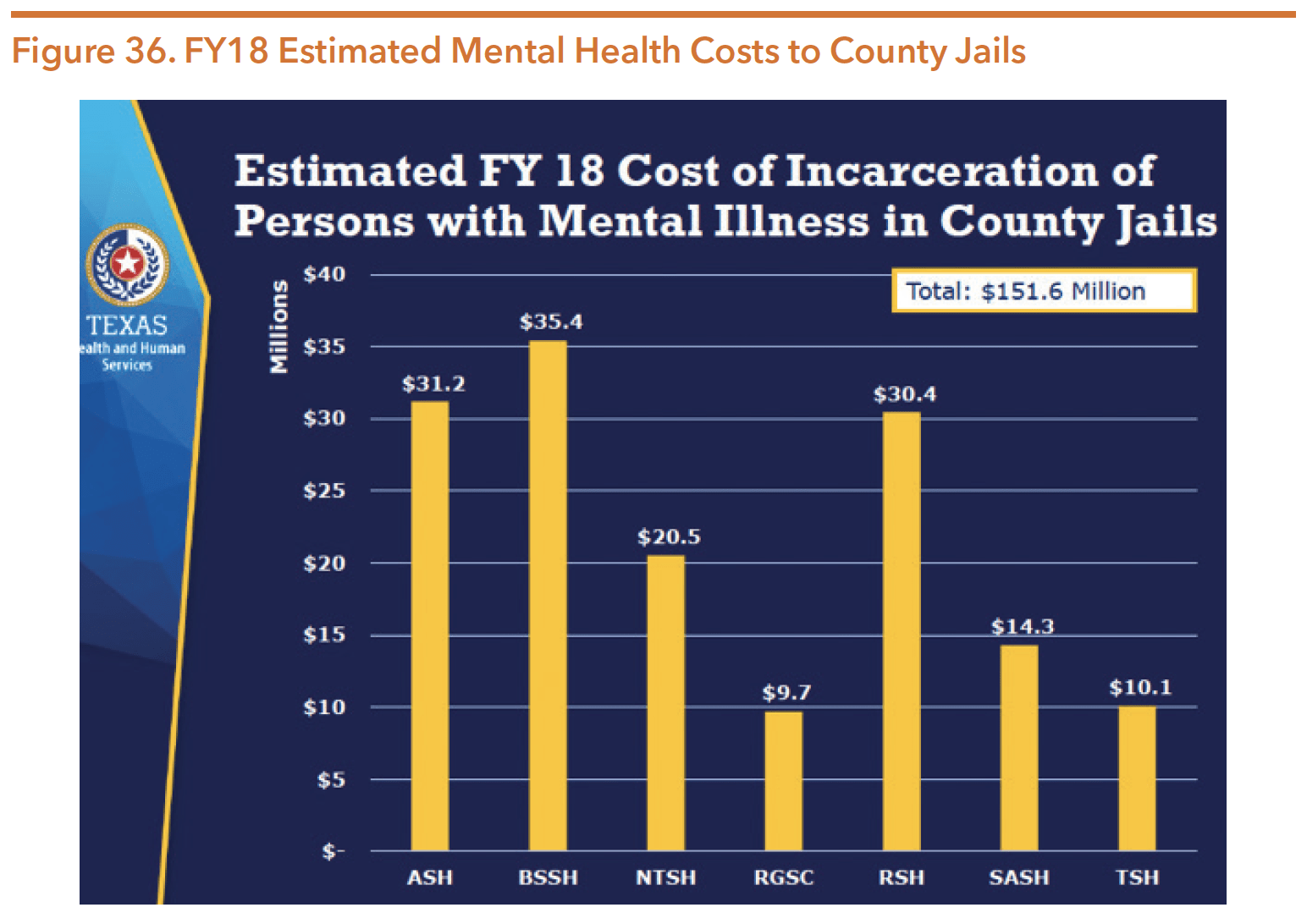
Source: Texas Health and Human Service Commission. (2020). HHSC All Access Texas presentation to the Behavioral Health Advisory Committee, June 23, 2020.
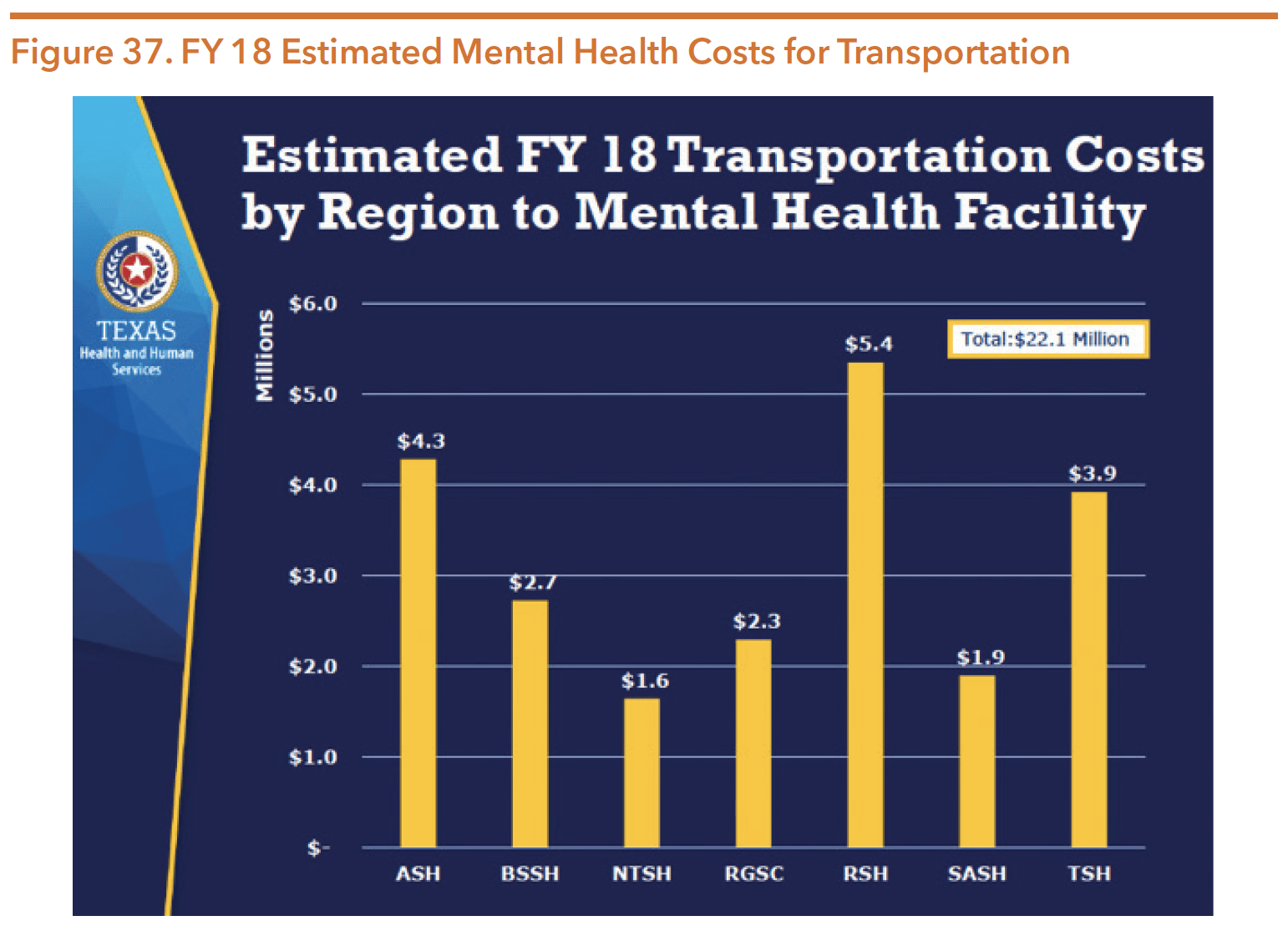
Source: Texas Health and Human Service Commission. (2020). HHSC All Access Texas presentation to the Behavioral Health Advisory Committee, June 23, 2020.
The Medical and Social Services Division oversees and regulates the quality of services provided to individuals through LMHAs/LBHAs and regularly provides LMHA/LBHA staff with training and technical assistance. LBHAs typically refer to local authorities that provide behavioral health services to include a broader range of substance use services than historically provided by LMHAs.
As an authority, LMHAs/LBHAs are responsible for:
- Allocating funds from the HHS Medical and Social Services Division to ensure mental health and substance use services are provided in the local service area for indigent populations;
- Balancing community input, cost effectiveness, and quality of care issues to ensure choice and the best use of public funds;
- Creating and maintaining a network of service providers;
- Recommending the most appropriate and available treatment alternatives for individuals requiring mental health services; and
- Demonstrating that the services provided comply with state health and regulatory standards, whether those services are provided directly by LMHA employees or through subcontractors and other private community providers involving state funds.
Each LMHA/LBHA is required to plan, develop, and coordinate local policy, resources, and services for mental health care. Additionally, LMHAs/LBHAs are required to ensure the best use of state funding to create a network of providers. LMHAs/LBHAs determine whether to provide a service, or contract that service to an outside organization. Some LMHAs have found it challenging to establish successful contracts for services, especially rehabilitation and other routine outpatient services, in part due to provider reimbursement rates and extensive behavioral health workforce shortages in rural counties and in the Texas-Mexico border regions. In such cases, LMHAs/LBHAs typically serve as primary service providers.
Individuals seeking mental health services can arrive at an LMHA/LBHA with or without an appointment. The first step to services is for a qualified mental health professional to provide a brief mental health screening to verify that each individual is seeking services that the LMHA/LBHA is equipped to provide. If so, the individual then works with licensed staff to complete a full psychosocial and diagnostic standardized assessment — youth are given the Child and Adolescent Needs and Strengths (CANS) assessment and adults are given the Adult Needs and Strengths Assessment (ANSA). An adult client’s score on the ANSA is combined with a supplemental assessment specific to the individual’s diagnosis. For example, the Quick Inventory of Depressive Symptomology is used with individuals who have a diagnosis of major depression to determine appropriate level of care (LOC). For children, no supplemental assessments are used in conjunction with the CANS, thus the LOC is based solely on the child’s diagnoses and the score obtained from the CANS. Local authorities serve children ages 3 to 17 who have a mental health diagnosis and are at risk of being removed from their home or school or enrolled in special education services.
Individuals may also enter LMHA/LBHA services by first utilizing crisis services (via Mobile Crisis Outreach Teams, mental health deputies, or a crisis hotline). Once an individual is enrolled in LMHA/LBHA services, providers regularly update the CANS and ANSA to verify that the LOC is still appropriate. The state also tracks LOC changes over time to estimate how individuals are responding to treatment.
Individuals seeking substance use services are referred to Outreach Screening Assessment and Referral (OSAR) providers, which are often located within an LMHA/LBHA. More information on OSAR and substance use services can be found later in the Substance Use Services section of this guide.
Adult mental health services provided by LMHAs/LBHAs may include:
- Case management
- Medication management
- Counseling (Cognitive Behavioral Therapy and Cognitive Processing Therapy)
- Medication training and support
- Psychosocial rehabilitative services
- Skills training and development
- Peer support services
Child and Family services provided by LMHAs/LBHAs may include:
- Crisis intervention
- Skills training and development
- Counseling
- Supportive employment
- Medication training and support
- Case management
- Family partner support services
TEXAS RESILIENCY AND RECOVERY FRAMEWORK
The state’s vision for behavioral health services of “Hope, Resiliency, and Recovery for Everyone” aligns with a broader national movement to incorporate resiliency and recovery-based services, practices, performance measures, and beliefs into the public mental health system. The framework that guides HHSC’s public mental health service delivery is Texas Resiliency and Recovery (TRR), a shift in mental health service delivery from the disease-focused model to a person-centered approach. The TRR model relies on evidence-based practices and principles of recovery and resiliency to obtain the best possible outcomes and maximize the therapeutic impact of available resources.
The TRR system is responsible for:
- Establishing who is eligible for services through a uniform assessment (ANSA and CANS);
- Establishing methods to manage service utilization;
- Measuring clinical outcomes and impacts of services rendered; and
- Determining service cost.
Clinical needs are identified through a psychosocial assessment and a uniform clinical instrument. ANSA and CANS assessments are used to determine the appropriate LOC and corresponding eligibility for services and specialty treatments. Within this model, the intensity of services is based on an individual’s continuum of active symptoms and corresponding mental health needs. The expectation built into the model is that as a person’s strengths are identified and resilience is built, the majority of individuals transition to lower LOCs, and eventually into sustained recovery in the community. The TRR system empowers people toward their own recovery by building on their strengths rather than focusing on “fixing” their symptoms. Table 22 describes the adult target population and services provided at each TRR LOC. Table 23 describes the same for children and adolescents.
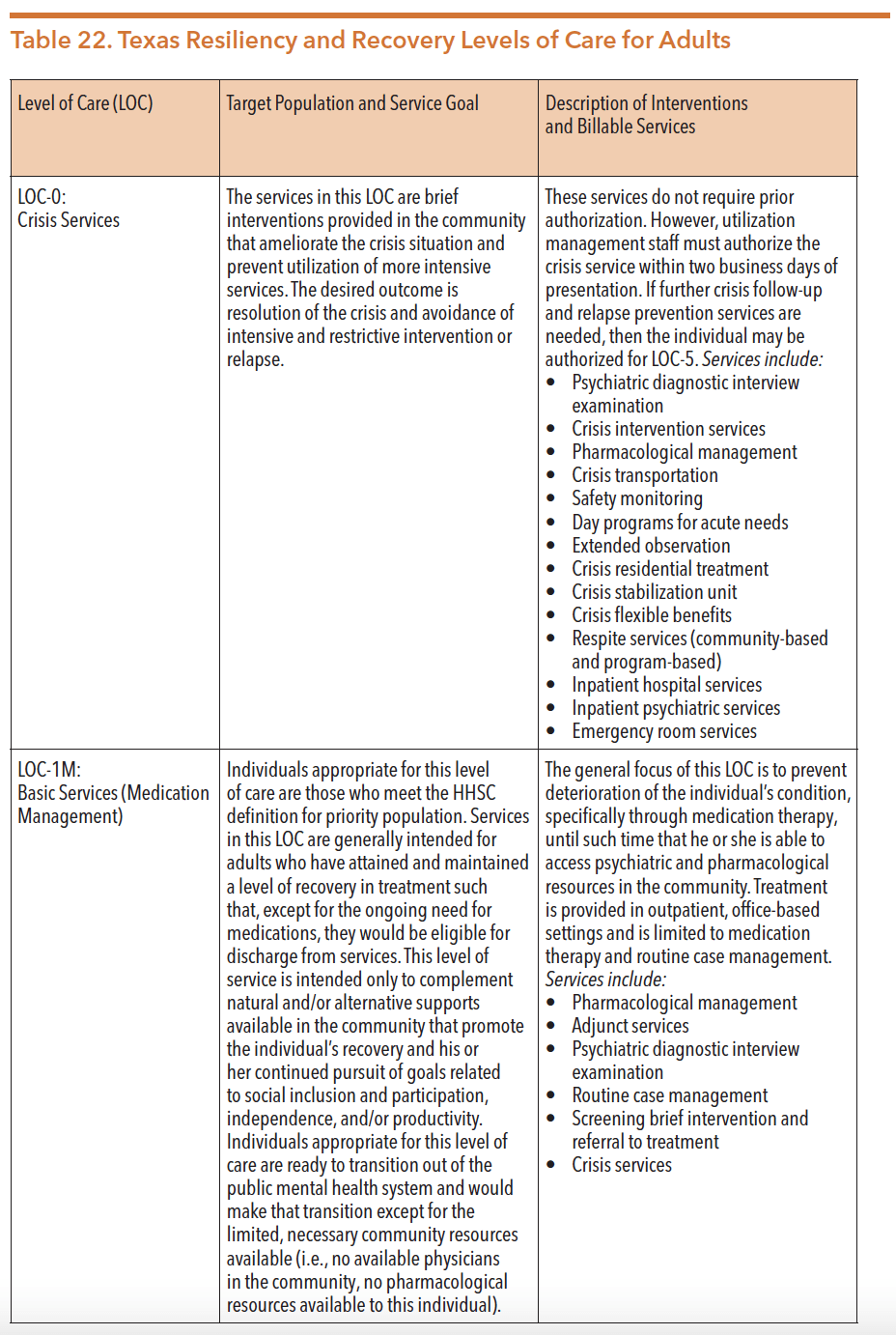
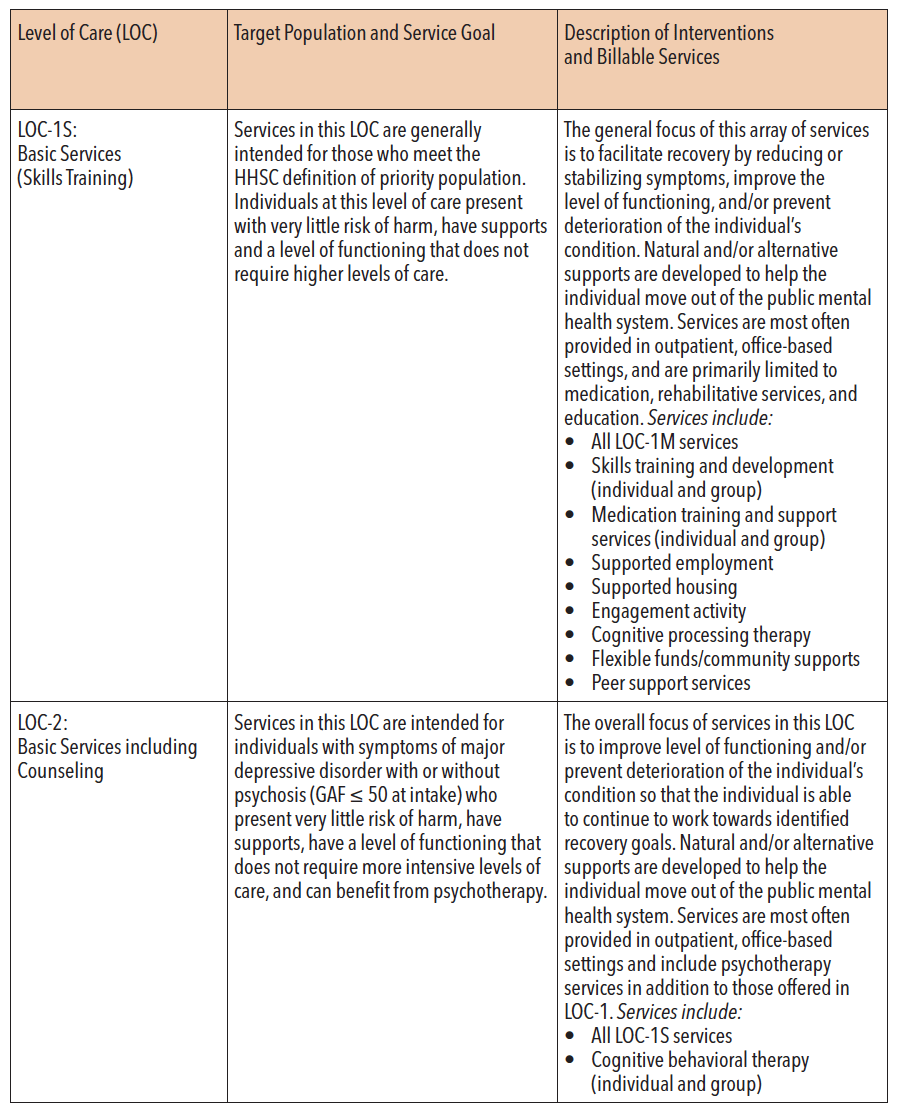
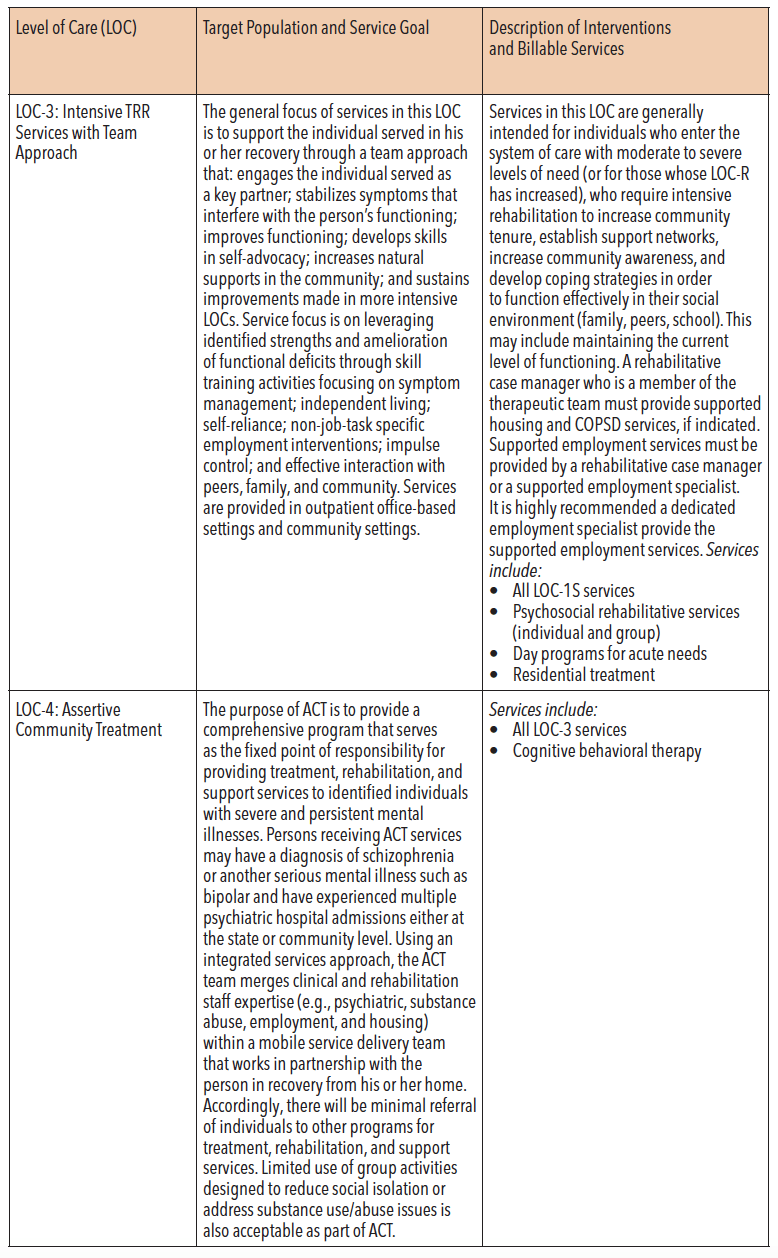
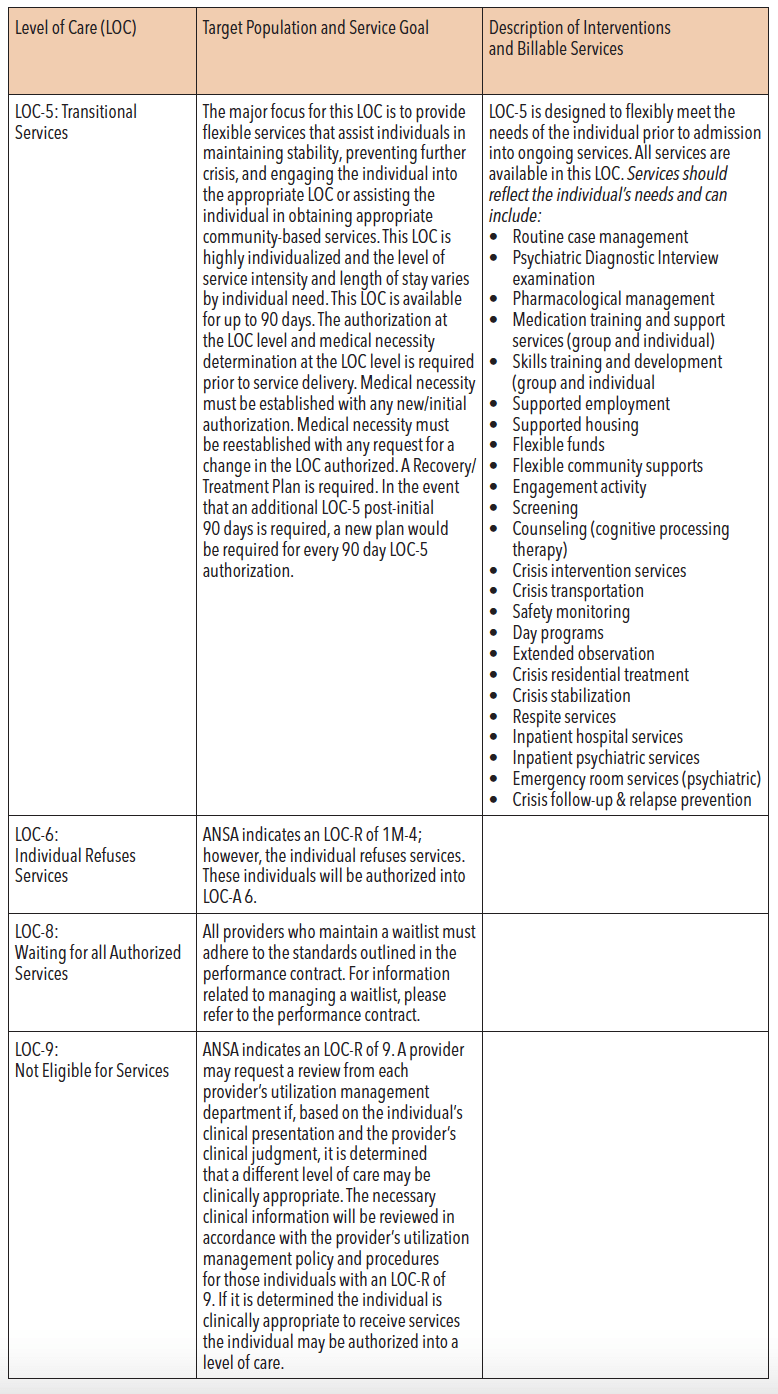
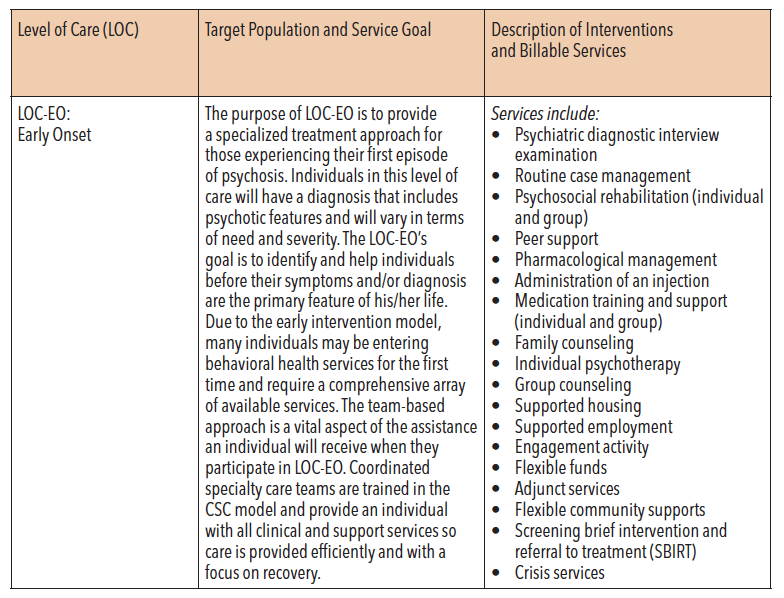
Source: Texas Health & Human Services Commission. (2017). Texas resilience and recovery utilization management guidelines: Adult mental health, effective April 2017. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/um-guidelines/trr-utilization-management-guidelines-adult.pdf
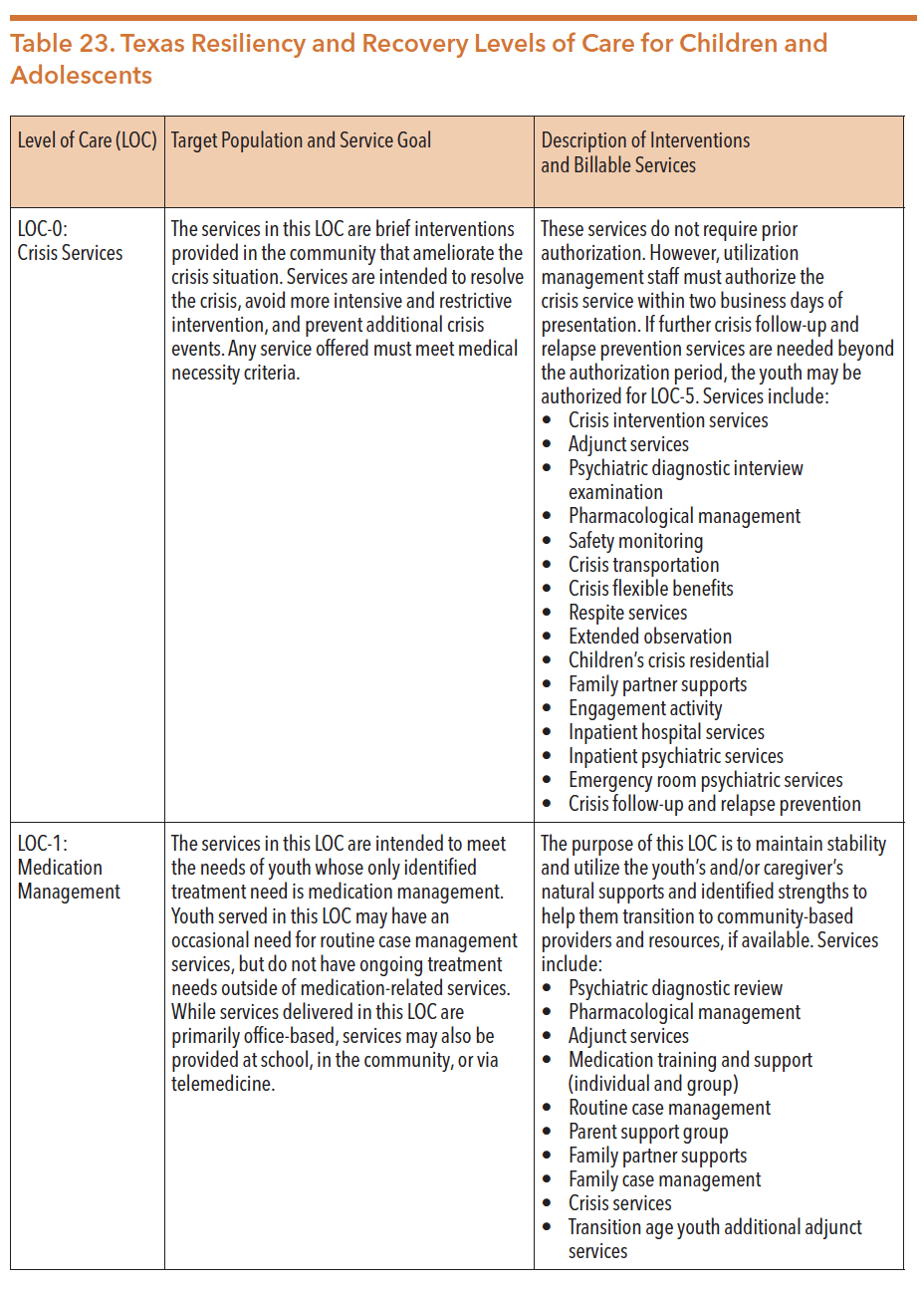
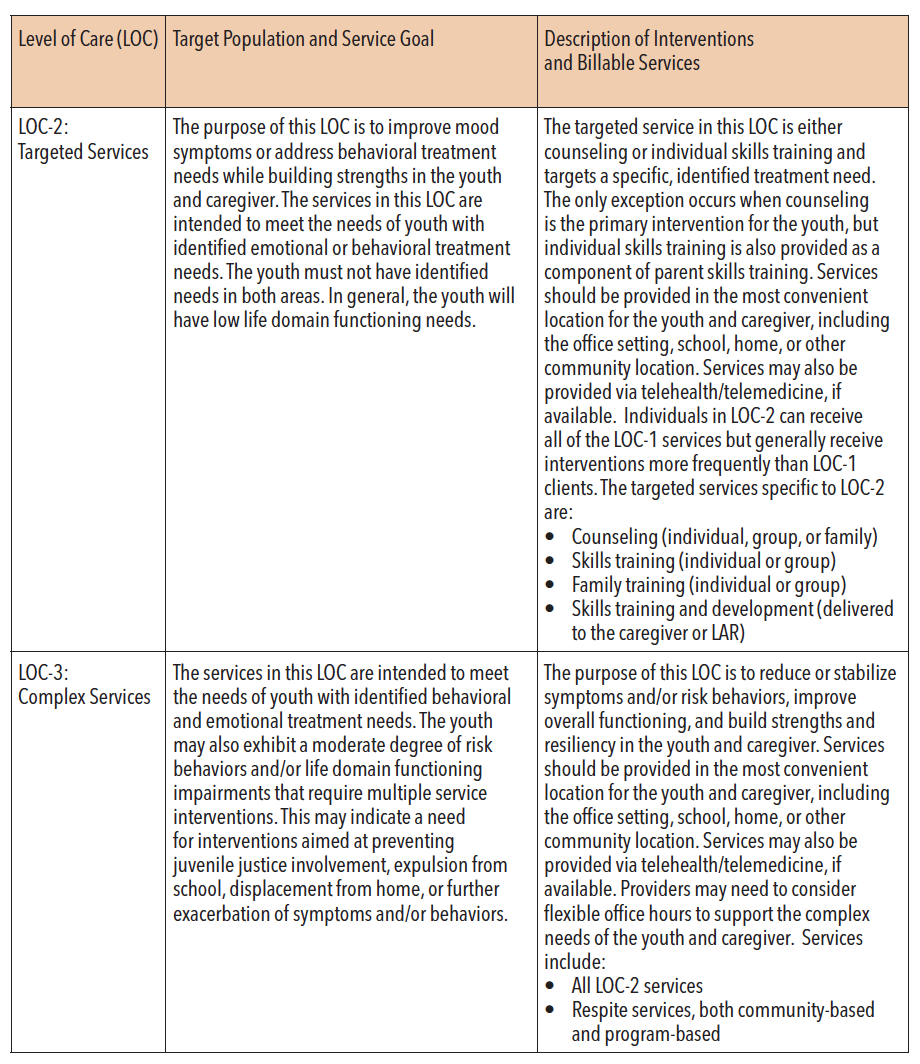
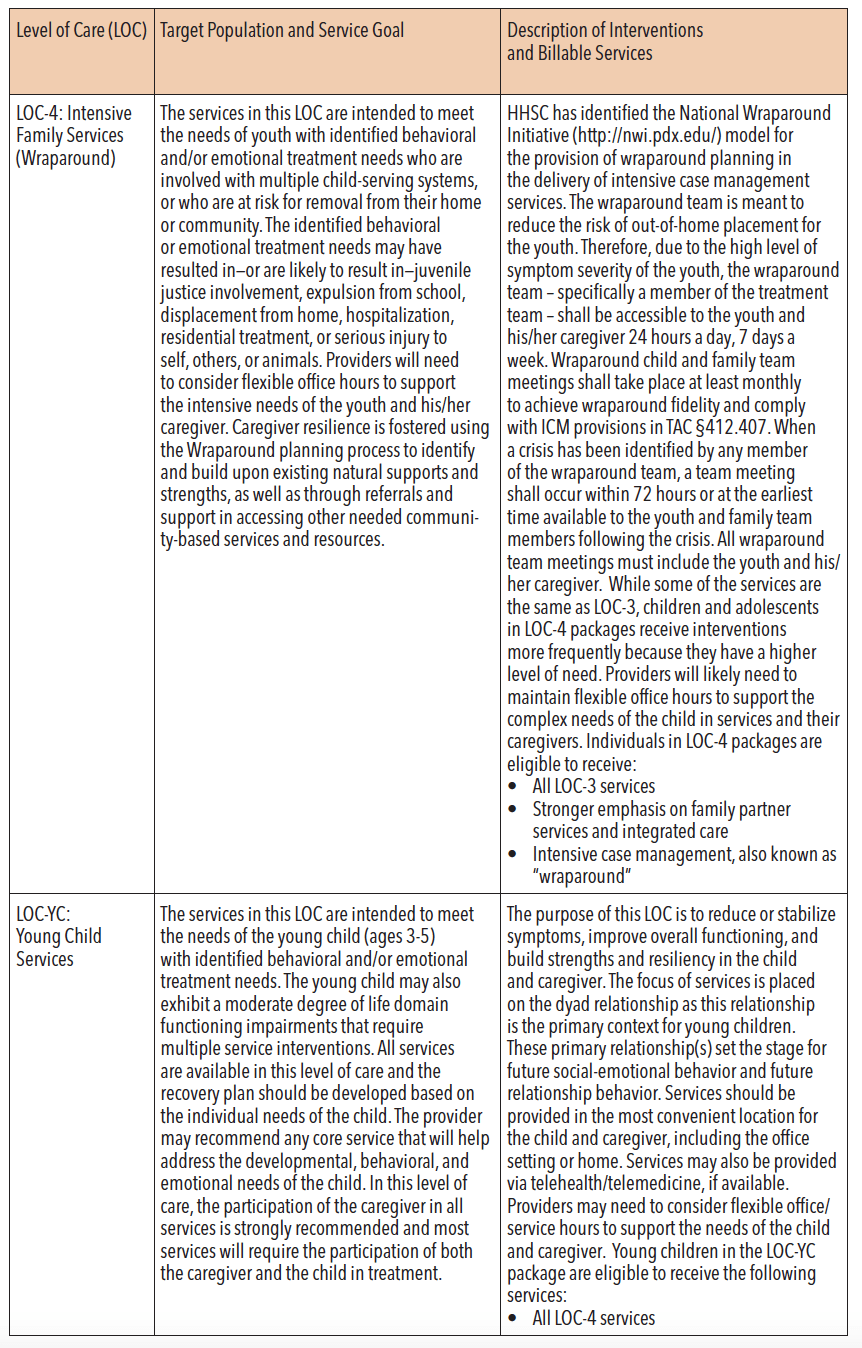
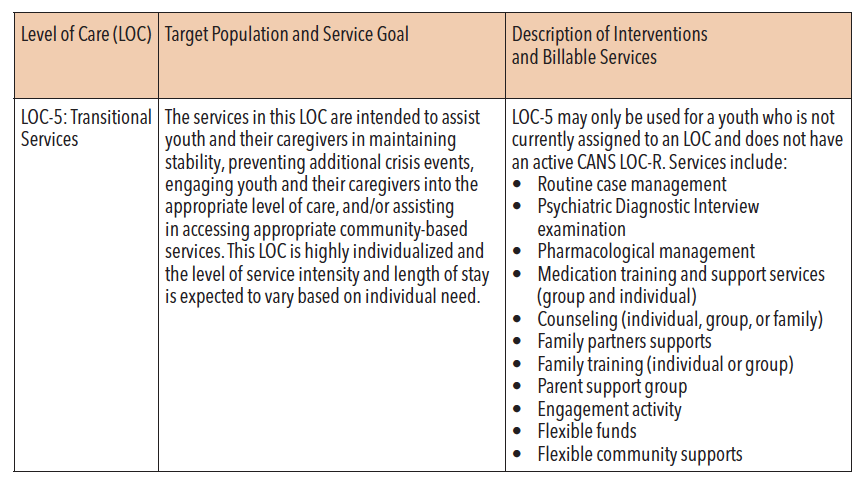
Source: Texas Health and Human Services. (2016). Texas resilience and recovery utilization management guidelines: Child and adolescent services, updated 2016. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/um-guidelines/trr-utilization-management-guidelines-child.pdf
TEXAS SYSTEMS OF CARE
Systems of care (SOC) is a spectrum of effective community-based services and supports for children, youth, and young adults who are experiencing, or at risk for mental health and related challenges, and their families. A SOC framework is also sensitive to the youth and their family’s cultural and linguistic preferences. This framework delivers highly individualized services such as wraparound and YES waiver supports to reduce youth admissions into hospitals, the juvenile justice system, and the child welfare system. Care for youth with intensive support needs is coordinated across state agencies, private and public organizations, and families so that children can overcome the barriers that prevent them from accessing the services they need.
HHSC and the Texas Institute for Excellence in Mental Health at the University of Texas at Austin lead the Texas System of Care, in collaboration with child-serving state agencies, family and youth advocacy organizations, and other stakeholders within the Texas children’s mental health service delivery system. The mission of the Texas System of Care is to “strengthen the collaboration of state and local efforts to weave mental health supports and services into seamless systems of care for children, youth and their families.” There are five state agencies that have entered into the Texas System of Care Memorandum of Understanding (MOU) depicted in Figure 38. Essentially, the MOU outlines strategies that each of the agencies can employ to integrate the system of care values and principles into their work. These strategies aim to create more family-driven, youth-guided, and culturally and linguistically responsive agencies.
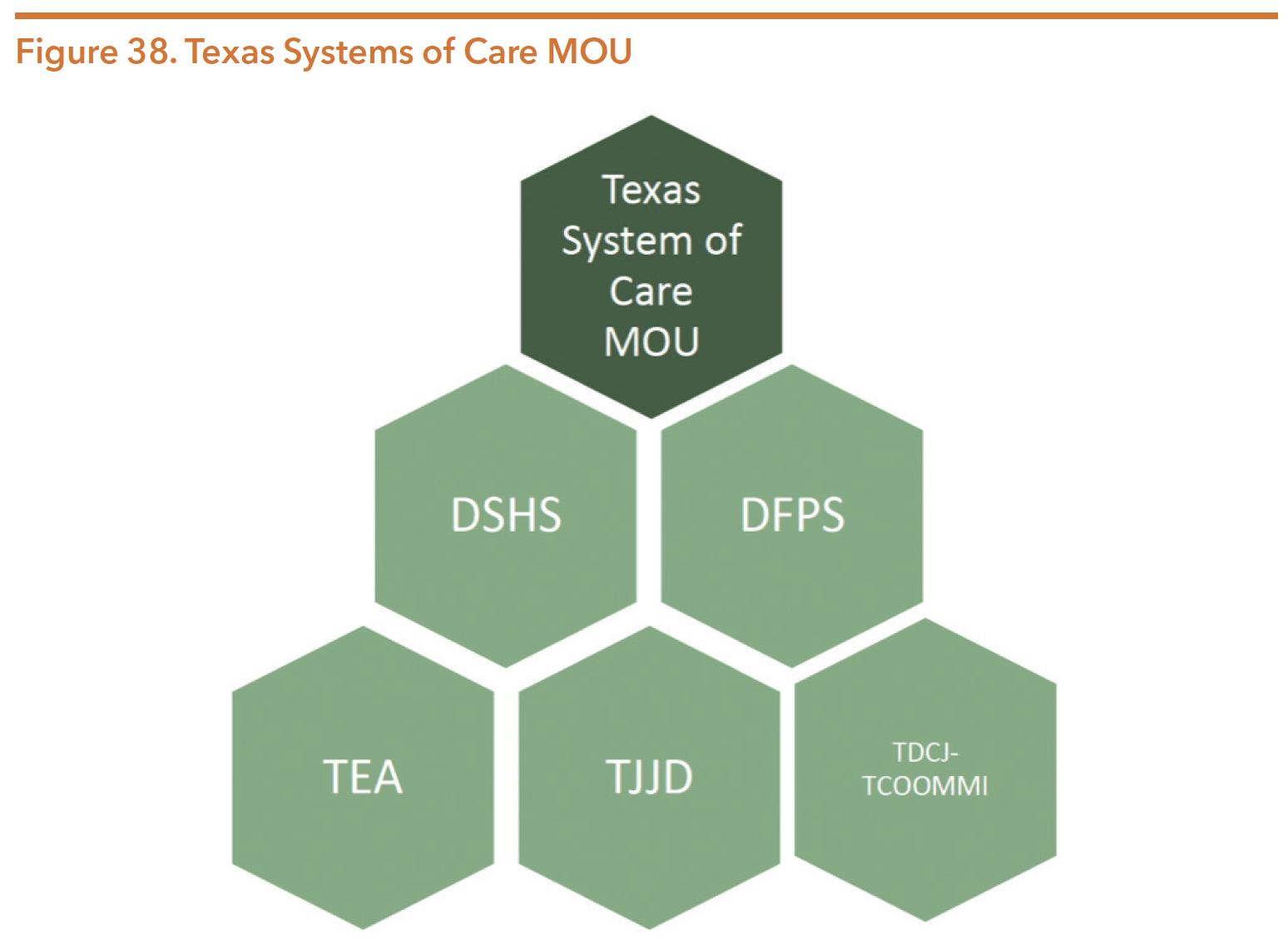
Source: Texas Health and Human Services, Statewide Behavioral Health Coordinating Council. (February 2019). Texas statewide behavioral health, fiscal years 2017-2021: Strategic plan update and the foundation for the IDD strategic plan. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2019/hb1-statewide-behv-hlth-idd-plan-feb-2019.pdf
In the early 2000s, the Texas legislature established the Texas Integrated Funding Initiative (TIFI). TIFI brought together many child- and youth-serving state agencies to provide systems of care grants to a handful of local communities. In 2011, the federal Substance Abuse and Mental Health Services Administration (SAMHSA) began granting HHS system of care grants across the country. Texas was a recipient of these grants to fund the development, planning, and implementation of a statewide and local systems of care plan. In 2017, Texas was awarded a four-year grant to further expand and sustain the System of Care framework across the state. The process and outcome evaluation for Year 1, including more information on work around the project’s goals and objectives, can be found at: https://txsystemofcare.org/ wp-content/uploads/2019/09/TxSOC-2-0-Evaluation-Report-Year-1-FINAL.pdf
HHSC currently contracts with LMHAs to oversee the implementation of systems of care in local communities. As of March 2020, Burke in East Texas and LifePath Systems in Collin County were participating in the Texas Systems of Care framework. In 2019, HHSC conducted a Needs and Capacity Assessment to identify two additional Texas System of Care communities. Through that process, the Harris Center in Harris County and Coastal Plains Community Center in the Gulf Coast region were selected and began implementation on September 30, 2019.
COMMUNITY MENTAL HEALTH SERVICES
A majority of community mental health services focus on outpatient community-based services designed to support adults’ movement toward independence and recovery, as well as support the recovery and resilience of children and their families. These services include medication-related services, rehabilitation services, counseling, case management, peer support services, family support services, crisis intervention services, and special programs such as Clubhouses.
According to HHSC, “over the past decade, LMHAs have been challenged to meet the growing demand for community-based outpatient mental health services. At the beginning of fiscal year 2012, over 7,000 adults and children were waiting for services. In each of the following three biennia, the Legislature made significant investments to expand outpatient capacity. This funding supported a steady expansion of services and in the past four years, tens of thousands of individuals have been brought into service.”
However, even with the continued investments, only 69 percent of adults with SMI and 58 percent of children with SED that HHSC estimates are eligible for services were enrolled in services. Over the next biennium, an estimated 9,085 new residents will be added to the population of indigent individuals needing long-term mental health services. Timely access to care is essential; data show that individuals who wait more than 30 days for service are unlikely to be admitted to care. Fortunately, individuals who are linked with appropriate and timely services are less likely to be incarcerated or admitted to inpatient services.
During the 86th legislative session, lawmakers increased both adult and children community mental health funding to a total of $948,735,798 in the 2020-2021 biennium, an increase of $78,999,358 from the 2018-2019 biennium.
Priority Populations
During the 83rd Legislative session, HB 3793 (83rd, Coleman/Hinojosa) amended the Health and Safety Code to expand access to community mental health services to individuals with a variety of mental health conditions. Although providing treatment services to individuals with other diagnoses was not prohibited prior to 2013, the law had previously mandated the provision of services only to adults with the “big three diagnoses”: schizophrenia, bipolar depression and major depressive order.126 As a result of HB 3793, LMHAs/BMHAs with sufficient resources can provide services for individuals with any of the diagnoses listed in Table 24. Despite this change in code to allow for more individuals served, LMHAs continue to provide services primarily for adults with schizophrenia, bipolar, or major depression with psychosis due to funding constraints. During FY 2017, 95 percent of diagnoses for adult clients in ongoing treatment related to one of these diagnoses.
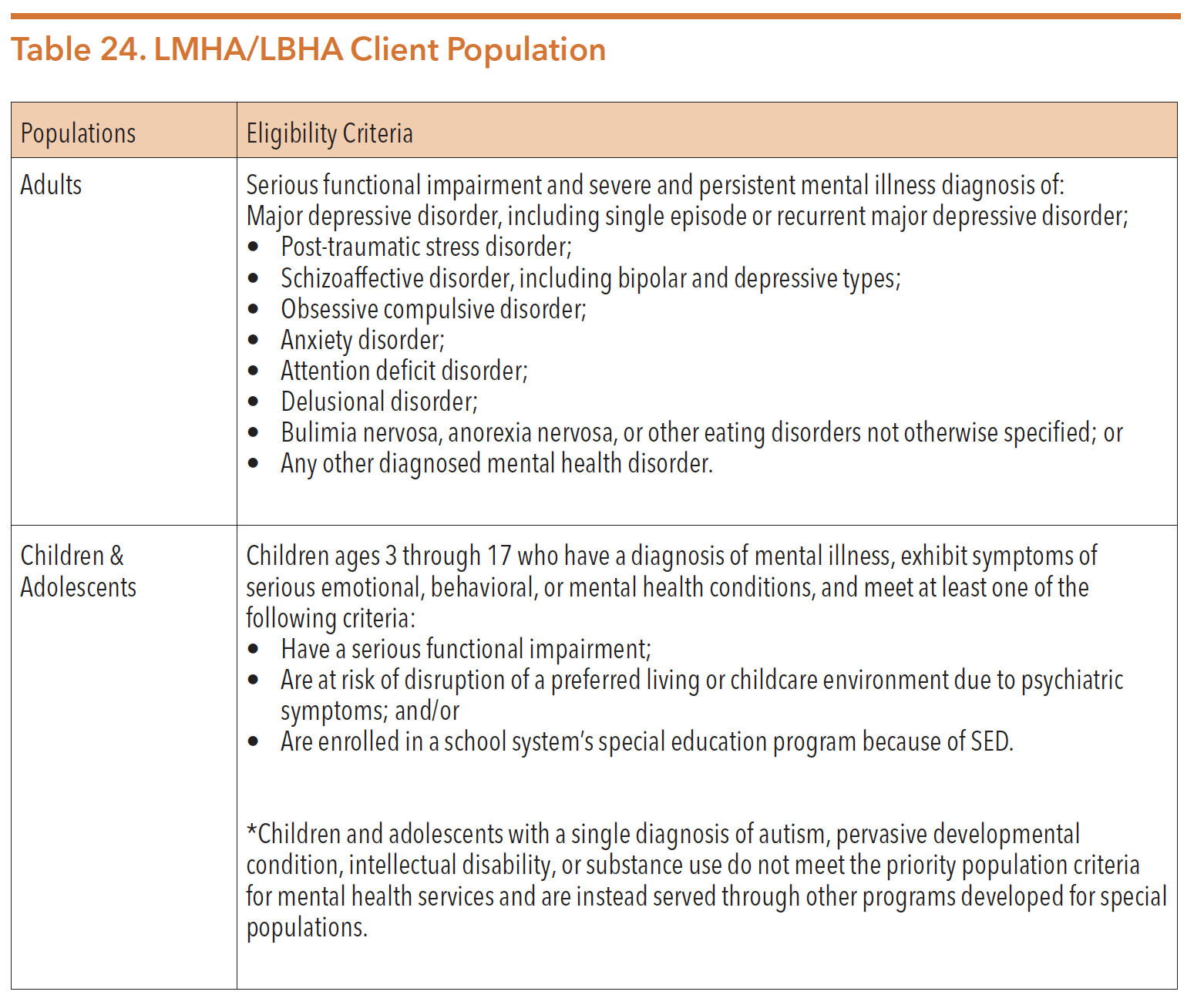
Sources: Texas Legislature Online. (2013). House Bill 3793. Retrieved from http://www.capitol.state.tx.us/BillLookup/History.aspx?LegSess=83R&Bill=HB3793
Texas Legislature Online. (2013). Senate Bill 7. Retrieved from http://www.capitol.state.tx.us/BillLookup/History.aspx?LegSess=83R&Bill=SB7
System Utilization
From FY 2013 through FY 2017, the average monthly number of adults receiving community mental health services through LMHAs increased steadily, reaching 117,792. However, during the next two years, the average monthly number dropped to 89,752. The average number of children receiving community mental health services also increased during FY13 through FY 2017, but like adults being served, the number of children declined over the following two years. Table 25 shows trends for the number served and the average cost per client from 2013-2019.
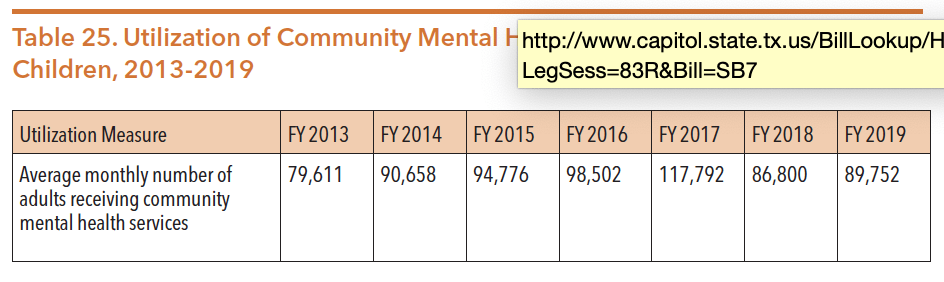
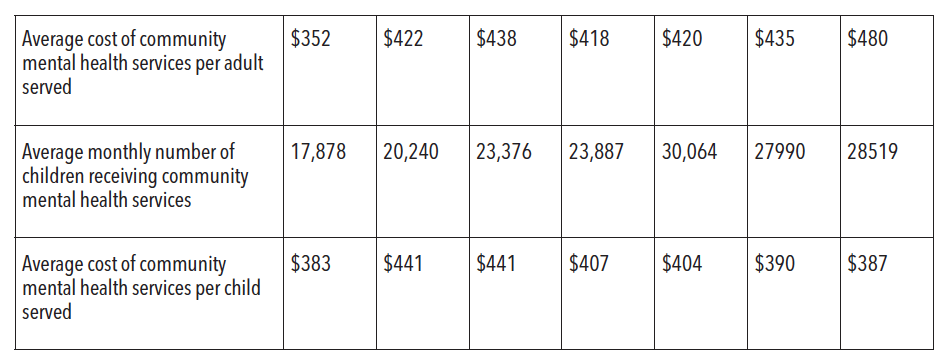
Sources: Texas Health & Human Services Commission. FY 13-17 Data request August 8, 2018. Data received from Michele Neal.
Texas Health & Human Services Commission. FY 18-19 Data Request. Data request May 20,2020. Data received from Sonja Gaines.
As illustrated in the figures below, there are significantly more adults and children in Texas who require mental health services than are currently being served in the public mental health system. The most recent data from FY 2018 illustrates that there were 291,881 adults in Texas who had a serious mental illness (SMI) and were living below 200 percent of the FPL; 202,722 of them—69.5 percent—received services at HHSC-funded community mental health centers. Similarly, there were 113,011 children with serious emotional disturbance (SED) living below 200 percent of the FPL in 2018; 66,216 of them—or 58.6 percent—received services through HHSC-funded community mental health centers.
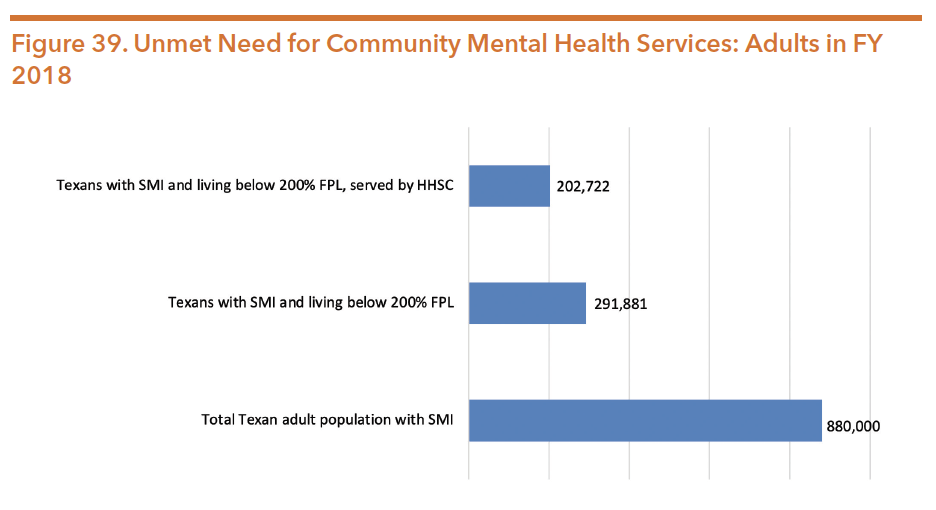
Sources: Texas Health and Human Services Commission. Data Request. Data request May 20, 2020. Data received from Sonja Gaines
Texas Health and Human Services, Statewide Behavioral Health Coordinating Council. (February 2019). Texas statewide behavioral health, fiscal years 2017-2021: Strategic plan update and the foundation for the IDD strategic plan. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2019/hb1-statewide-behv-hlth-idd-plan-feb-2019.pdf
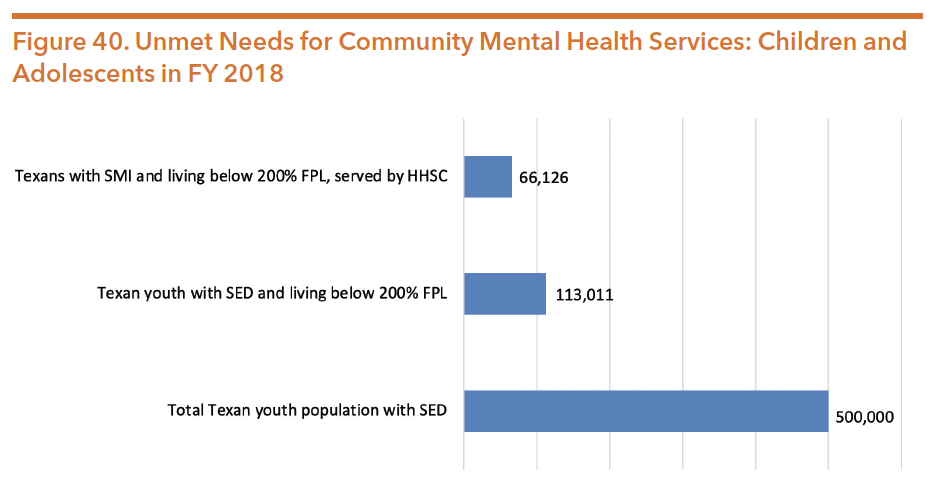
Sources: Texas Health and Human Services Commission. Data Request. Data request May 20, 2020. Data received from Sonja Gaines
Texas Health and Human Services, Statewide Behavioral Health Coordinating Council. (February 2019). Texas statewide behavioral health, fiscal years 2017-2021: Strategic plan update and the foundation for the IDD strategic plan. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2019/hb1-statewide-behv-hlth-idd-plan-feb-2019.pdf
Quality of Care Measures
Table 26 and Table 27 shows selected data on common adult and child/adolescent outcome measures for FY 2016-2019.
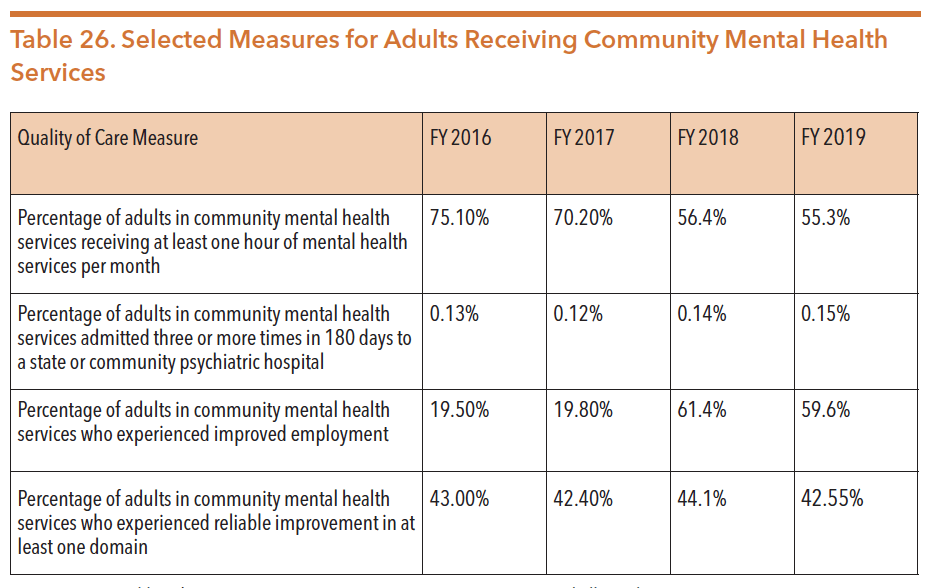
Sources: Texas Health and Human Services Commission. FY16-17 Data request: Michelle Neal, August 8, 2018.
Texas Health and Human Services Commission. FY 18-19 Data Request. Data request May 20,2020. Data received from Sonja Gaines.
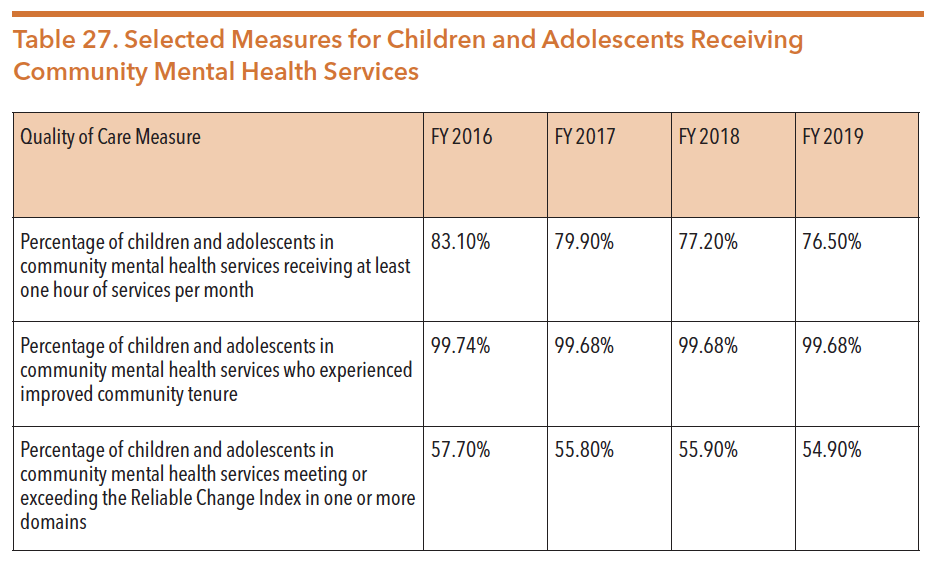
Sources: Texas Health and Human Services Commission. FY 16-17 Data request: Michelle Neal, August 8, 2018.
Texas Health and Human Services Commission. FY 18-19 Data Request. Data request May 20,2020. Data received from Sonja Gaines.
Waitlists
When LMHAs exhaust their funding, non-Medicaid eligible individuals who require mental health services are added to a waitlist. Individuals who are on Medicaid must be admitted into services because federal law prohibits waitlists for Medicaid. As of April 2020, 172 adults were “waiting for all services,” and 1,043 underserved adults were waiting for additional services.
On the other hand, in April 2020 there were no eligible children waiting for services and 155 underserved children waiting for additional services.
The factors identified by LMHAs as impacting waiting lists are shown in Table 28.
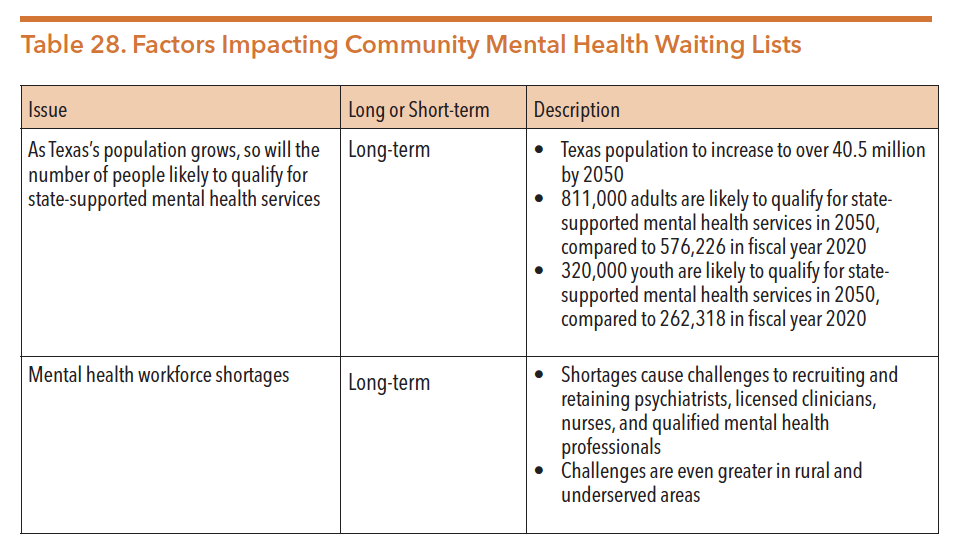
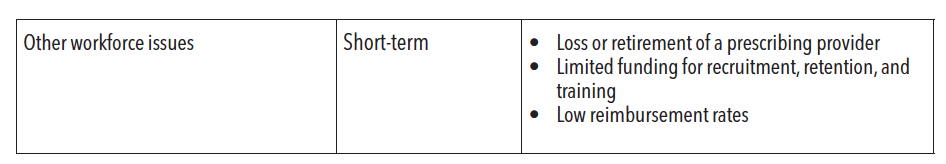
Source: Texas Health and Human Services Commission. (2020). Semi-annual reporting of waiting lists for mental health services. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/hb1-semi-annual-waiting-lists-mhs-april-2020.pdf
Factors contributing to the ongoing waitlists for mental health services include the growing Texas population, significant mental health workforce shortages (especially in rural areas), and low reimbursement rates for mental health providers.
The 86th Legislature appropriated additional funding of approximately $59 million specifically to address the waiting lists for adult and children’s services to avoid future wait lists and increase outpatient treatment capacity at LMHAs/LBHAs.
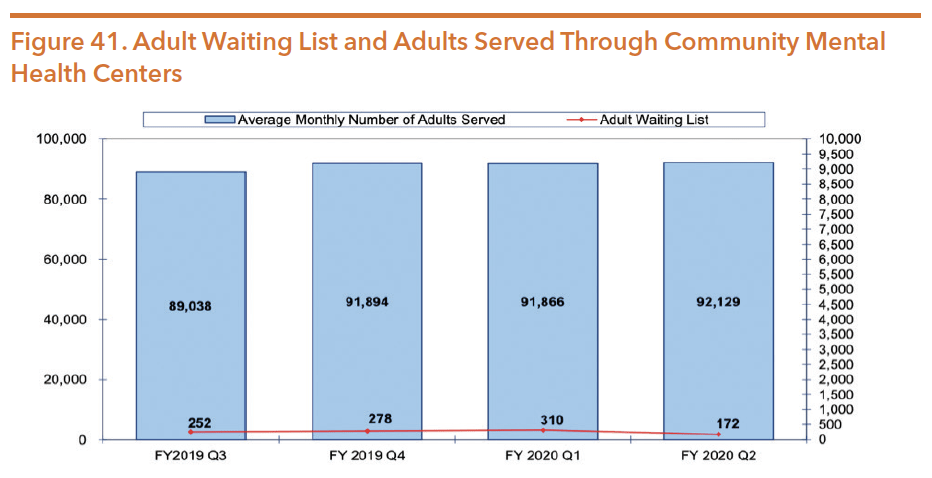
Source: Texas Health and Human Services Commission. (2020). Semi-annual reporting of waiting lists for mental health services. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/hb1-semi-annual-waiting-lists-mhs-april-2020.pdf
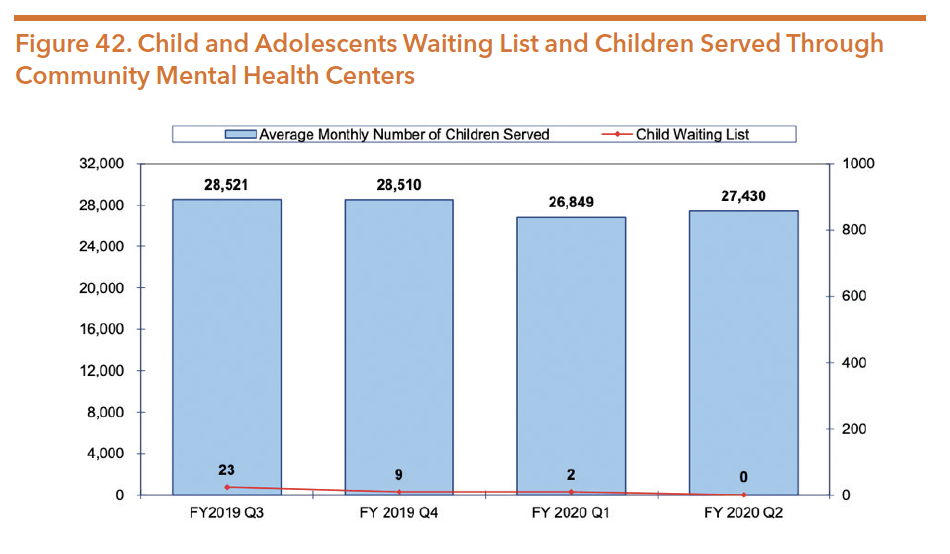
Source: Texas Health and Human Services Commission. (2020). Semi-annual reporting of waiting lists for mental health services. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/hb1-semi-annual-waiting-lists-mhs-april-2020.pdf
Youth Empowerment Services (YES) Waiver
The YES Waiver is a Medicaid 1915(c) home and community-based waiver program for children ages 3 to 18 years old who have serious mental, emotional, and behavioral difficulties (including serious emotional disturbance or SED), are at risk of being removed from their home due to a mental health concern, and meet the requirements to be in a psychiatric hospital. A full range of Medicaid services, non-traditional services, and family supports are available to create an intensive, comprehensive, and individualized child and family plan of care. As with other 1915(c) waivers, YES waivers do not take family income into account when determining eligibility. With all Medicaid 1915(c) waivers, the individual may gain Medicaid eligibility as a result of receiving waiver services. They may not meet standard Medicaid eligibility, but if they meet waiver financial eligibility (up to 200 percent of FPL), they are eligible for the waiver which makes them eligible for Medicaid.
The YES waiver program offers an alternative to inpatient treatment by providing community-based coordinated care for youth with particularly complex or severe behavioral health needs. The program uses a wraparound approach that combines direct services with family supports to help the child stay safely within their community. The average length of time services are delivered is typically 11-18 months, but can be extended if there is still clinical need for the services provided. As with traditional Medicaid, YES waiver services are jointly funded by the state and the federal government.
HHSC contracts with LMHAs to manage YES waiver services in each of their respective service regions. Table 29 shows the capacity of each LMHA across the state.
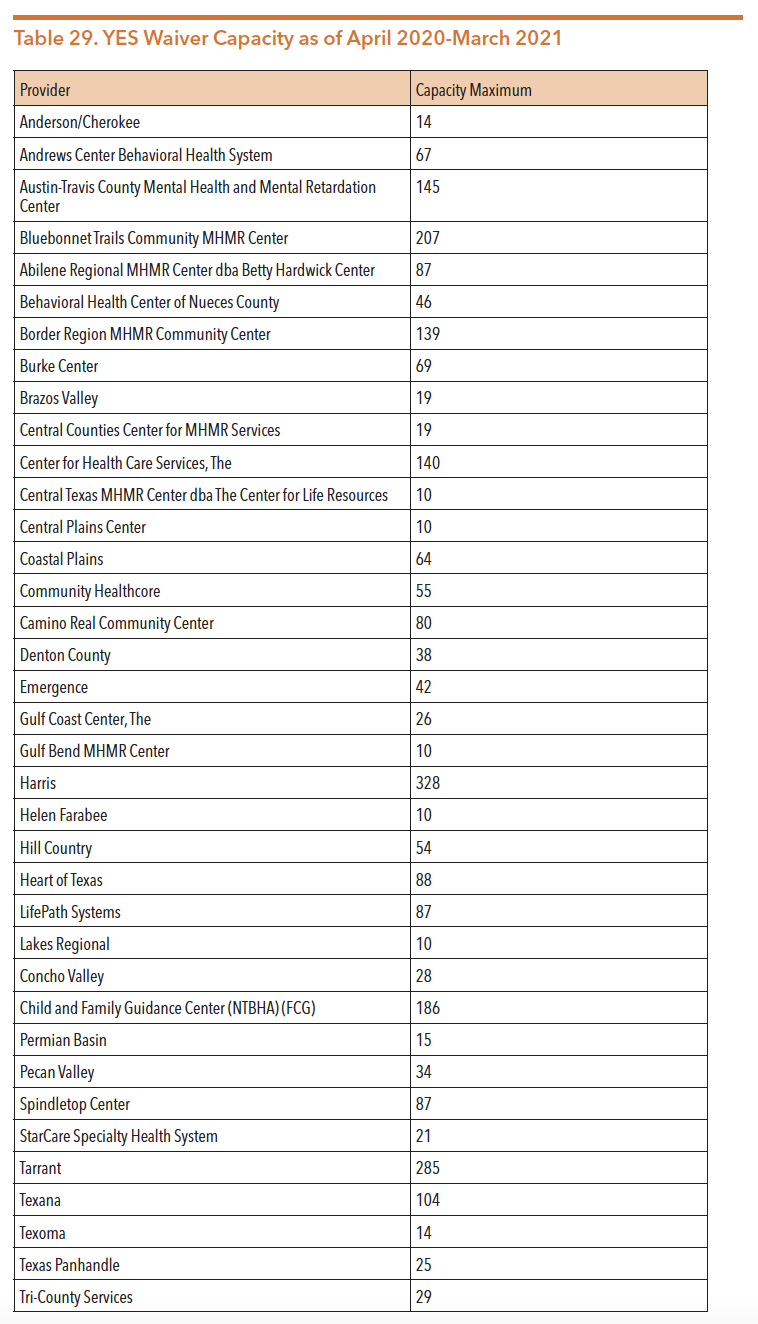
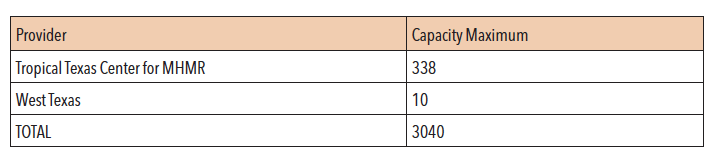
Source: Texas Health and Human Services. (April 2020). YES Waiver data. Retrieved from https://hhs.texas.gov/about-hhs/records-statistics/data-statistics/yes-waiver-data
LMHAs contract with community service providers to ensure all required YES waiver services are available, though some are utilized and provided at much higher rates than others, while some are not yet utilized as depicted in Figure 43. Utilization and access to services depends on what is available across the state, leaving some rural and underserved areas with fewer offerings. Services offered through the YES waiver program include:
- Comprehensive case management
- Adaptive aids and supports
- Community living supports
- Family supports
- Minor home modifications
- Non-medical transportation
- Professional and paraprofessional services
- Respite
- Supportive family-based alternatives
- Transitional services
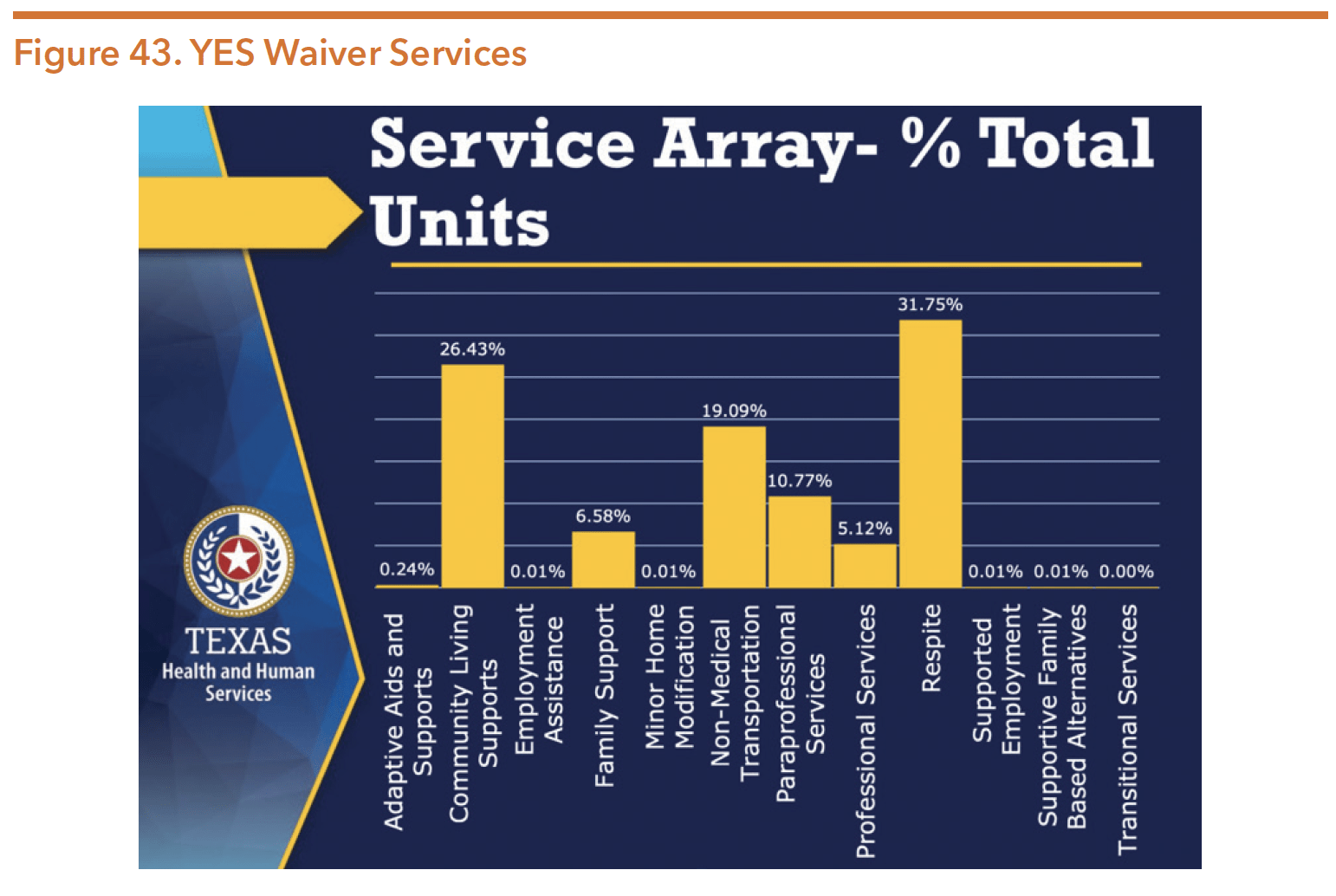
Source: Texas Health and Human Services Commission. (2018). Youth empowerment services waiver data dashboard February 2018. Retrieved from https://hhs.texas.gov/sites/default/files/documents/about-hhs/records-statistics/research-statistics/yes-waiver/yes-data-dashboard-feb-2018.pdf
The YES waiver program was approved for statewide expansion during the 84th legislative session through Rider 60. Table 30 shows the steady increase in YES waiver enrollments over the past seven years.
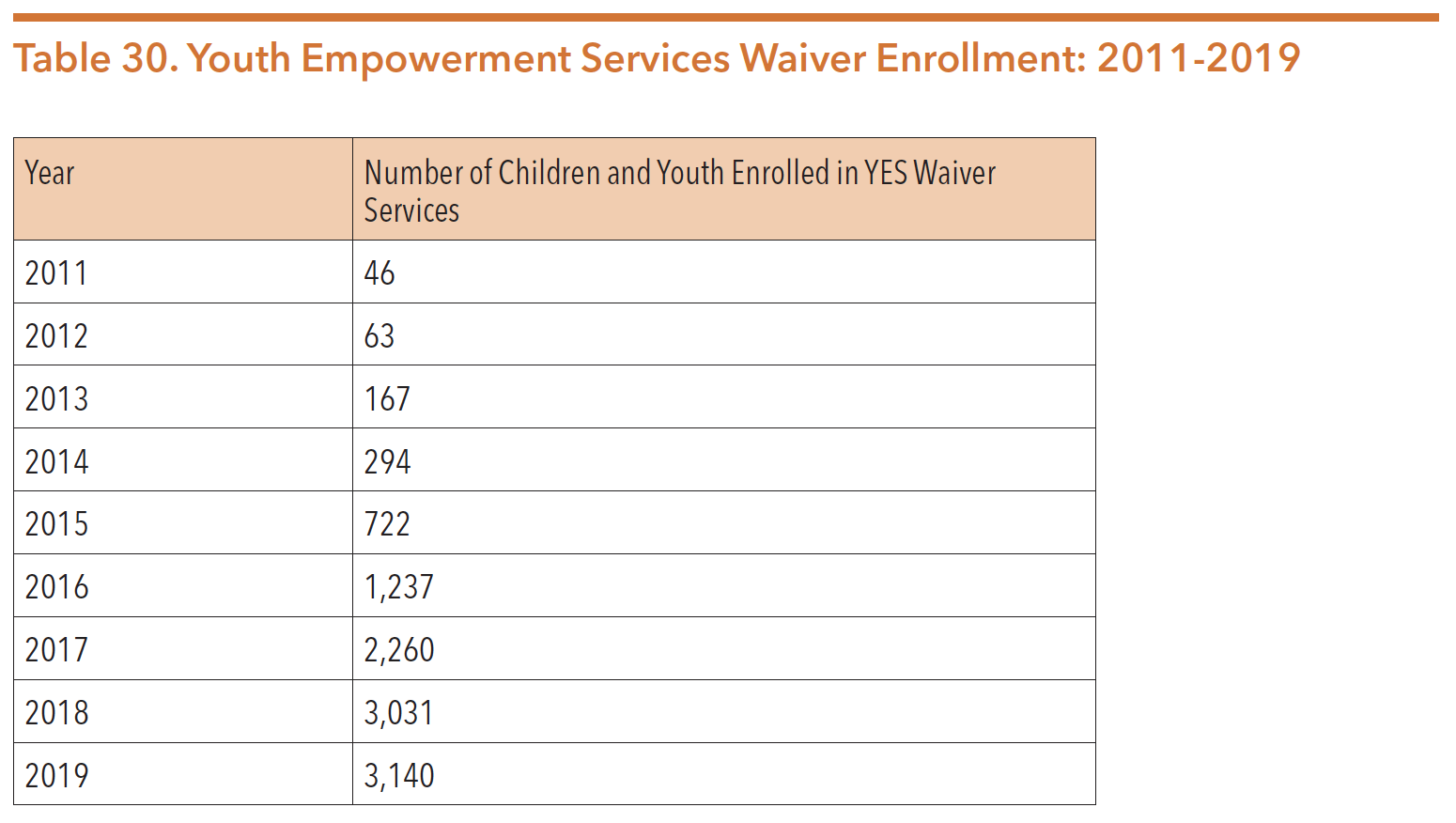
Sources: Lewis, L., & Jesse, G. (March 22, 2016). Presentation to the Select Committee on Mental Health: Children’s mental health services. Texas Department of State Health Services. Retrieved from http://www.dshs.texas.gov/WorkArea/linkit. aspx?LinkIdentifier=id&ItemID=8590006580.
Texas Health and Human Services Commission. (April 16, 2018). FY 2017 data stakeholder meeting.
Texas Health and Human Services Commission. FY 18-19 Data Request. Data request May 20,2020. Data received from Sonja Gaines.
The expansion of the YES waiver program should allow more youth with SED to access intensive community behavioral health services in effort to decrease the number of children who receive inpatient care and/or are relinquished to the DFPS solely because of an inability to access needed mental health services. However, due to a high need and specific number of allocated waiver slots for regions across the state, individuals must call their LMHA to be added to the YES Waiver inquiry list. HHSC determines the vacancy allocations based on population size, community, need, and local infrastructure. HHSC re-evaluates allocations at least annually, or more often as needed. Areas with greater service demands receive unused vacancies from other areas.
In February 2016, DSHS required that children at “imminent risk” of being relinquished to the state be prioritized for YES waiver services. The YES waiver sets aside a reserve of five percent of waiver slots specifically for these children.138 In recent years, the YES waiver was amended to allow children who are in state conservatorship (in foster care through DFPS) to be eligible to receive YES waiver services.
More information on the YES Waiver can be found at: https://hhs.texas.gov/services/ mental-health-substance-use/childrens-mental-health/yes-waiver.
Supportive Housing Rental Assistance Program
Since 2013, the Supportive Housing Rental Assistance (SHR) program has provided short- and long-term rental and utility assistance to individuals who are experiencing homelessness or who at risk of homelessness. Through the program, these individuals receive services at one of 20 LMHAs. SHR funds can be used for various assistance including rent, utilities, deposits and other move-in expenses. To qualify, individuals must be working with their case manager to apply for permanent housing vouchers and create an income stability plan. In FY 17-18, $11.6 million in GR funds was allocated to the program, which provided services to 2,119 people in FY 2018.
In FY 2018, after receiving SHR assistance, recipients experienced a 57 percent reduction in the average number of psychiatric hospitalizations and a 48 percent reduction in the number of crisis encounters. Additionally, after receiving SHR assistance recipients experienced a 39 percent reduction in criminal justice involvement and an overall 79 percent reduction in homelessness. Table 31 summarizes outcomes of the SHR program during FY 17-18.
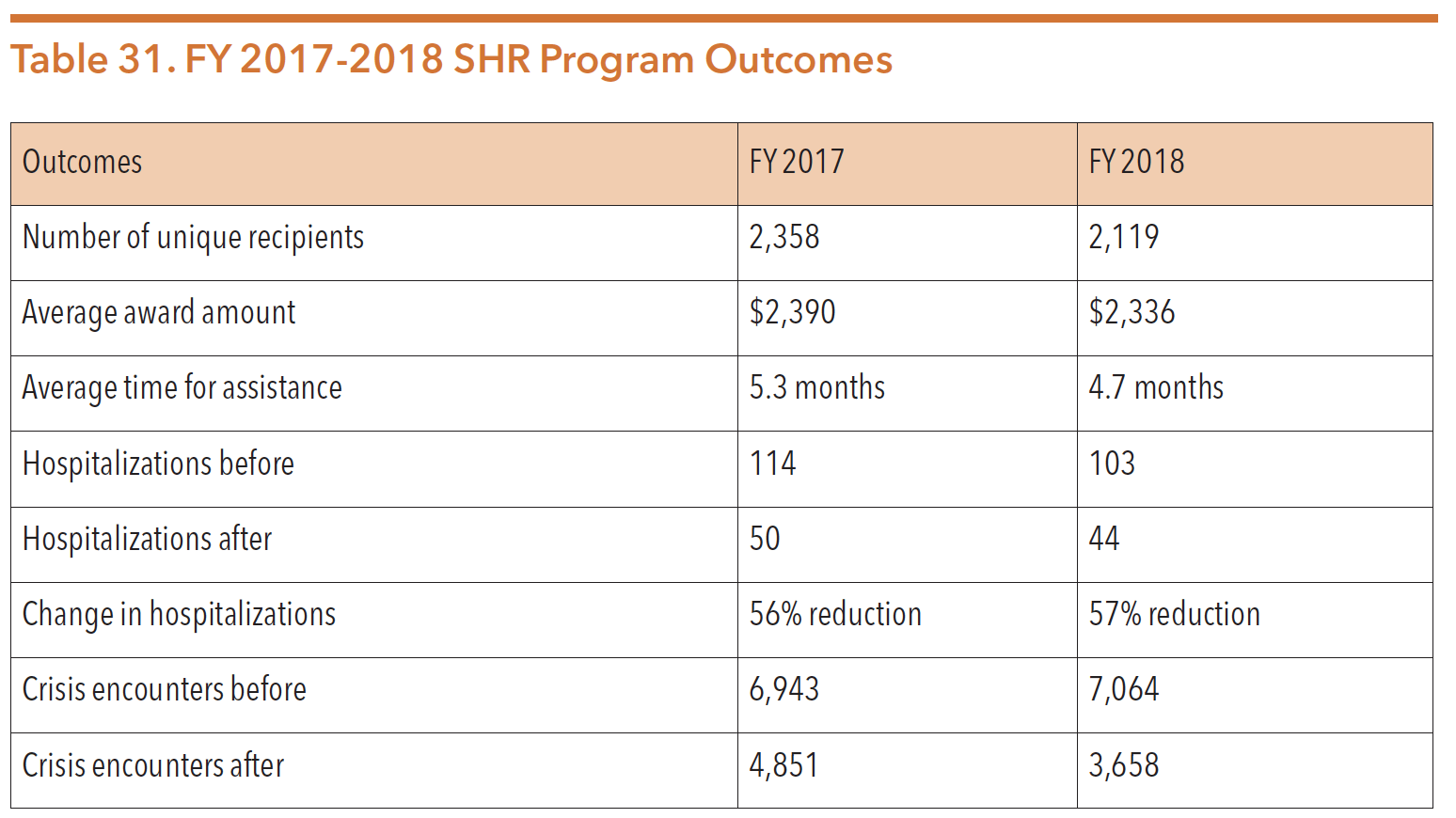
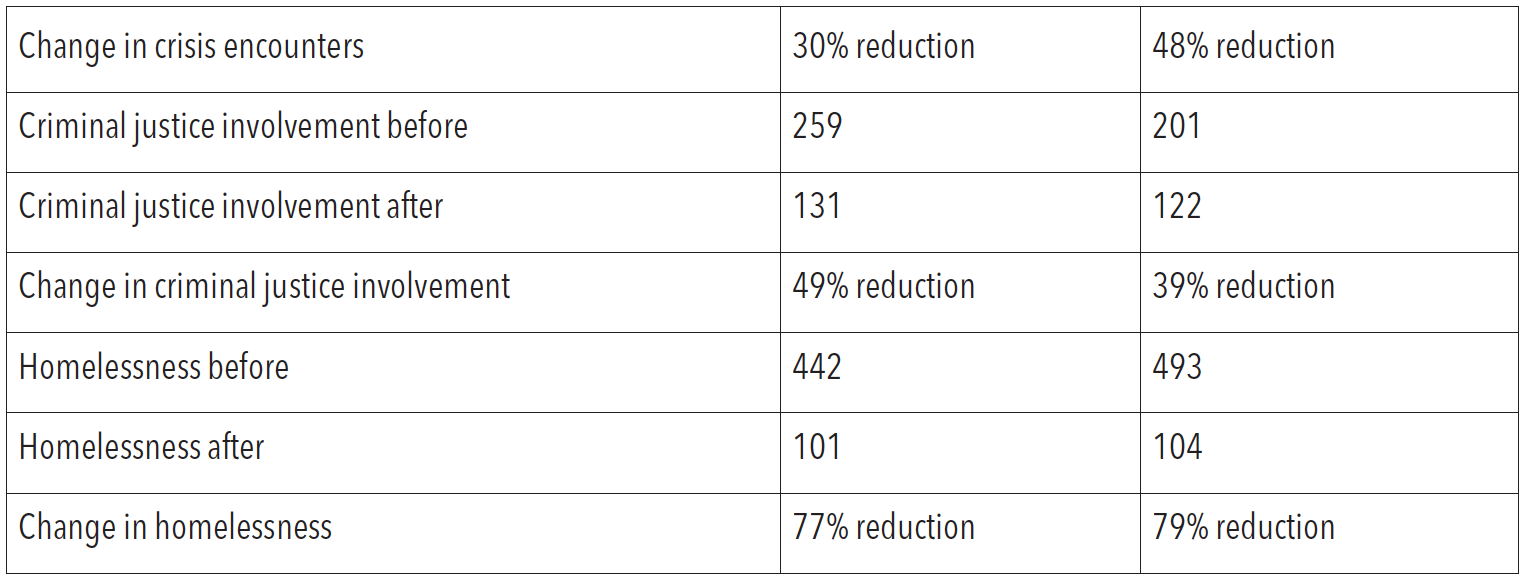
Source: HHSC information request, Feb. 21, 2019
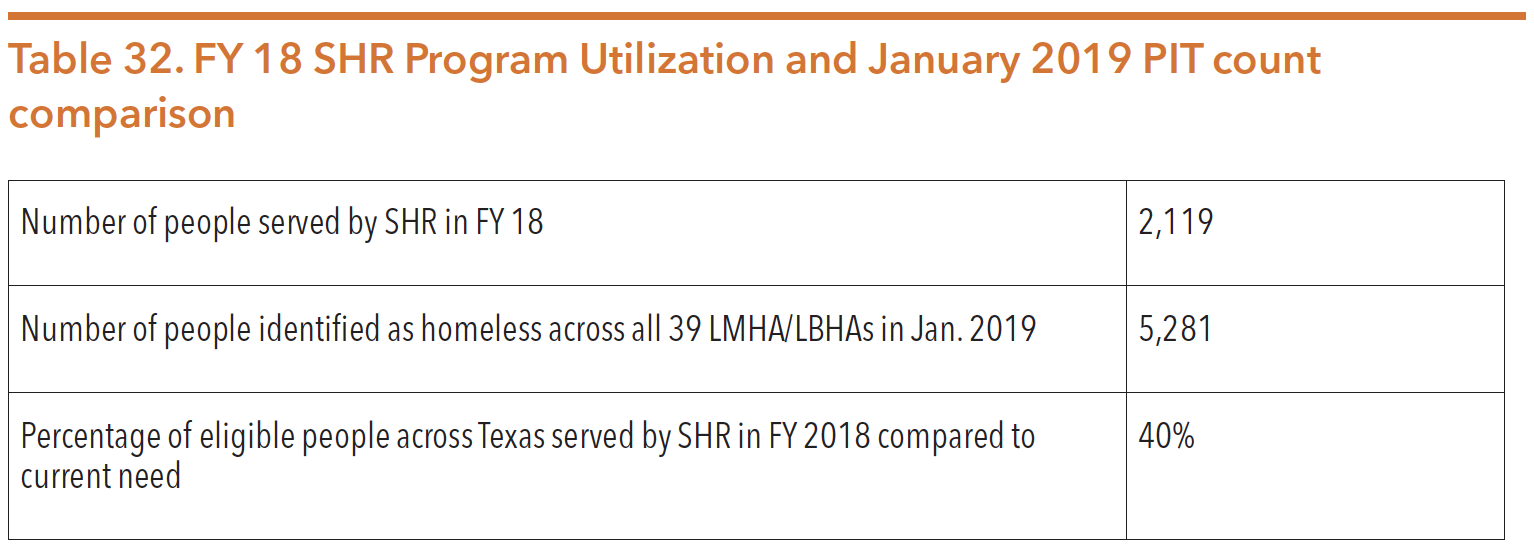
Source: HHSC information request, Feb. 21, 2019
Peer Services Programs, Planning, and Policy Unit
Mental health and substance use peer support services are critical to supporting the recovery of many people with mental health and/or substance use conditions. HHSC has illustrated the importance of these services by creating the Peer Services Programs, Planning, and Policy Unit within the commission. The unit’s first Director of Peer Services, Noah Abdenour, launched the unit in February 2019. The unit now includes the director, five program specialists, and an administrative assistant. Creation and development of this unit was a significant advancement in validating the importance of these services.
Peer Services
According to HHSC, “peer support is when someone with lived experience gives encouragement and assistance to help someone with mental illness or a substance use condition achieve long-term recovery. Peers offer emotional support, share knowledge, teach skills, provide practical assistance, and connect people with resources, opportunities and communities of support.”
A peer is a person with lived experience of recovery from mental health and/or substance use conditions. By combining this experience with skills learned in formal training, peer specialists (e.g., certified peer specialist, peer support specialist, recovery coach) deliver services in behavioral health settings to support long-term recovery. Peer support is non-clinical and recovery focused, and often works on a team with other mental health professionals. While peer support is a deliverable service, it is not a provider type. Peer specialists can be found in LMHAs/LBHAs, peer run service providers, state hospitals, community-based organizations, recovery organizations and treatment organizations. Common tasks performed by peer specialists include helping people self-advocate, connecting people to resources and work, goal setting, facilitating support groups, outreach and engagement, face-to-face recovery coaching, and telephone peer support.
Peer support is becoming more widely recognized as an important support service for individuals with mental health and substance use conditions. As these services are more widely available and utilized, so is the data on impact and cost savings. Current evidence suggests that peer support and recovery coaching:
- Reduces the admissions and days spent in hospitals and increases time in the community;
- Reduces the use of acute services;
- Increases engagement in outpatient treatment, care planning and self-care;
- Improves social functioning;
- Increases hope, quality of life, and satisfaction with life;
- Reduces substance use;
- Reduces depression and demoralization;
- Improves chances for long-term recovery;
- Increases rates of family unification; and
- Reduces average services cost per person.
Recognizing the importance of peer services, lawmakers passed HB 1486 (85th, Price/Schwertner) during the 85th Texas Legislature, which required HHSC to create a Medicaid reimbursable state plan benefit for peer support services. To define the new Medicaid benefit and operationalize this directive, HHSC created a Peer Support Stakeholder Workgroup, consisting of providers and people with lived experience from the peer support community. The workgroup provided input on the development and adoption of rules related to peer specialists, peer services, and the provision of those services under Medicaid. The workgroup met frequently between November 2017 through July 2018, and:
- Established training requirements for peer specialists;
- Established certification requirements for peer specialists;
- Defined the scope of services peer specialists may provide;
- Distinguished peer services from other services that a person must hold a license to provide; and
- Developed any other rules necessary to protect the health and safety of persons receiving peer services.
For Peer Support as a Medicaid Benefit, HHSC designated two entities to certify peers, peer supervisors, and peer/peer supervisor training entities: The Texas Certification Board (formerly The Texas Certification Board of Addiction Professionals) and Wales Education Services.
To be eligible to receive Medicaid peer support services, a person must:
- Be at least 21 years old;
- Be a Medicaid recipient;
- Have a mental health condition and/or substance use condition; and
- Have peer specialist services included in the person’s person-centered recovery plan.
To be eligible to become a Medicaid peer specialist provider, a person must:
- Be at least 18 years of age;
- Have lived experience with a mental health condition and/or substance use condition;
- Have a high school diploma or general equivalency degree (GED);
- Appropriately share their own recovery story;
- Demonstrate current self-directed recovery; and
- Pass criminal history and registry checks.
Certified peers must deliver services in conjunction with a facility, provider group, community center, etc., as they cannot yet separately enroll in Medicaid as a Medicaid provider, or be separately credentialed by an MCO. Alternatively, peer specialists without certification are able to provide mental health rehabilitative services and provide peer services through the 1915i and YES Waivers. HHSC provides information on peer support services, the certification process, and benefits of peer supports which can be found at https://hhs.texas.gov/doing-business-hhs/ provider-portals/behavioral-health-services-providers/peer-support-services
More information on peer services in Texas can be found in the Policy Environment Section, and information specific to substance use peer specialists (also called recovery coaches) can be found later in this section.
Clubhouses in Texas
One example of a recovery-oriented program within the Peer Services Programs, Planning, and Policy Unit is Clubhouse. The Clubhouse model is a recovery-oriented program for adults diagnosed with a mental illness. The model has been adopted in Texas and continues to expand to new regions of the state. The purpose of the Clubhouse programming is to improve an individual’s ability to function successfully in the community through involvement in a peer-focused environment. Clubhouse members are encouraged to participate in the everyday operations of the Clubhouse such as clerical duties, reception, food service, transportation, and financial services. Members are also encouraged to participate in activities to promote outside employment, education, meaningful relationships, housing, and an overall improved quality of life. According to a 2018 survey of Clubhouse members, 91 percent of members reported an improvement in their mental health, 70 percent reported having a job or receiving job training/education, and reported a 6 percent jail recidivism rate compared to the general population’s 60 percent.
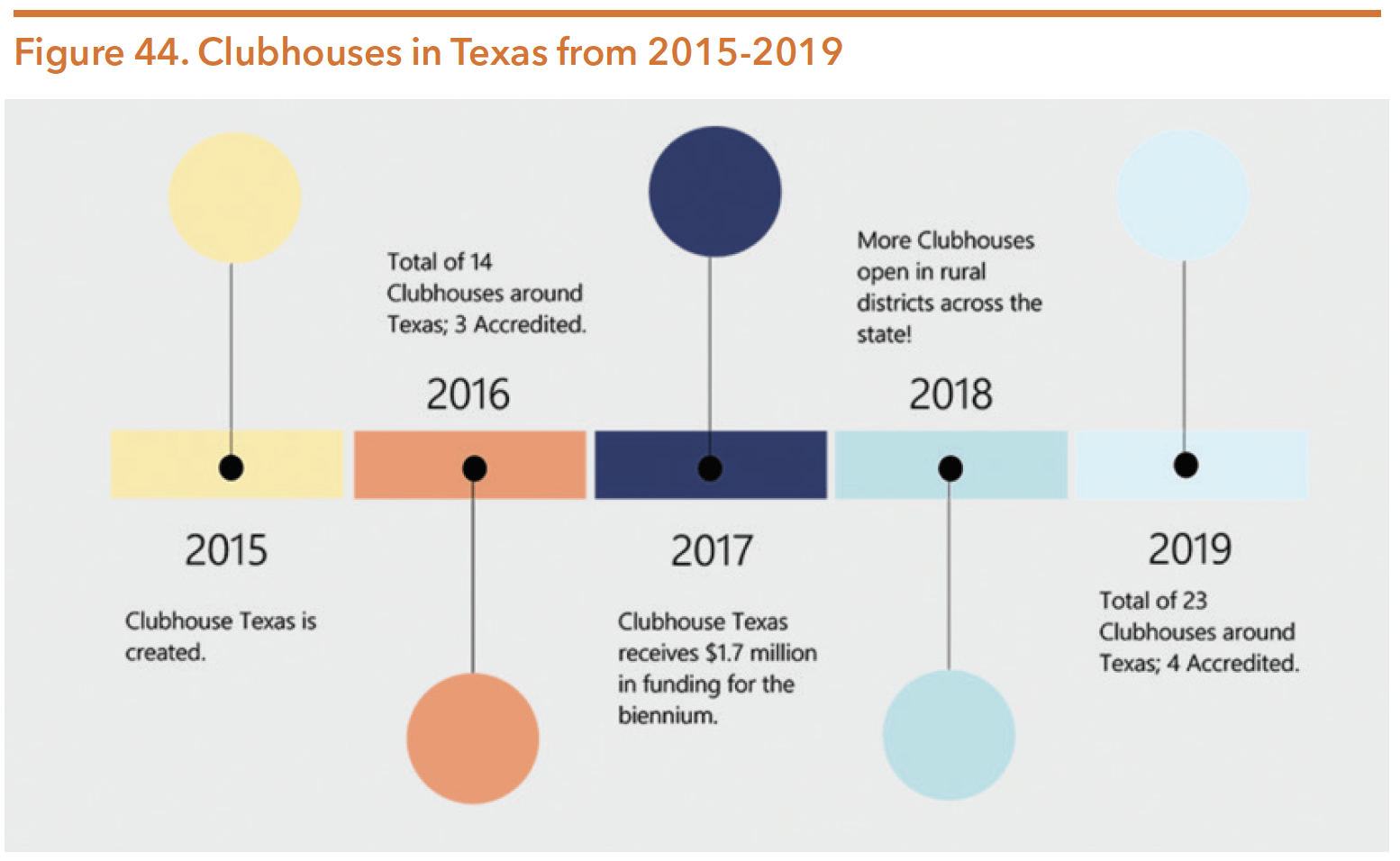
Source: Clubhouse Texas. (n.d.) Clubhouse Texas. Retrieved from http://clubhousetexas.org/#top
WHAT IS A CLUBHOUSE?
Clubhouses provide a caring, supportive community and meaningful work to individuals living with mental illness. Often diagnosed as children or adolescents, people with a chronic mental illness can spend a lifetime in and out of emergency rooms, jails and psychiatric hospitals. Membership and participation with the Clubhouse can help members avoid the crises that often result in hospitalization or incarceration.
Once individuals with mental illness are stabilized, they are often sent home. They are often isolated there, left to manage their illness alone. The Clubhouse surrounds the person with a community of peers, working side-by-side with professional staff. In addition to meaningful work, the Clubhouse has an employment program that helps members find jobs in their community.
Members show up for work every day, doing volunteer tasks and contributing to the maintenance and operations of the Clubhouse. Most participants avoid further hospitalizations as a direct result of attending and working at the Clubhouse.
Source: Clubhouse Texas. (n.d.) Clubhouse Texas. Retrieved from http://clubhousetexas.org/#top
During the 86th legislature, Texas lawmakers recognized the value of Clubhouses and continued their $1.7 million funding through Rider 65. Of the 23 Clubhouses across the state, HHSC contracts with four: Austin Clubhouse, San Angelo Clubhouse, San Antonio Clubhouse, and St. Joseph Clubhouse. Additionally, the Hope Fort Bend Clubhouse is a recipient of a HB 13 Community Mental Health grant.
Certified Community Behavioral Health Clinics (CCBHC) Initiative
In 2014, the federal government passed the Protecting Access to Medicare Act of 2014 (PAMA). Section 223 of PAMA creates a two-year demonstration program for states to certify community behavioral health clinics. According to SAMHSA, CCBHCs are certified community behavioral health clinics that meet federally developed criteria. PAMA directs the care provided by CCBHCs be “patient-centered.” CCBHCs are expected to offer care that is person-centered and family-centered in accordance with the ACA, trauma-informed and recovery-oriented, as well as integrate physical and behavioral health care.
The criteria are based on a review of Medicaid state plans, FQHC standards, Medicaid Health Homes, and other state quality measures. The criteria consist of standards for:
- Staffing;
- Availability and accessibility of services;
- Care coordination;
- Scope of services;
- Quality and other reporting; and
- Organizational authority, governance, and accreditation.
In 2015, Texas was awarded a CCBHC planning grant from SAMHSA. The planning grant allowed HHSC to partner with MCOs, providers, and stakeholders to certify clinics, and develop an integrated service delivery framework.155 The 2015 grant provided one year funds for states to certify community behavioral health clinics, establish a Prospective Payment System (PPS) for Medicaid reimbursable behavioral health services provided by the certified clinics, and prepare an application to participate in a two-year demonstration program.156 The grant was the first of two phases. While Texas was not selected for phase 2 as a national demonstration site, HHSC continues to use the CCBHC framework as a best practice model for the delivery of behavioral health services.
CCBHCs help address gaps in the human services system of care for individuals with serious and persistent mental illnesses, emotional disturbances, and substance use conditions. The goal of expansion across the state is to improve capacity and outcomes for community-based behavioral health services. CCBHCs typically incorporate MOUs with community partners to establish a network of community supports. These partners include primary care providers, local veterans’ services organizations, school districts, individual providers, and others. To ensure a level of consistency across CCBHCs, a list of evidence-based practices (EBPs) was developed as minimum standards. The list of EBPs reflect statewide needs assessment findings and support other Texas program initiatives:
- Adult Specific EBPs:
- SAMHSA Assertive Community Treatment (ACT)
- Cognitive Behavioral Therapy (CBT) and Cognitive Processing Therapy (CPT)
- SAMHSA Illness Management and Recovery (IMR)
- SAMHSA Integrated Treatment for Co-occurring conditions
- SAMHSA Supported Employment and Permanent Supportive Housing
- Child/Adolescent Specific EBPs:
- Nurturing Parent Training
- Trauma Focused CBT
- Case Management using the NWIC Wraparound model, when indicated
- EBPs applicable to all populations:
- Screening, Brief Intervention, and Referral to Treatment (SBIRT) model
- Motivational Interviewing
- Person-Centered Recovery Planning
- Seeking Safety
In order to become certified as a CCBHC, a community clinic must go through an extensive application process. Once approved, certification is valid for 3 years. In FY 19, Texas had 12 CCBHCs with plans to increase to 19 during FY 20, as indicated in their inaugural business plan, Blueprint for a Healthy Texas. More information on HHSC’s plan can be found in the Policy Environment Section of this Guide.
CRISIS SERVICES
The Texas Administrative Code defines a psychiatric crisis as a situation in which an individual presents the following risk factors due to a mental health condition:
- Presents an immediate danger to self or others;
- Is at risk of serious deterioration of mental or physical health; and/or
- Believes that he or she presents an immediate danger to self or others, or that his or her mental or physical health is at risk of serious deterioration.
During the 86th legislative session, lawmakers increased community mental health crisis funding to a total of $343,263,746 in the 2020-2021 biennium, an increase of $17,833,194 from the 2018-2019 biennium. Crisis services funding is used to enhance community-based psychiatric emergency services projects that serve as alternatives to divert individuals from hospitals, emergency rooms, and/or jails.
In 2020, HHSC created a COVID-19 hotline specifically to assist Texans dealing with mental health needs related to the pandemic. The hotline is staffed by mental health professionals employed at the Harris County MHMR and helps to refer callers to needed services based on their individual situation.
Crisis services are available statewide to individuals regardless of if they are enrolled in ongoing mental health care. Table 33 lists most of the crisis services available through state-funded programs and providers:
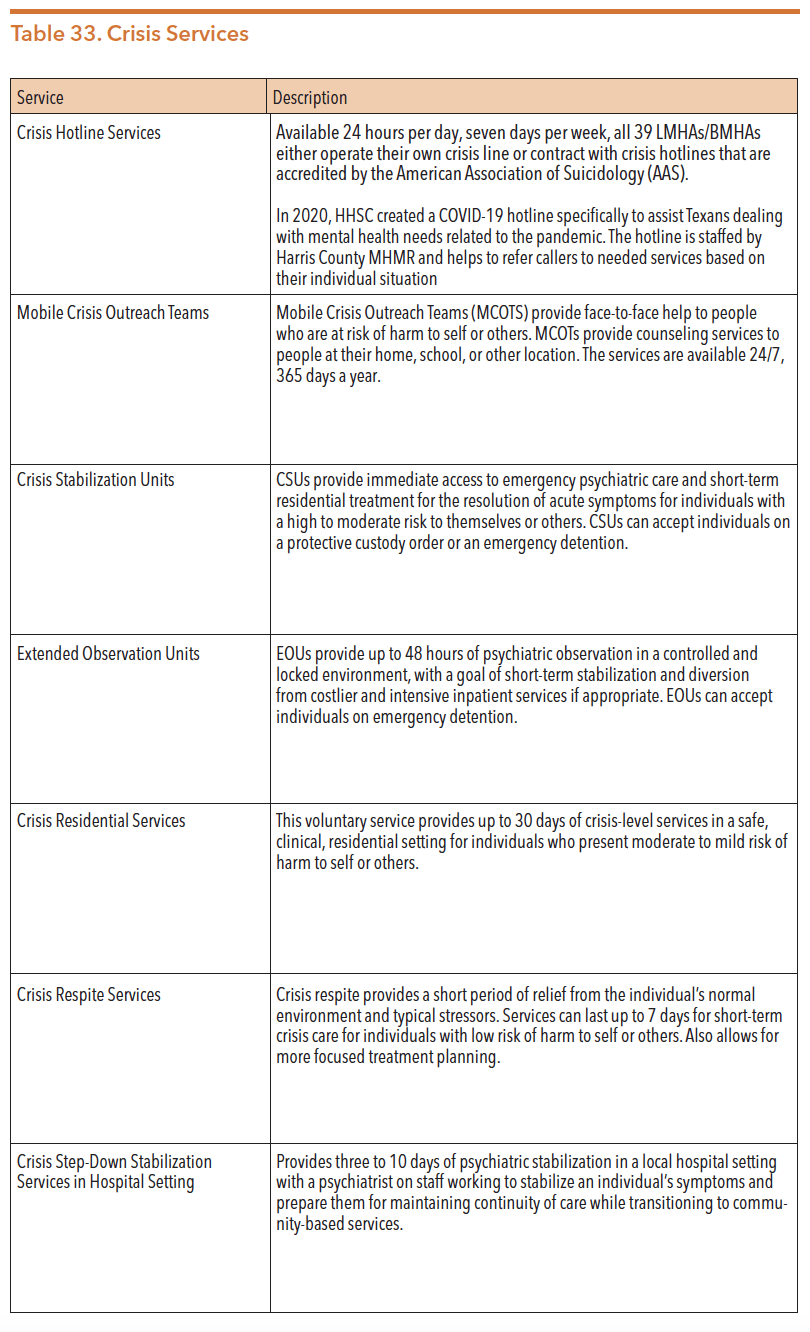

Source: Texas Department of State Health Services. (2010). Crisis services. Word document retrieved from https://www.dshs.texas.gov/mhsacsr/Mental-Health-and-Substance-Abuse-Crisis-Services-Redesign.pdf
Texas Health and Human Services Commission. (2020). Crisis units. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/mental-health-crisis-services/crisis-units
and Texas Department of State Health Services. (2016). Presentation to Select Committee on Mental Health: The behavioral health system [PowerPoint slides]. Retrieved from http://www.legis.state.tx.us/tlodocs/84R/handouts/ C3822016021810001/5fc9614b-41a4-436e-9eba-67b14f00ad22.PDF
Utilization and Costs
The utilization and cost for residential and outpatient crisis mental health services are included in Table 34 and Table 35 below.
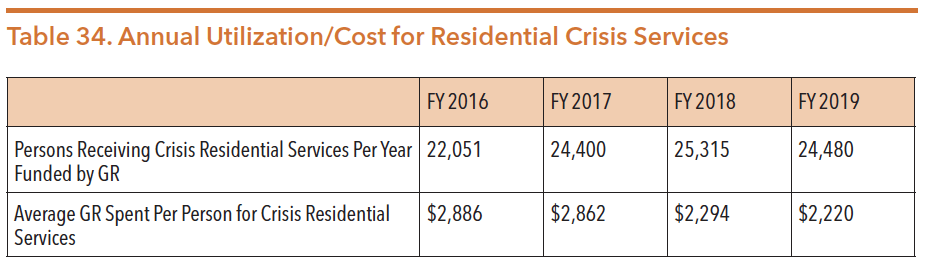
Source: Texas Health and Human Services Commission. (2020). IDD-BHS data book. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/idd-bhs-data-book.pdf
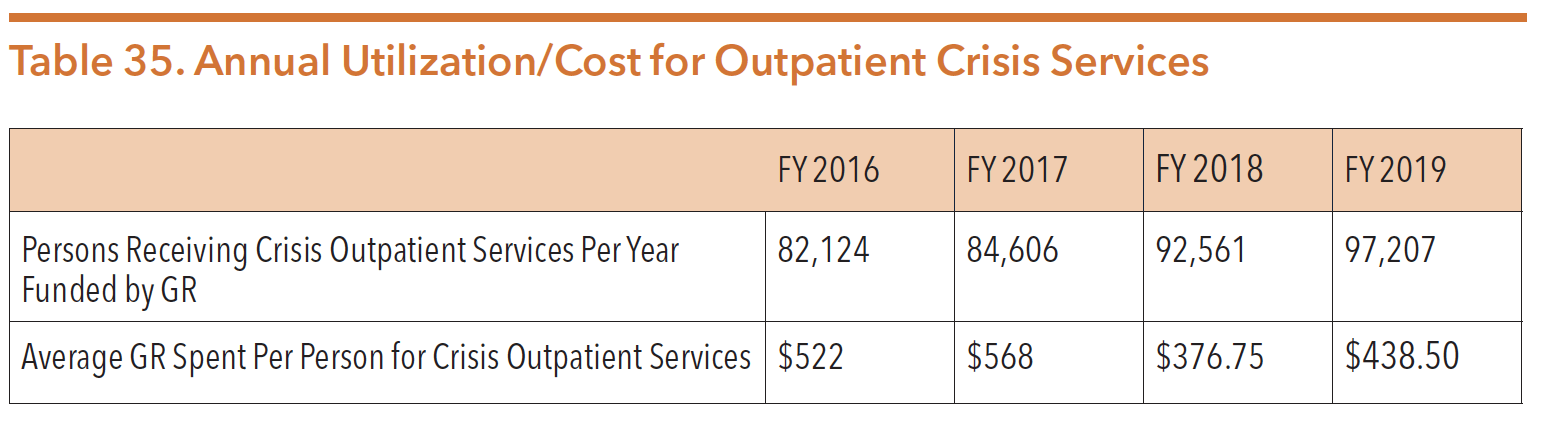
Source: Texas Health and Human Services Commission. (2020). IDD-BHS data book. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/idd-bhs-data-book.pdf
INDIVIDUALS CONSIDERED MEDICALLY INDIGENT
According to the Texas Health and Safety Code, a person is defined as medically indigent if they are under the following circumstances:
- Possesses no property
- Has no person legally responsible for their support
- Is unable to reimburse the state for the costs of support, maintenance, and treatment.
Individuals who are deemed to be medically indigent are eligible to receive services through the public mental health system without the state receiving compensation or reimbursement for service, and cannot be denied services on their ability to pay. Within the first 30 days of rendering mental health services, LMHA/LBHA staff (typically benefits coordinators or office managers) conduct a financial assessment of an individual’s ability to pay for services and calculate a maximum monthly fee (or no fee) depending on the individual’s gross income, family size, and extraordinary expenses paid in the last 12 months or expected in the next 12 months.
The County Indigent Health Care Program (CIHCP) was created by the Texas Legislature in 1985 and provides health care services to individuals who do not qualify for other state or federal health care programs. CIHCP provides health services through counties, hospital districts, and public hospitals to eligible residents who:
- Live in Texas;
- Have income at or below 21 percent of FPL;
- Have resources less than $2,000; and
- Are not eligible for Medicaid.
For more information on CIHCP, please see https://hhs.texas.gov/services/health/ county-indigent-health-care-program.
MENTAL HEALTH NEEDS OF AGING TEXANS
Texas is home to a large number of aging individuals. According to the Texas Demographic Center, in 2018 there were over 3.6 million people in Texas age 65 or older (12.6 percent of the total population).165 Between 2010 and 2018, the 65 plus age category had the greatest increase (slightly more than one million) and grew at the fastest rate compared to the younger age groups.166 By 2050, this population is expected to more than double, growing to more than 8 million.
Aging Texans require mental health and substance use services to meet their unique needs. People who are aging often have under-recognized and undertreated behavioral health conditions. Approximately 20 percent of the older population has some form of neurological or mental health condition, the most common including dementia, depression, anxiety, and substance use. An estimated 1.4 to 4.8 percent of the over 49 million adults over the age of 65 in the United States have serious mental illness. It’s also estimated that two-thirds of these older adults with mental health conditions do not receive the services and support they needs due to a lack of services focused on this age group. The suicide rate among Texans 65 and older reached almost 25 a day in 2018 in the United States, with people over 85 years old with the highest suicide rate of any age group.
It is important to know that depression is not a normal part of aging. However, depression often co-occurs with other serious illnesses, such as heart disease, stroke, diabetes, cancer, and Parkinson’s disease. Many health professionals mistakenly conclude that depression is a consequence of these problems, leaving the condition widely unrecognized and undertreated among older adults.
SUBSTANCE USE
The national opioid crisis has brought the dire need for an array of substance use supports and services to the forefront of behavioral health conversations. According to SAMHSA, in 2018 an estimated 20.3 million Americans aged 12 and older self-reported needing support for substance use in the past year. SAMHSA also estimates that the impact of individuals not having ready access to supports and services cost the nation more than $600 billion each year.
Prior to 2010, Medicaid reimbursement for substance use services in Texas was only available to individuals under the age of 21, and those benefits were limited in scope. In 2009, the 81st Texas Legislature directed HHSC to develop Medicaid state plan substance use condition benefits for adults. Implementation of these services began in 2010. Subsequently in 2015, the legislature directed HHSC to develop a methodology for evaluating the cost benefits of these services. The 85th Texas Legislature then directed HHSC to submit a report on the findings of the evaluation by December 1, 2017.
The December 2017 report showed that the average monthly Medicaid costs for individuals with a SUD diagnosis receiving SUD services ($1,410) was lower than the average monthly cost for individuals with a SUD diagnosis ($1,559) who did not receive treatment. The data also showed that people who received SUD services had a decrease in homelessness and arrests, two outcomes which often generate costs in other systems. This report is available online at https://hhs.texas.gov/sites/ default/files/documents/laws-regulations/reports-presentations/2017/substance-abuse-disorder-treatment-nov-2017.pdf.
OUTREACH, SCREENING, ASSESSMENT, AND REFERRAL (OSAR)
OSAR providers are often the first point of contact and serve as the front door for those seeking substance use condition treatment service. As a result of SB 1507 (84th, Garcia/Naishtat), OSAR providers are responsible for substance use outreach, screenings, assessments, and referrals for substance use services free of charge and are now co-located within LMHAs/LBHAs across all of Texas. While LMHAs are the only entities that can now act as OSAR providers, they are authorized to subcontract with substance use providers to provide OSAR services.
As of March 2020, there were 14 main OSAR offices, with at least one operating in each of the 11 Texas Health and Human Services regions. Figure 45 displays the location of the OSARs across the state. OSARs serve approximately 30,000 individuals annually funded by approximately $7 million per year. OSARs are able to serve adults and adolescents. While many LMHAs attempted to address OSAR accessibility through satellite offices, there were some administrative and logistical challenges. For example, assessments and screenings often require appointments, offices are open for limited hours and days of the week, and services are available based on counselor availability.
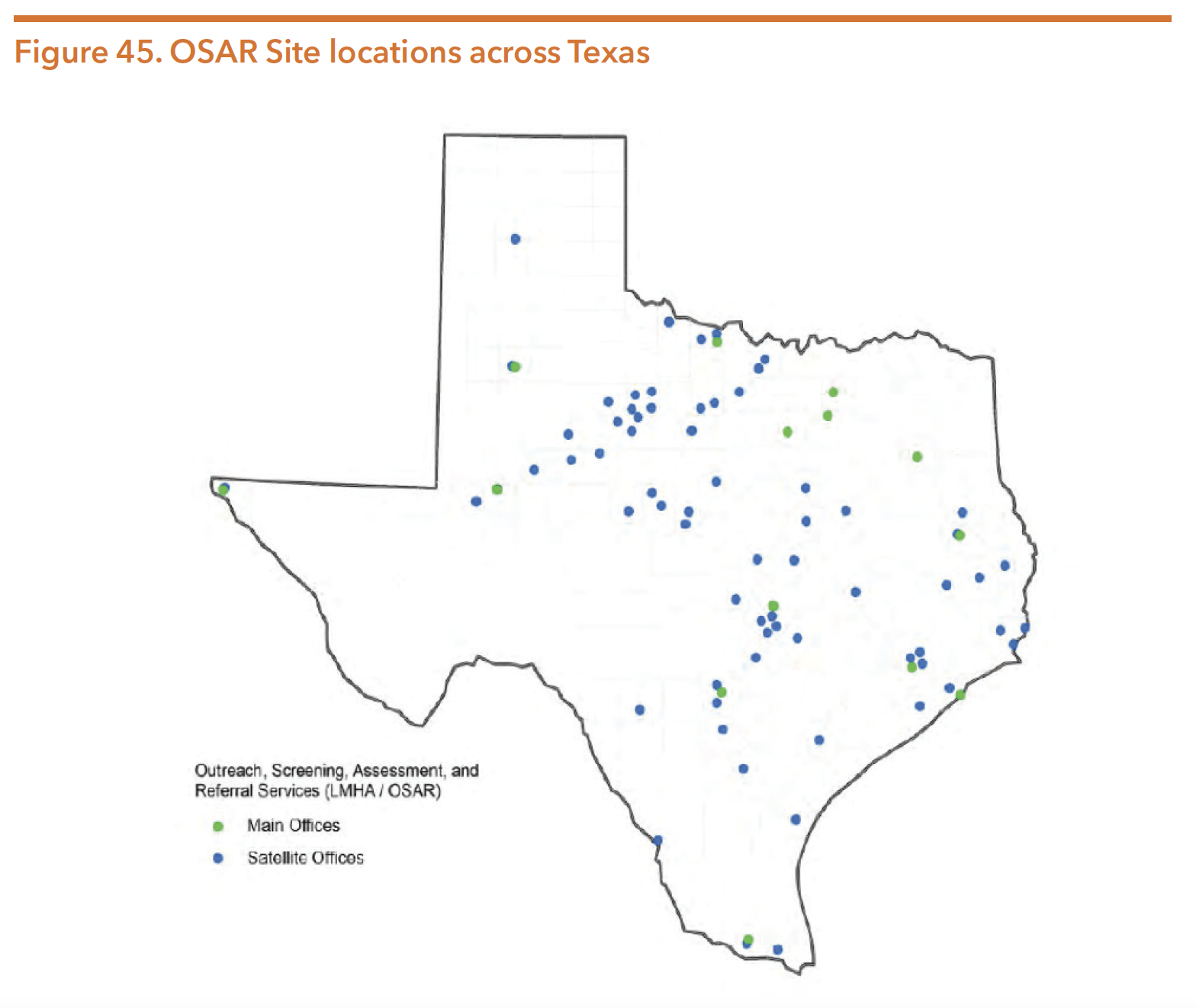
Source: Gaines, S. & Ramirez, L. (2018). Presentation to the Senate Health and Human Services Committee on substance use disorder in Texas. Texas Health and Human Services Commission. Retrieved from https://hhs.texas.gov/reports/2018/03/presentation-senate-health-human-services-committee-substance-use-disorder-texas
SUBSTANCE USE SERVICES
The HHS System provides substance use services for eligible youth and adults through contracts with service providers. These treatment services differ from OSAR services as they cover a continuum of care after receiving a screening, assessment, or referral and are not required to contract with the LMHAs. The HHSC Mental Health and Substance Use Division is responsible for creating and implementing policies regarding substance use services and defining optimal treatment outcomes. Table 36 highlights HHSC’s non-Medicaid indigent substance use care programs across a continuum of care. The varying treatment levels of care for adults and youth are outlined in Table 37.

Source: Gaines, S. & Ramirez, L. (2018). Presentation to the Senate Health and Human Services Committee on Substance Use Disorder in Texas. Texas Health and Human Services Commission. Retrieved from https://hhs.texas.gov/reports/2018/03/presentation-senate-health-human-services-committee-substance-use-disorder-texas
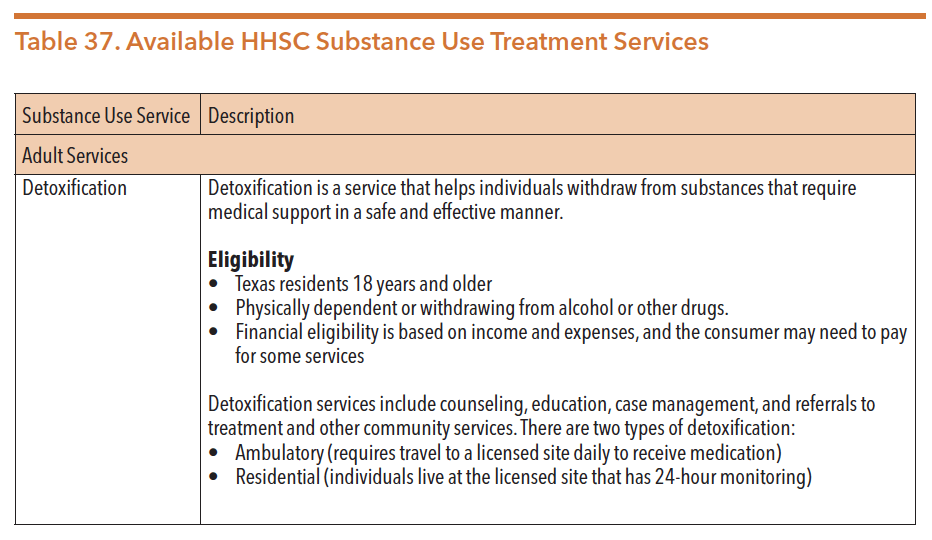

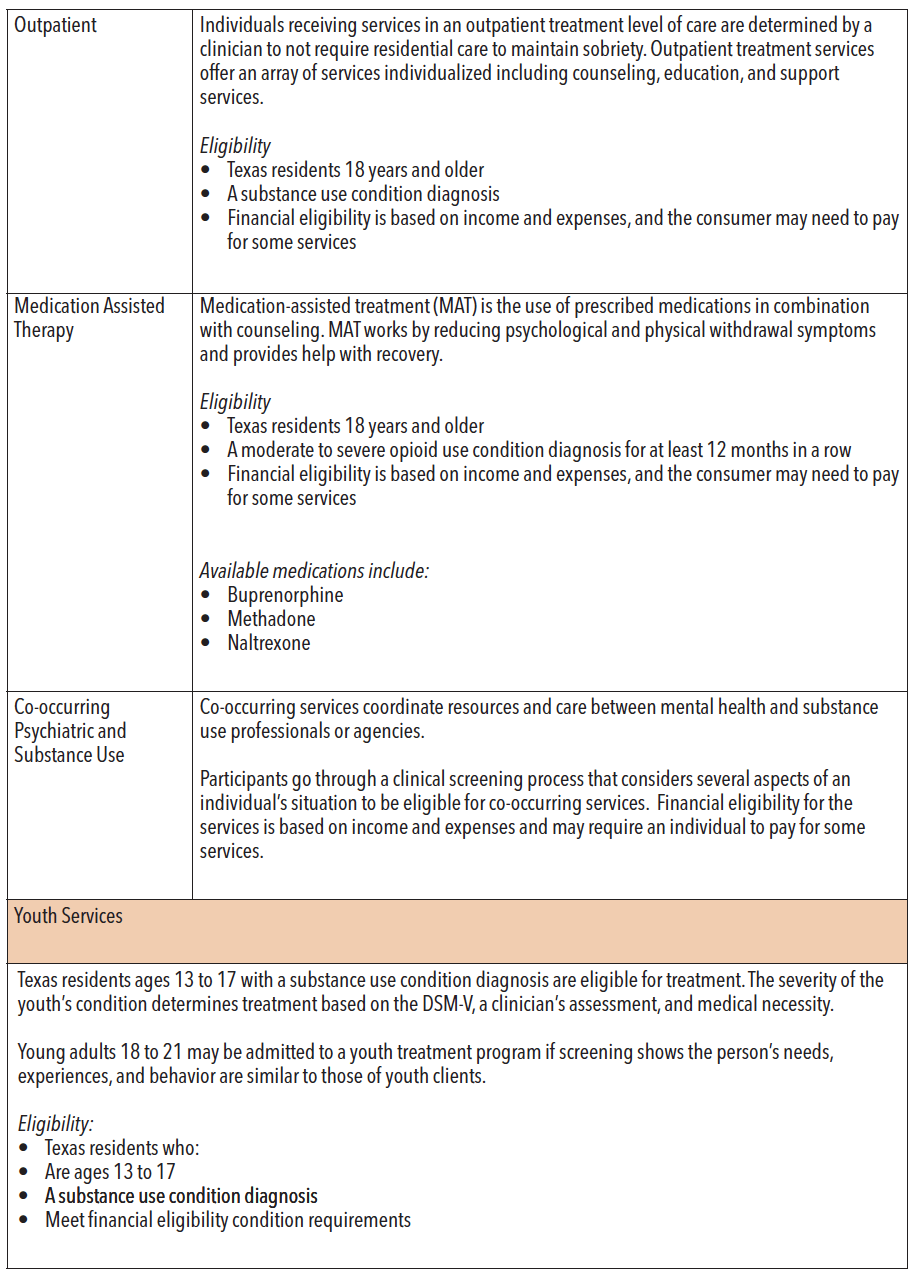
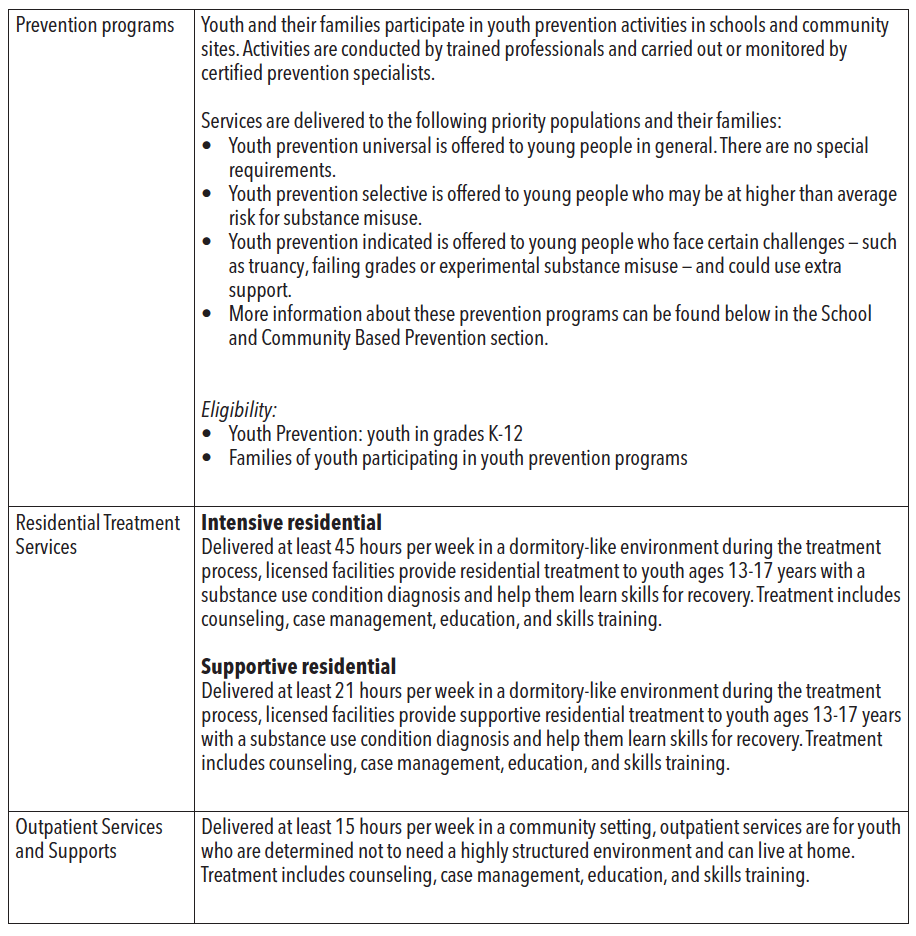
Sources: Gaines, S. & Ramirez, L. (2018). Presentation to the Senate Health and Human Services Committee on Substance Use Disorder in Texas. Texas Health and Human Services Commission. Retrieved from https://hhs.texas.gov/reports/2018/03/presentation-senate-health-human-services-committee-substance-use-disorder-texas
Texas Health and Human Services Commission. (n.d.). Adult substance use detoxification services. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/adult-substance-use/adult-substance-use-detoxification-services
Texas Health and Human Services Commission. (n.d.). Adult substance use intensive residential treatment. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/adult-substance-use/adult-substance-use-intensive-residential-treatment
Texas Health and Human Services Commission. (n.d.). Adult substance use HIV services. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/adult-substance-use/hiv-services
Texas Health and Human Services Commission. (n.d.). Adult substance use women & children in residential treatment. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/adult-substance-use/adult-substance-use-women-children-residential-treatment
Texas Health and Human Services Commission. (n.d.). Adult substance use outpatient program. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/adult-substance-use/adult-substance-use-outpatient-program
Texas Health and Human Services Commission. (n.d.). Adult substance use medication-assisted treatment. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/adult-substance-use/adult-substance-use-medication-assisted-treatment
Texas Health and Human Services Commission. (n.d.). Co-occurring psychiatric & substance use disorder. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/adult-substance-use/co-occurring-psychiatric-substance-use-disorder
Texas Health and Human Services Commission. (n.d.). Youth substance use. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/youth-substance-use
Texas Health and Human Services Commission. (n.d.). Youth substance use prevention programs. Retrieved from https://hhs.texas.gov/services/mental-health-substance-use/youth-substance-use/youth-substance-use-prevention-programs
Co-occurring Mental Health and Substance Use Conditions
Many individuals experience mental health and substance use concerns simultaneously. According to SAMHSA, in 2018 across the United States:
- 47.6 million adults received a mental health diagnosis;
- 5.9 million adolescents received a mental health diagnosis;
- 20.3 million adults received a substance use diagnosis;
- 916,000 adolescents received a substance use diagnosis;
- 12.4 million adults received both a mental health and substance use diagnosis; and 358,000 youth a mental health and substance use diagnosis
Individuals living with mental health conditions are more likely than those without to have a co-occurring substance use condition. Often someone with a mental health condition who is not engaged in any supports or treatment may “self-medicate” with alcohol or drugs, which can lead to misuse and ultimately a substance use condition. Integrating physical and behavioral health care is the best way to ensure that any co-occurring conditions are addressed. Additionally, early detection, intervention, and treatment offer the best potential for positive outcomes and recovery.
State agencies and organizations are increasingly using the term “behavioral health” in place of “mental health” to more accurately represent the co-occurrence of mental health and substance use conditions. In an effort to improve integrated care, there has also been increased focus on how LMHAs can better integrate substance use services with the mental health services typically provided by LMHAs/LBHAs. The Texas program aimed at addressing co-occurring mental health and substance use conditions is the Co-Occurring Psychiatric and Substance Use Disorders Services, or COPSD. These programs emphasize the need to address both conditions as simultaneous, primary conditions. As of September 2020, HHSC was reviewing substance use treatment standards of care rules in the Texas Administration Code Title 25, Chapter 448 to address barriers in licensing that prevent facilities’ ability to provide integrated COPSD Treatment.
SUBSTANCE USE FUNDING
The level of public funding for substance use services is not sufficient to address need, creating significant barriers to treatment. In Texas, substance use treatment is funded through a variety of sources, including health insurance, self-pay, federal grants including the Substance Abuse Prevention and Treatment (SAPT) Block Grant, state general revenue, Medicaid (if applicable), and federal funds through 1115 waiver projects. A large amount of federal funds awarded to states are to be used to address opioid use known at State Opioid Response (SOR) and State Targeted Response (STR) grants. In Texas, these dollars are collectively awarded through the Texas Targeted Opioid Response (TTOR). For a more in-depth overview of substance use funding, please refer to the Funding section of this guide.
Per HHSC, federal funds account for 73 percent of total HHSC funding for substance use prevention, intervention, treatment, and recovery in Texas– while 27 percent comes from state general revenue. Table 38 shows All Funds funding trends allocated to substance use over the last three budget cycles.
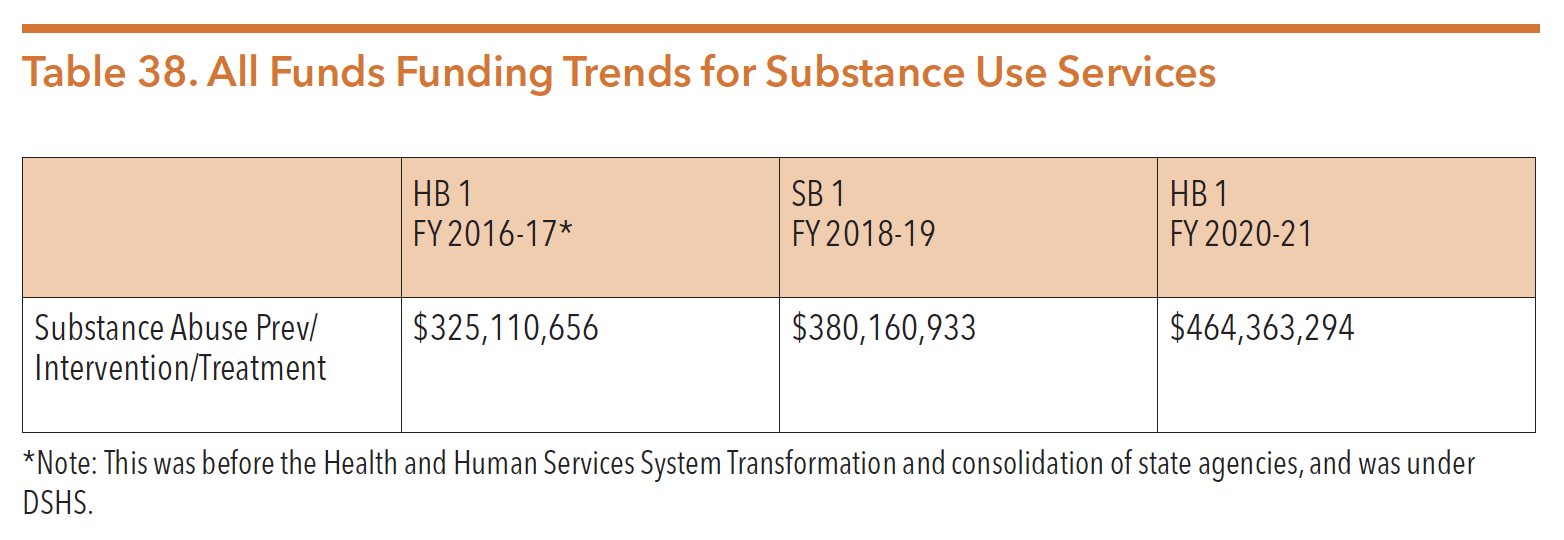
Sources: Texas Legislature Online (2019). H.B.1, General Appropriations Act, 86th Legislature, FY 2020-21. Retrieved from https://capitol.texas.gov/tlodocs/86R/billtext/pdf/HB00001F.pdf#navpanes=0
Texas Legislature Online (2017). S.B.1, General Appropriations Act, 85th Legislature, FY 2018-19. Retrieved from https://capitol.texas.gov/tlodocs/85R/billtext/pdf/SB00001F.pdf#navpanes=0
Texas Legislature Online (2015). H.B.1, General Appropriations Act, 84th Legislature, FY 2016-17. Retrieved from https://capitol.texas.gov/tlodocs/84R/billtext/pdf/HB00001F.pdf#navpanes=0
Block Grant Priority Populations
Federally, SAMHSA identifies populations that receive priority for admission for substance use services before anyone else, in the following order of priority:
- Pregnant women who use substances intravenously (must be admitted immediately)
- Other pregnant women (must be admitted immediately)
- Individuals using substances intravenously (must be admitted within 14 days)Additionally, Texas has identified two additional priority populations (must be admitted within 72 hours):
- Individuals identified as high risk of overdose
- Individuals referred by Department of Family and Protective Services (DFPS)
UTILIZATION AND COSTS
The following two figures show the yearly utilization and costs of substance use services; Table 39 details information for adults and Table 40 is for youth.
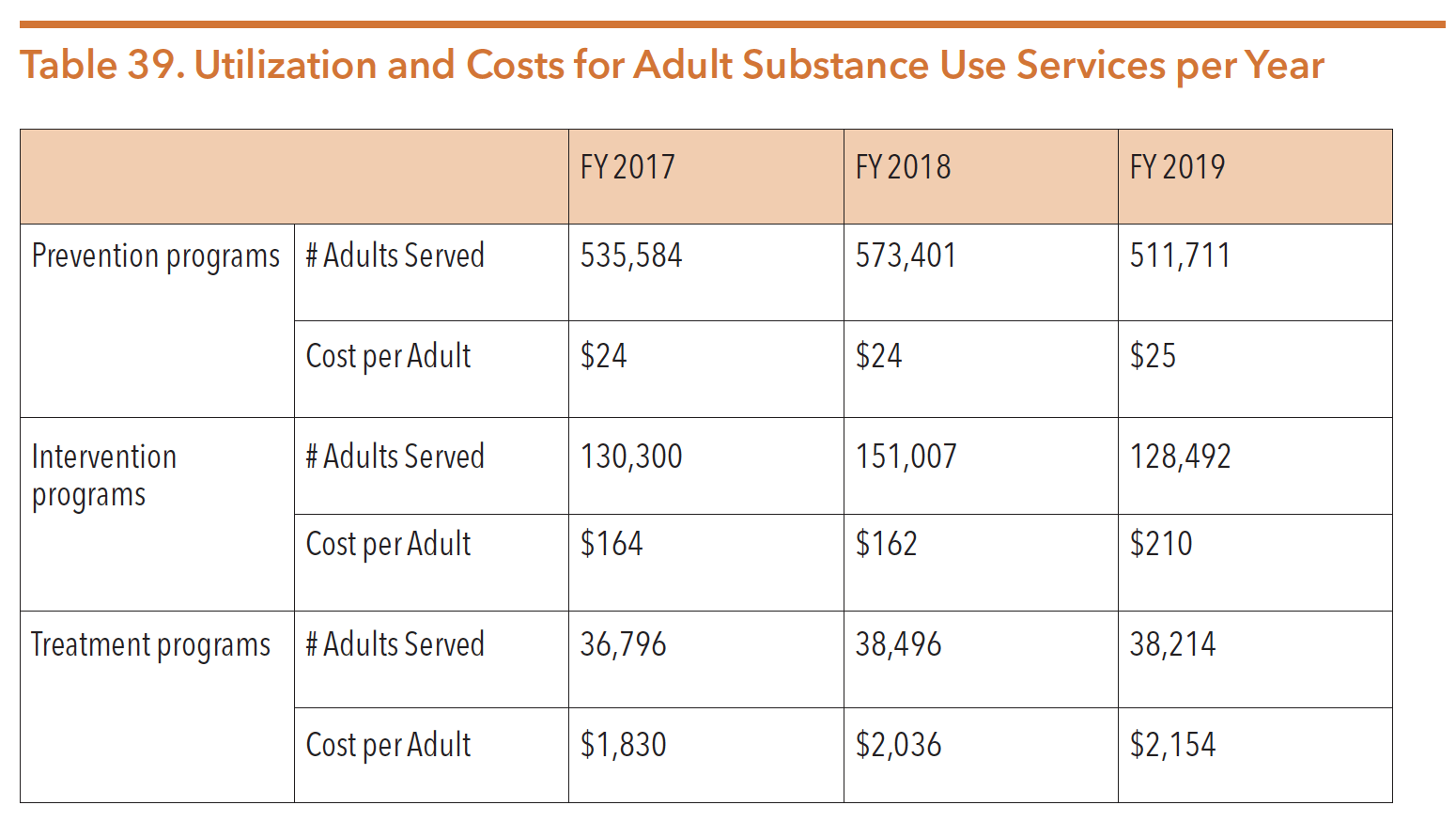
Source: Texas Health and Human Services Commission. (2020). IDD-BHS data book. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/idd-bhs-data-book.pdf
Figure 46 and Figure 47 further details treatment program admissions for adults; Figure 48 and Figure 49 details this information for youth.
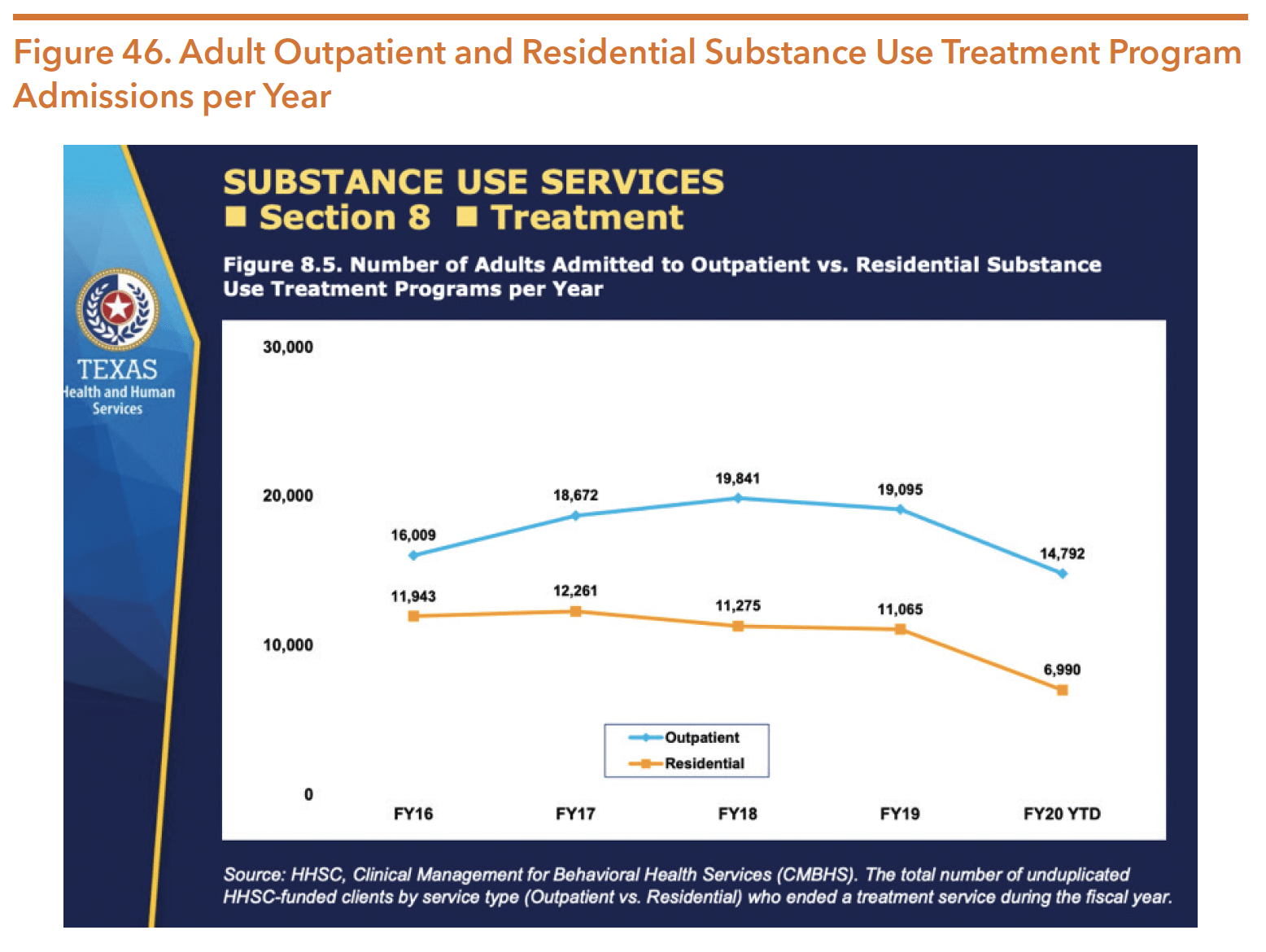
Source: Texas Health and Source: Texas Health and Human Services Commission. (2020). IDD-BHS data book. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/idd-bhs-data-book.pdf
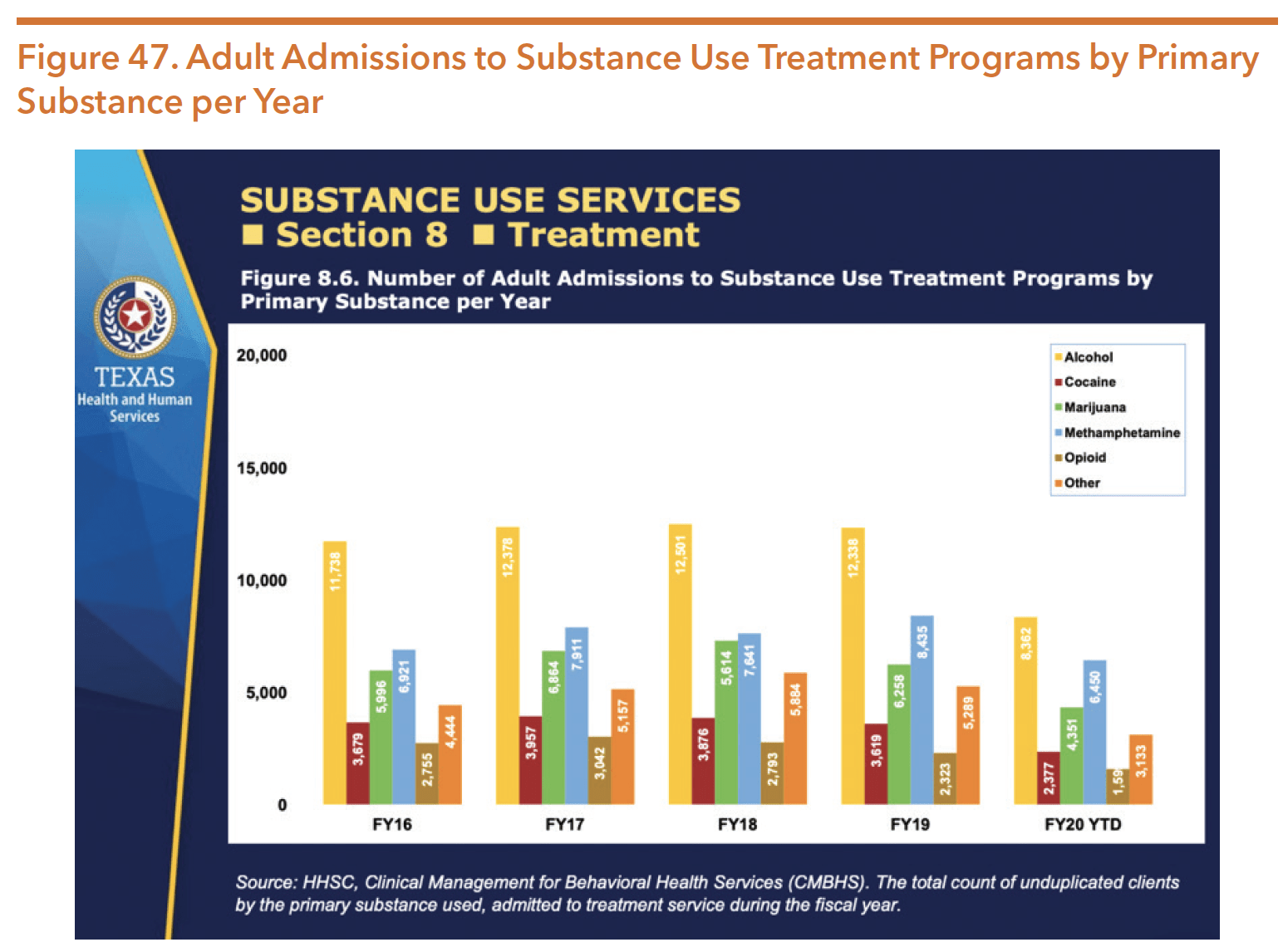
Source: Texas Health and Human Services Commission. (2020). IDD-BHS data book. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/ idd-bhs-data-book.pdf
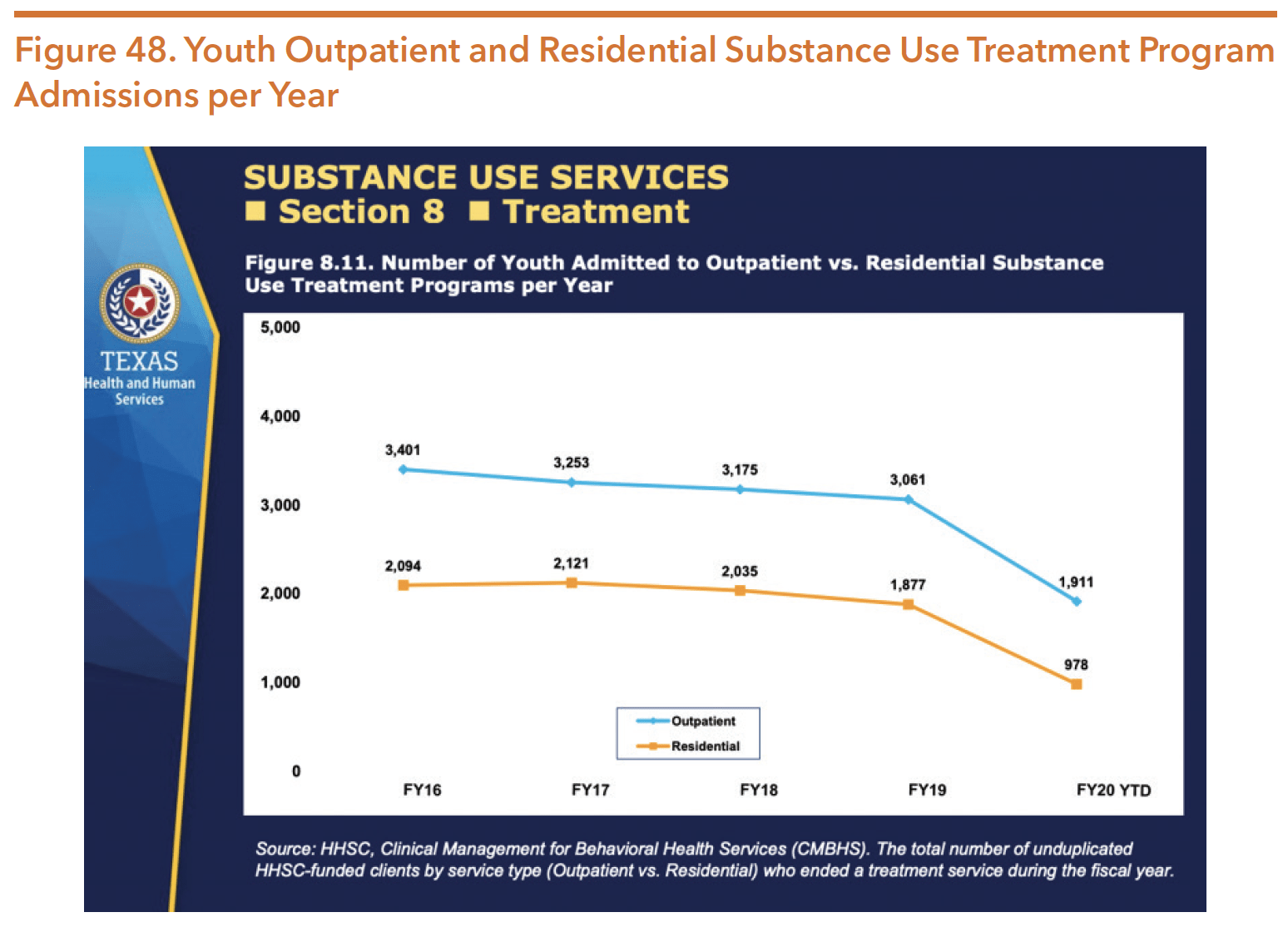
Source: Texas Health and Human Services Commission. (2020). IDD-BHS data book. Retrieved from https://hhs.texas.gov/ sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/idd-bhs-data-book.pdf
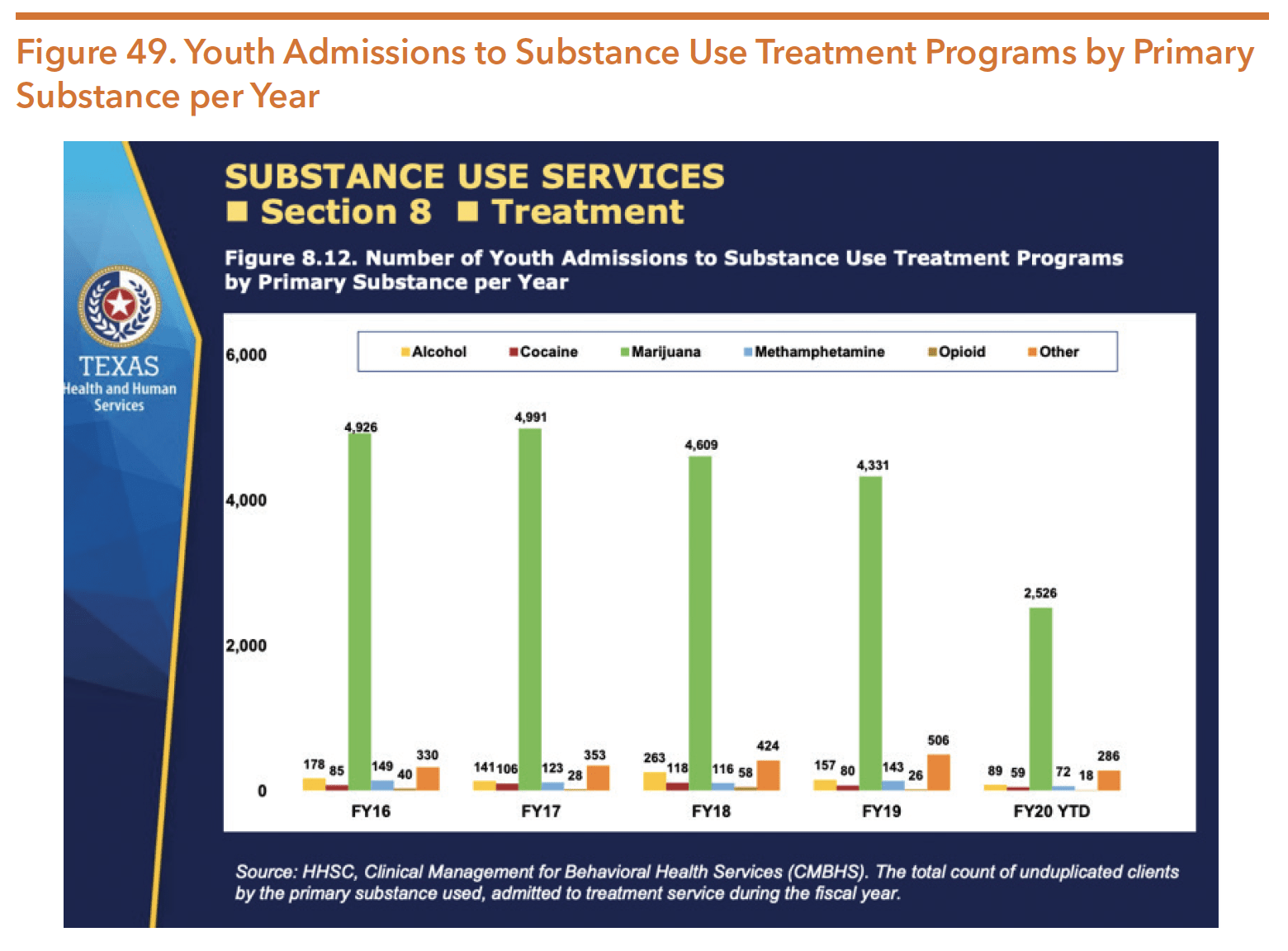
Source: Texas Health and Human Services Commission. (2020). IDD-BHS data book. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/idd-bhs-data-book.pdf
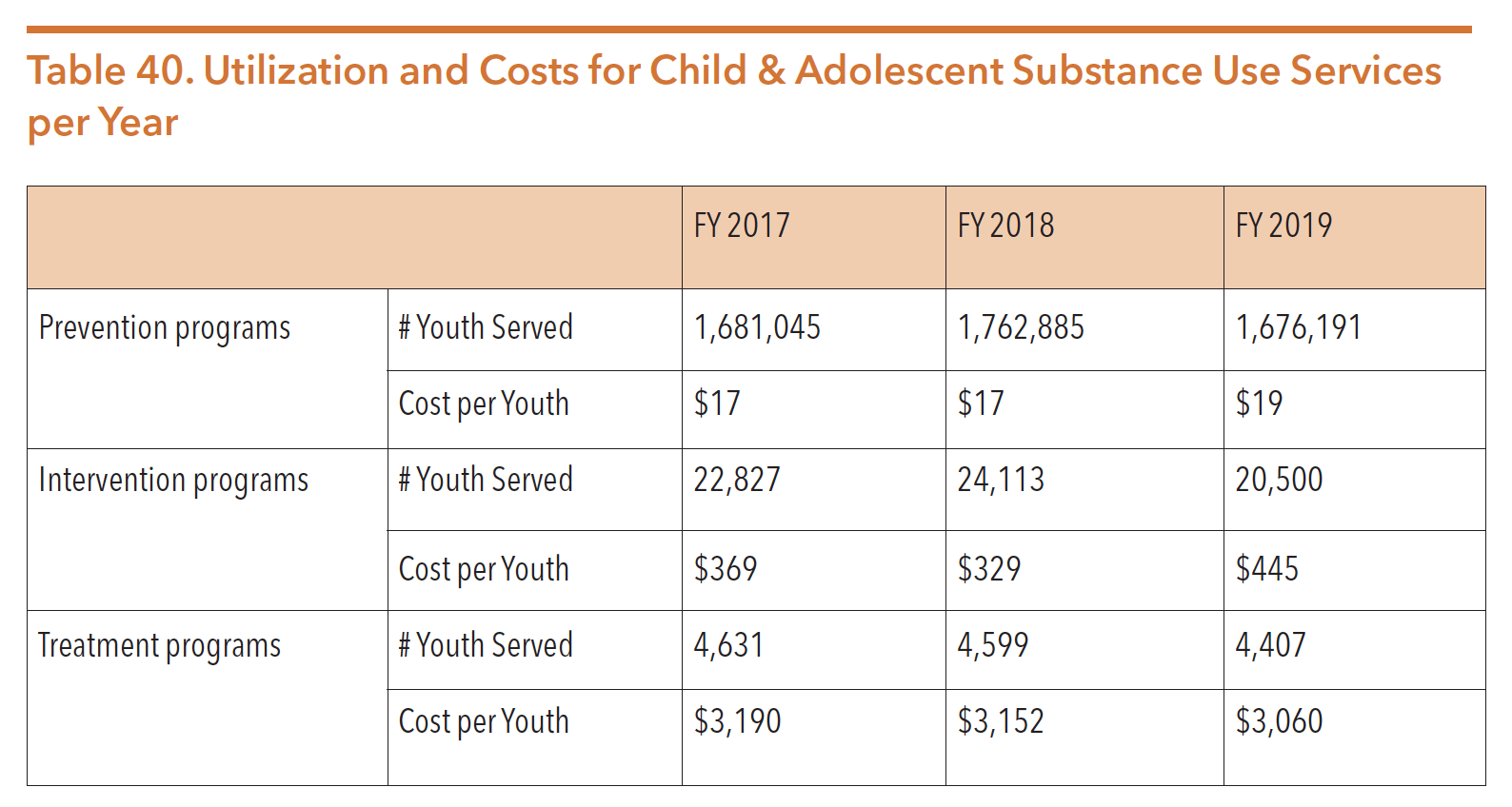
Source: Texas Health and Human Services Commission. (2020). IDD-BHS data book. Retrieved from https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/behavioral-health-provider/idd-bhs-data-book.pdf
QUALITY OF CARE MEASURES
HHSC monitors quality and performance in several areas based on the Texas Resilience and Recovery framework. More information on the TRR Framework is available under the Community Mental Health Services section. Table 41 shows some of the measures tracked on a regular basis for adult substance use services and Table 42 shows the same for youth services.
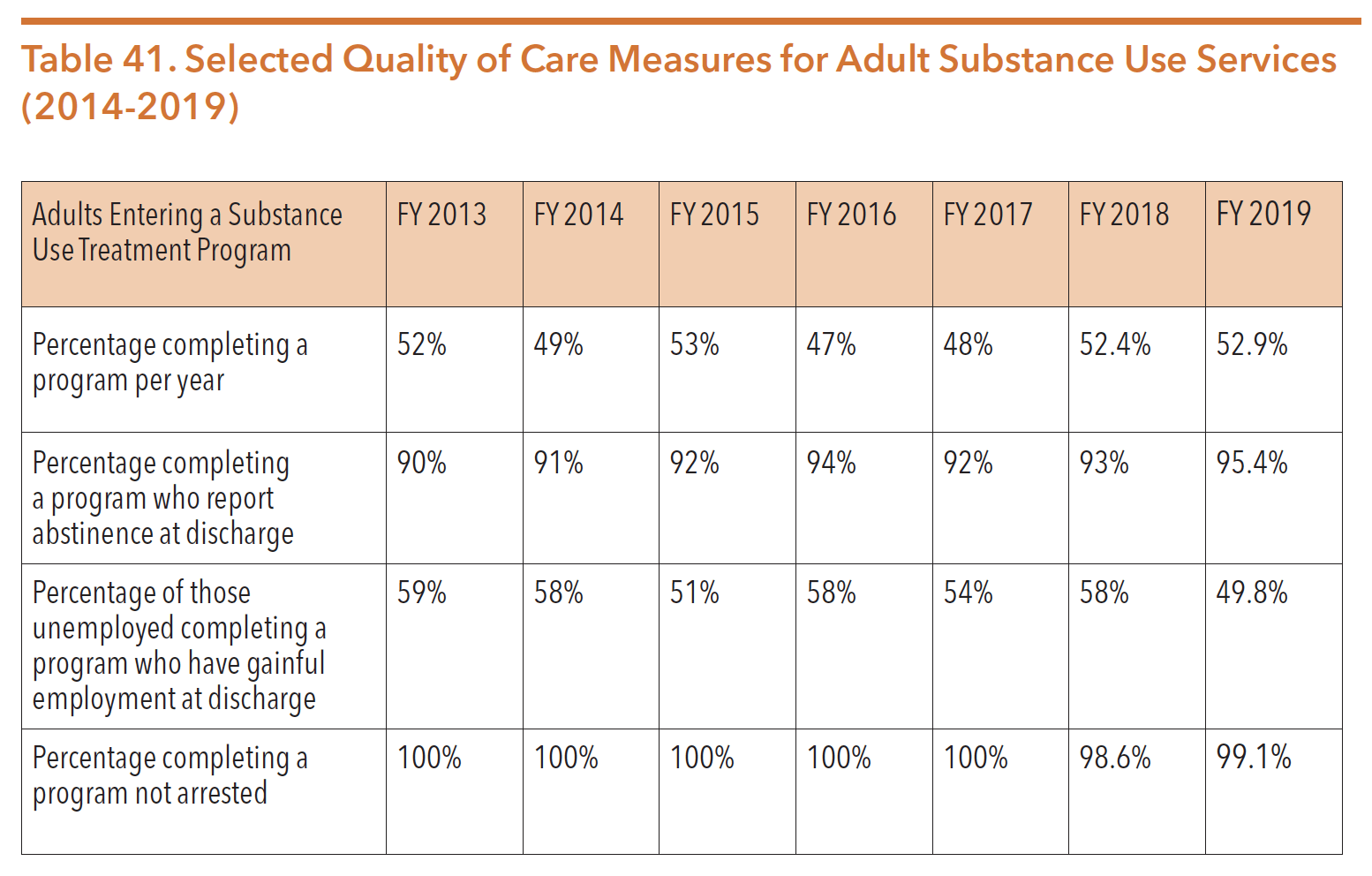
Sources: Texas Health and Human Services Commission. Data request. Received 8/15/18.
Texas Health and Human Services Commission. FY 18-19 Data Request. Data request May 20,2020. Data received from Sonja Gaines.
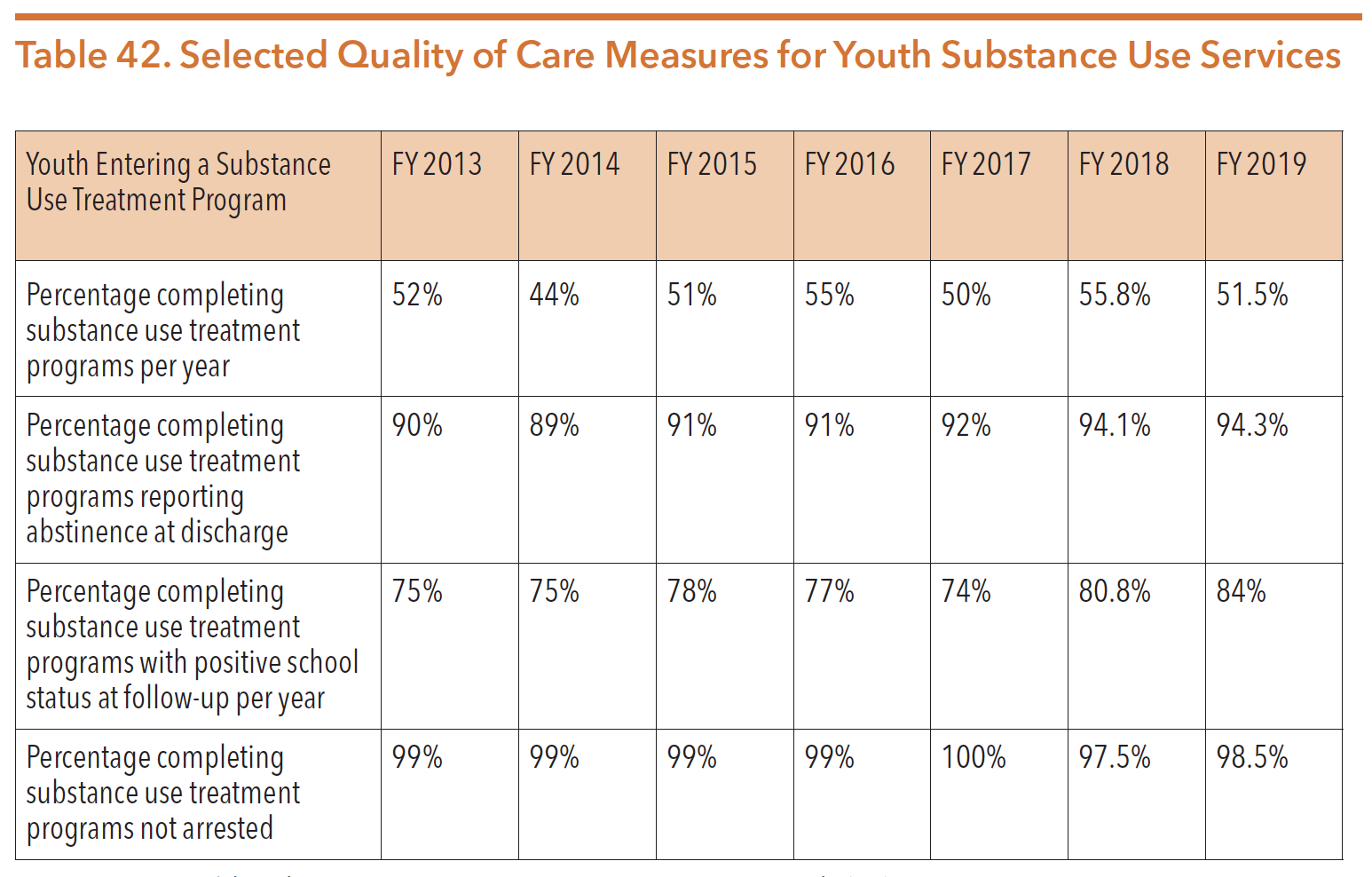
Sources: Texas Health and Human Services Commission. Data request. Received 8/15/18.
Texas Health and Human Services Commission. FY 18-19 Data Request. Data request May 20,2020. Data received from Sonja Gaines.
RECOVERY HOUSING
Recovery housing is one evidence-based resource that empowers individuals to achieve and maintain a life in recovery from substance use conditions. Recovery housing is a shared living environment that promotes sustained recovery from substance use. Recovery houses allow for integration into the surrounding community and provides a setting that: connects residents to supports and services, is centered on peer support, and is free from substance use. Individuals living in recovery housing have a greater chance of achieving long-term recovery than those who do not live in recovery-oriented environments. Living in recovery housing has been associated with positive outcomes including decreased substance use, reduced probability of relapse/reoccurrence, and lower rates of incarceration.
Because federal disability policy within the Social Security Code does not classify substance use condition as a disability, people with substance use condition are ineligible for many benefits available to people with serious mental illness or other disabilities, including: income, employment, and housing benefits. Further, individuals in recovery from substance use conditions cannot access Medicaid coverage through the Aged, Blind, and Disabled category, the Project Access Program, disability income, vocational rehabilitation services, or Section 8 rental assistance. The federal definition of disability per Section 223 of the Social Security Code, specifically excludes substance use, stating “an individual shall not be considered to be disabled for purposes of this title if alcoholism or drug addiction would be a contributing factor material to the Commissioner’s determination that the individual is disabled.”
Identified through Gap #12 in the Texas Statewide Behavioral Health Strategic Plan, access to housing is a critical issue across the state, but more so for those with substance use conditions in our public behavioral health system.
Distinguished by the National Association of Recovery Residences (NARR), there are four widely accepted and defined levels of recovery housing:
- Level I – Run democratically, peer-ran, and self-sufficient with typical open length of stay
- Level II – Level I with a house manager or senior resident who is responsible for oversight
- Level III – Structured or semi-structured with paid staff, like certified staff or case managers
- Level IV – Inclusive of clinical services or residential treatment centers with credentialed staff
A resource for more information on specific standards of each level can be found at https://narronline.org/wp-content/uploads/2014/02/NARR-Standards-20110920.pdf
Oxford House, Inc.
The Oxford House program is a democratically operated, peer-run recovery model intended to be self-supporting after an initial start-up investment. Residents are expected to contribute to rent and expenses during their stay in order to be self-sustaining. HHSC reports that 62 percent of Oxford House residents have previously experienced homelessness. As of July 2020, there were 288 Oxford Houses in Texas operating at approximately 81 percent capacity across 22 counties, with 407 of the 2,159 beds vacant. Of the 288 houses, 174 were specified homes for men, 8 allowed children, and 103 for women, with 37 of those homes allowing children.
In 2020, Oxford House, Inc. was the sole-entity receiving any state funding for recovery housing in Texas. Oxford House, Inc. administers start-up loans from the state funds to individuals who are interested in starting an Oxford House (Level I). To qualify for residency, individuals must contribute to rent and expenses and the daily functions of the household, as well as remain sober from alcohol and drugs. However, individuals are not provided any additional supports. Other level II, III, and IV recovery homes that offer more intensive services are available in Texas but remain less common. Often, individuals complete a residential or detoxification program prior to residency. Individuals who have financial barriers and who have completed an HHSC-funded program are eligible for stipends to offset move-in fees.
Other recovery housing data is not collected across the state for homes that are provided through the private sector, or public-private partnerships. During the 86th legislative session, HB 1465 (Moody/Menendez) was filed to study and evaluate recovery housing. The study would have required details on the current status, opportunities, challenges, and needs of recovery housing throughout the state. While passed in the House, HB 1465 was unable to pass the Senate before the conclusion of the legislative session. Without legislative direction, HHSC distributed a housing survey in May 2020 to collect data on the housing needs of people with mental health conditions, substance use histories and/or intellectual and developmental disabilities to create a Texas Housing Choice Plan.
RECOVERY SUPPORT SERVICES
In 2010, Texas began to shift from addressing substance use conditions with an acute care model and instead focus on recovery. HHSC established a series of local community networks to collaborate in identifying strengths and obstacles for individuals in recovery, and to improve the local environment to support recovery. These local Recovery-Oriented Systems of Care (ROSCs) were the framework for a long-term systems transformation. Beginning with an initial effort in Houston, HHSC facilitated meetings to organize and support ROSCs in communities throughout Texas. Currently there are 22 ROSCs operating across the state. The Houston ROSC was planned and supported by HHSC and the University of Texas Addiction Research Institute (ARI), and has served as a model for other sites across Texas. A report of this initial Houston ROSC effort may be found at https://socialwork.utexas.edu/dl/files/cswr/institutes/ari/pdf/Houston-ROSC-Phase-I.pdf
Recovery Support Service (RSS) Project
In 2014, HHSC continued the transition to a recovery-focused system by issuing an RFA to provide recovery support services to individuals across the state. The RFA was open to SUD treatment organizations (TOs), peer-run Recovery Community Organizations (RCOs), and other community-based organizations (CBOs) that have a history of providing SUD services to individuals and family members. The result was a network of 22 recovery support service organizations (RSSOs), collectively known as the Recovery Support Services (RSS) Project.
RSSOs deliver a wide array of non-clinical, peer-provided services to help individuals initiate, support, and maintain recovery. Services are provided by peers, including peer support specialists and peer recovery coaches, that help initiate services like counseling, sober housing, transportation and medications. Individuals with a history of substance use or abuse, including co-occurring mental health conditions, who are in or seeking recovery, along with their family members and significant others are eligible to receive recovery support services at an RSSO.
One of the key elements in the project was the recruitment and utilization of peer recovery coaches. Services also include peer-run groups; development and/or use of recovery homes and recovery schools; life skills training such as financial management, parenting, employment and stress management; educational support; recovery check-ups; and connections to mutual aid support groups. HHSC contracted with the Addiction Research Institute at the Steve Hicks School of Social Work at UT to evaluate the RSS Project from May 2014-July 2018. The number of services provided by the 22 RSSOs are shown through Figure 50, Figure 51, Figure 52, and Figure 53. The full report can be found at https://socialwork.utexas.edu/dl/ari/recovery-support-services-report-2018.pdf
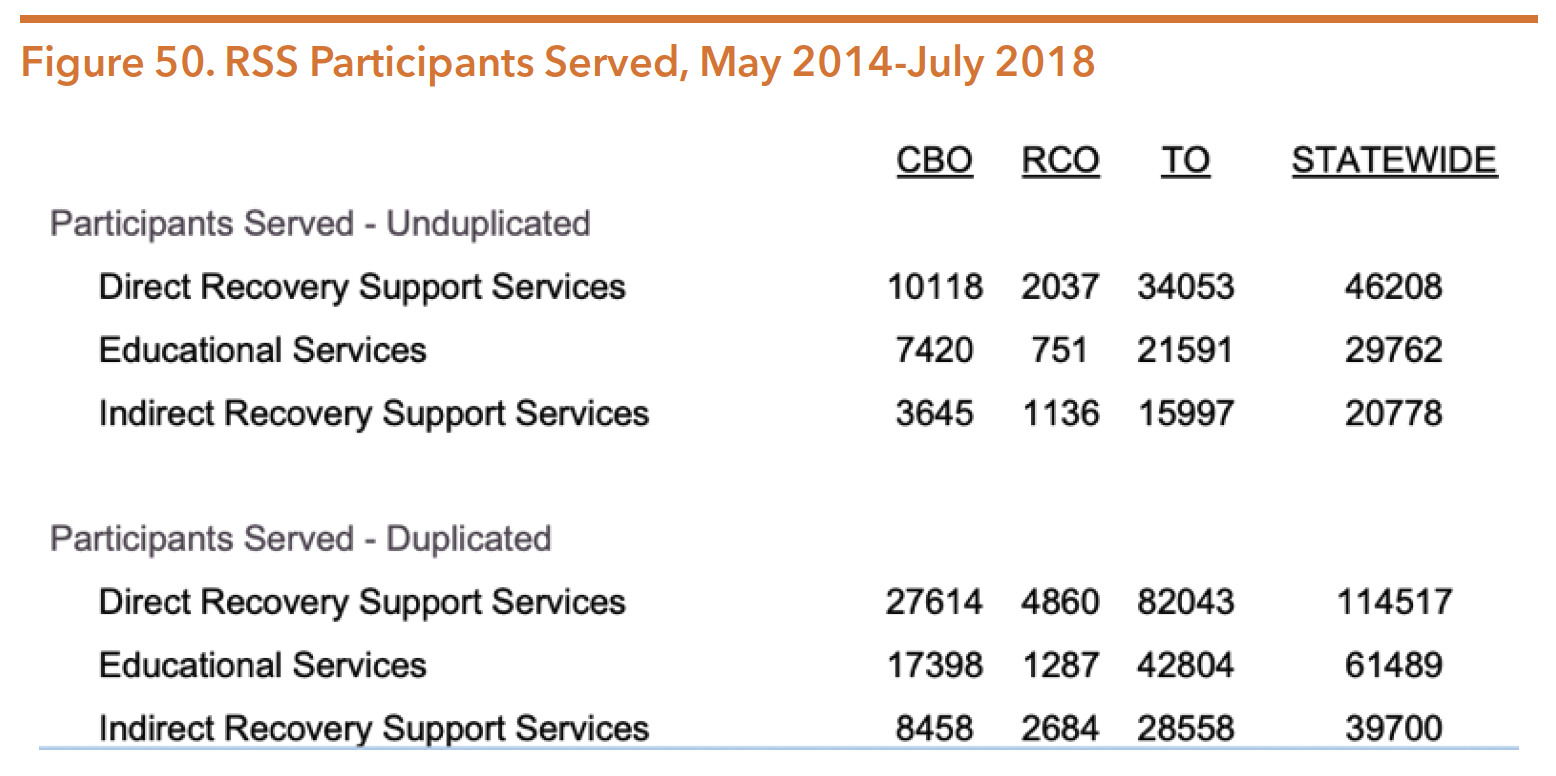
Source: Mangrum, L., Spence, R., Nichols M., &Petersen, C. (2018). HHSC contract no. 2017-049621-001, recovery support services project, fiscal year 2018 interim process evaluation report. The University of Texas Steve Hick School of Social Work, Addiction Research Institute: Austin, TX. Retrieved from https://socialwork.utexas.edu/dl/ari/ recovery-support-services-report-2018.pdf
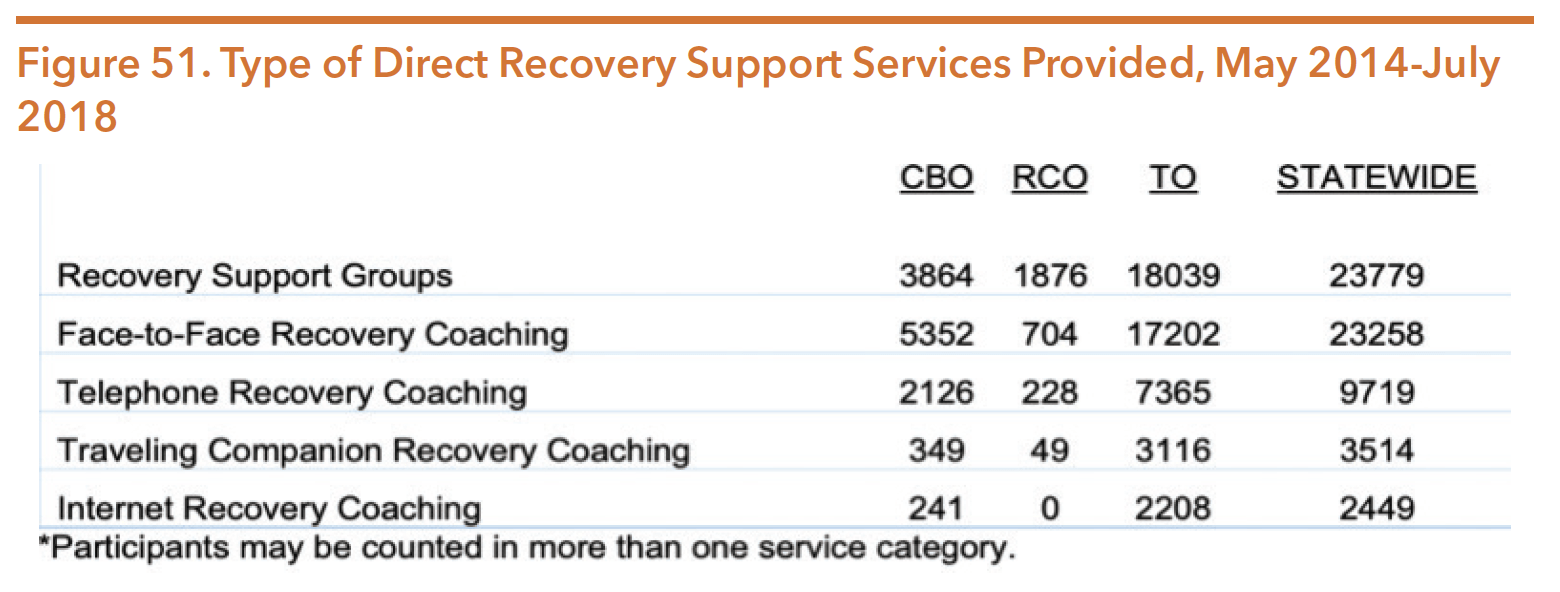
Source: Mangrum, L., Spence, R., Nichols M., & Petersen, C. (2018). HHSC contract no. 2017-049621-001, reco very support services project, fiscal year 2018 interim process evaluation report. The University of Texas Steve Hick School of Social Work, Addiction Research Institute: Austin, TX. Retrieved from https://socialwork.utexas.edu/dl/ari/recovery-support-services-report-2018.pdf
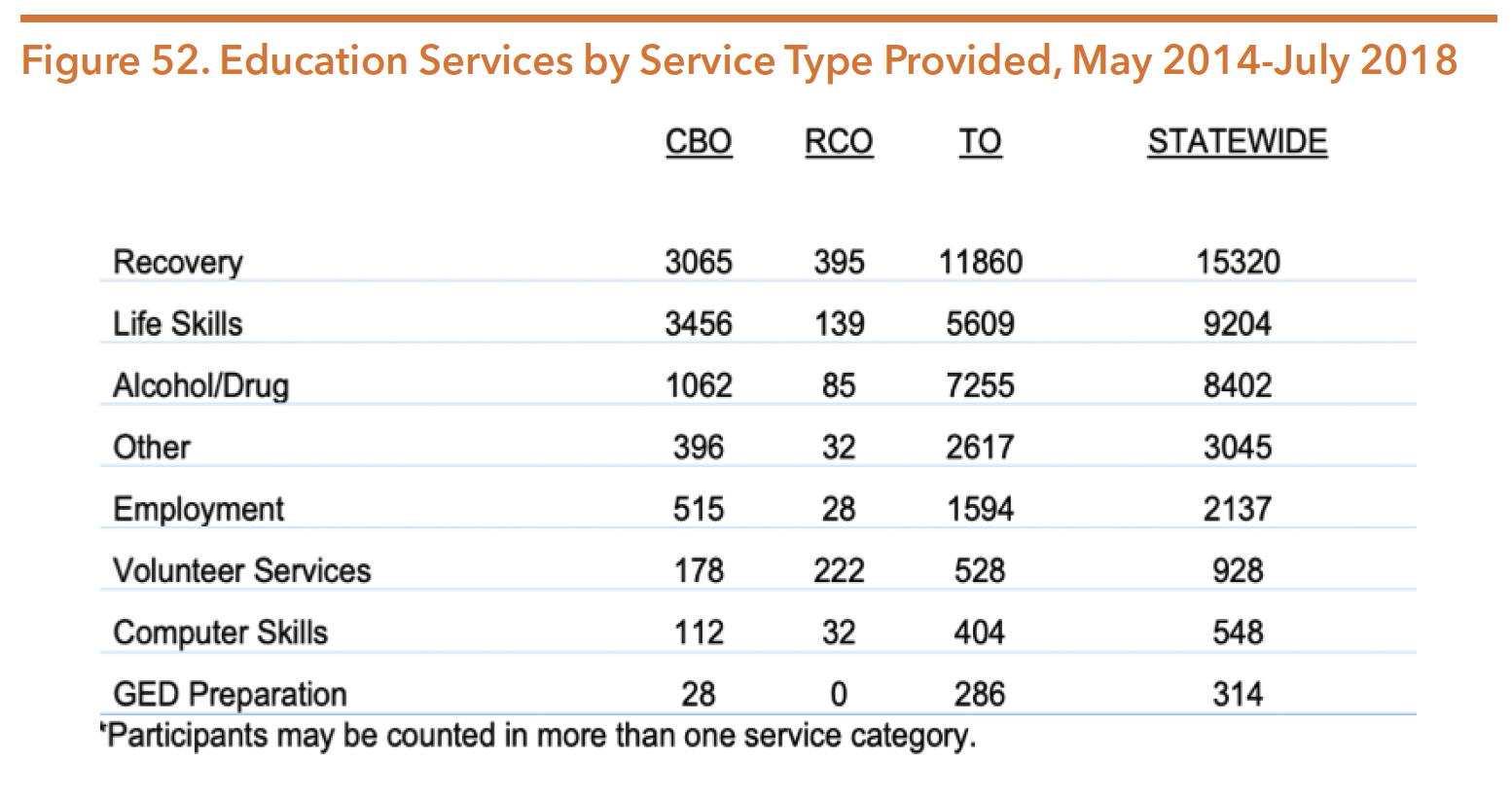
Source: Mangrum, L., Spence, R., Nichols M., &Petersen, C. (2018). HHSC contract no. 2017-049621-001, reco very support services project, fiscal year 2018 interim process evaluation report. The University of Texas Steve Hick School of Social Work, Addiction Research Institute: Austin, TX. Retrieved from https://socialwork.utexas.edu/dl/ari/recovery-support-services-report-2018.pdf
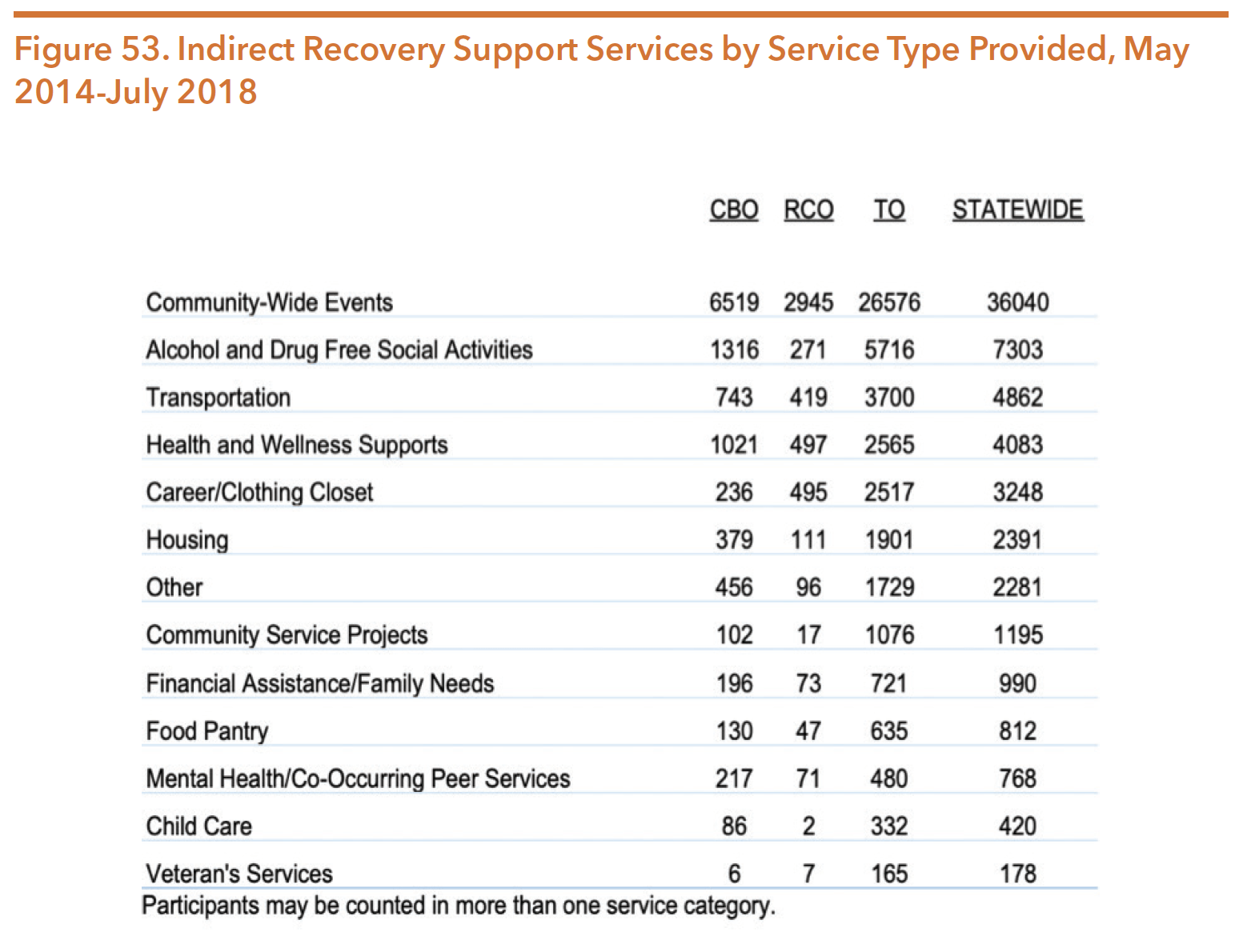
Source: Mangrum, L., Spence, R., Nichols M., &Petersen, C. (2018). HHSC contract no. 2017-049621-001, recovery support services project, fiscal year 2018 interim process evaluation report. The University of Texas Steve Hick School of Social Work, Addiction Research Institute: Austin, TX. Retrieved from https://socialwork.utexas.edu/dl/ari/recovery-support-services-report-2018.pdf
As of May 2020, 21 RSSOs continue to operate across the state of Texas. HHSC provides a list of the RSSOs in Texas that can be accessed at https://hhs.texas.gov/services/mental-health-substance-use/adult-substance-use/adult-substance-use-recovery-support-service-organizations
Recovery Support Peer Services
Recovery coaches are an integral part of recovery support services for someone in recovery. After the passage of HB 1486 (85th, Price/Schwertner), services offered by certified recovery support peers became eligible for Medicaid reimbursement. As of August 2020, there were 246 certified recovery coaches across the state.
In Texas, one long-term study focusing on substance use condition peer specialists in Texas, also called recovery coaches, demonstrated exciting results at 12 months:
- Housing status improved, with 54 percent of long-term coaching participants owning or renting their own living quarters after 12 months, compared to 32 percent at enrollment.
- Overall employment increased to 58 percent after 12 months from 24 percent at enrollment.
- Average wages increased to $879 per month after 12 months from $252 at enrollment.
- Healthcare utilization dropped after 12 months of recovery coaching:
- Outpatient visits dropped to 815 visits from 4,118 at enrollment
- Inpatient care days dropped to 1117 days from 9,082 at enrollment
- Emergency room visits dropped to 146 from 426 at enrollment
In total, recovery coaching saved $3,422,632 in healthcare costs, representing a 72 percent reduction in costs over 12 months.
HHSC provides information on peer support services, the certification process, and benefits of peer supports which can be found at https://hhs.texas.gov/doing-business-hhs/provider-portals/behavioral-health-services-providers/peer-support-services
Additional information on peer services in Texas can be found in the Policy Environment Section.
SCHOOL AND COMMUNITY BASED PREVENTION
School and community-based substance use prevention programs are funded through HHSC’s Medical and Social Services Division-Behavioral Health Services section. HHSC currently funds 225 programs statewide to address the state’s four prevention priorities: underage alcohol use, underage tobacco and nicotine products use, marijuana and other cannabinoid use, prescription drug misuse, and the use and misuse of other drugs and substances. The following description of available programs was captured from the HHSC website: https://hhs.texas.gov/about-hhs/process-improvement/improving-services-texans/behavioral-health-services/substance-use-misuse-prevention
Substance Use and Misuse Prevention
Community Coalition Partnerships – Programs that work in the community to engage and mobilize various sectors to implement evidence-based environmental strategies with a primary focus on changing policies and influencing social norms related to substance use and misuse.
Prevention Resource Centers – Centers work to increase the capacity of the statewide substance use and misuse prevention system by enhancing community collaboration, increasing community awareness and readiness, providing information and resources on substance use and related behavioral health data, supporting professional development of the prevention workforce, and providing resources for evaluation activities within each service region. Prevention Resource Centers also support the federal Synar requirement by conducting voluntary tobacco retail compliance checks throughout the state to help reduce youth access to tobacco and other nicotine products.
Youth Prevention Indicated – Provide strategies and interventions aimed to address people with initiative behaviors and related risk factors with an elevated risk for substance use and misuse. While the target population might show early signs of substance use and misuse, indicated services are not designed for people with a diagnosable substance use condition.
Youth Prevention Selective – Provide strategies and interventions that address specific subgroups of the general population known to have risk factors that increase the likelihood of substance use and misuse.
Youth Prevention Universal – Provide strategies and interventions that address the general public or a segment of the entire population with average probability of developing a substance use condition, risk or condition.
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES SERVICES
The Intellectual and Developmental Disabilities Services division oversees intellectual and developmental disability services provided by Local Intellectual and Developmental Disability Authorities (LIDDAs). Prior to the HHS system transformation required by the 2015 legislature, IDD services were located within the Department of Aging and Disability Services (DADS). DADS functions moved to HHSC and the Texas Workforce Commission (TWC) and the agency dissolved.
MENTAL HEALTH NEEDS OF INDIVIDUALS WITH INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
Intellectual and developmental disabilities (IDD) can often overshadow existing mental health or medical conditions. Professionals, caregivers, and family members who are accustomed to seeing an individual through the lens of their disability can misinterpret behaviors that may be associated with mental health conditions, distress, acute medical conditions, or trauma.
Many systems of care for people with IDD continue to focus on controlling and managing behaviors without considering whether underlying mental health conditions, medical conditions, or trauma cause the behaviors. The focus of treatment has often been the development of behavior management plans to promote compliance or the use of medications to control the behaviors. In both cases, the treatment is targeting the behavior and not the actual mental health or medical condition. Often, the first line of “treatment” is psychopharmacological; psychotropic drugs are frequently used to control behaviors, which may address the symptoms but not the illness. Psychotropic medications also have the potential to exacerbate existing challenges, which significantly reduces opportunities for recovery.
Individuals with disabilities can experience all mental health conditions and require access to quality mental health services. People with disabilities, while at a higher risk of having mental health conditions than the general population, often experience significant disparities in their ability to access needed services. People with IDD frequently experience trauma, yet rarely are systems, programs, or policies for people with IDD developed based on recovery and trauma-informed principles. Further, goals and objectives of state agency and healthcare systems rarely address or promote a focus on mental wellness. The mental health needs of people with intellectual disabilities are routinely overlooked in the research and these individuals often do not receive quality mental health treatment.
Further, while HHSC has integrated recovery-focused interventions into its mental health system, the HHS enterprise has not yet incorporated the principles of recovery into the service provision culture for individuals with IDD. Individuals with IDD and older adults who have mental health conditions can benefit from recovery-focused interventions that are embedded in a culture of hope and resilience.
PREVALENCE OF MENTAL HEALTH CONDITIONS FOR PEOPLE WITH DISABILITIES
The coexistence of an intellectual or developmental disability along with a mental health condition is one type of dual diagnosis. Persons with IDD often experience dual diagnoses at higher rates than the general public. As many as 30 to 40 percent of individuals with intellectual disabilities are diagnosed with mental health conditions, and they are three to five times more likely to have a dual diagnosis with a psychiatric disability. Individuals with IDD who have a dual diagnosis or who present behavioral “challenges” are more likely to be institutionalized and are often the last to be released to a community-based setting. Additionally, community services and supports are frequently incapable of meeting the behavioral health needs of these individuals, leading to less successful outcomes when transitioning into the community.
Children with IDD are more likely to have experienced traumatic events including emotional, physical, or sexual abuse, neglect, and maltreatment when compared to able-bodied peers. While many individuals with IDD have known histories of abuse (some research suggesting nearly 30 percent), the rate may be higher because of underreporting or lack of recognition by family and other caregivers.
While trauma is not the only cause of mental health challenges in people with disabilities, it is significant and requires attention. Adults and children with disabilities experience abuse, neglect, institutionalization, abandonment, bullying, and other types of trauma at rates higher than the general population. In one study, nearly 75 percent of participants with IDD experienced at least one traumatic event in their lifetime, increasing the likelihood of developing a mental health condition.
The higher prevalence of mental health conditions among people with disabilities may also be linked to psychological stress related to a disability, social isolation, trauma, institutionalization, bullying, low self-esteem, and other factors.
CHANGING THE PARADIGM
The conversation continues to shift from simply trying to “manage” behaviors to prioritize, recognize and address the mental health and trauma needs of individuals with IDD. The Hogg Foundation for Mental Health partnered with the National Child Traumatic Stress Network to develop The Road to Recovery: Supporting Children with IDD Who Have Experienced Trauma. This is a two-day, training curriculum and toolkit that is available free of charge online. The Hogg Foundation previously funded a three-year grant to provide the training statewide. A current grant awarded to the Center for Disability Studies at the University of Texas at Austin will develop “master trainers” to ensure that the training is available statewide. The toolkit is available on the NCTSN website at https://learn.nctsn.org/enrol/index.php?id=370. Registration and login are required, but the product is available to the public.
HHSC has begun to recognize the importance of addressing the mental health needs of individuals with IDD. Two web-based training series have been developed and are offered free of charge online. The series, Mental Health Wellness for Individuals with Intellectual and Developmental Disabilities (MHW-IDD), includes a series of six modules for direct service workers and a series of three modules for healthcare professionals. All modules are available at http://training.mhw-idd.uthscsa.edu/.
The course for direct service workers consists of the following six modules:
- Co-occurring conditions: Intellectual and Developmental Disabilities and Mental Illness
- Trauma Informed Care for Individuals with IDD
- Functional Behavioral Assessment and Behavior Support
- Overview of Genetic Syndromes Associated with IDD
- Overview of Other Medical Diagnoses Associated with IDD
- Putting it all Together: Supports and Strategies for Direct Service Workers
The series for healthcare professionals includes:
- Integrated Healthcare for Individuals with Intellectual and Developmental Disabilities
- Communicating with Individuals with Intellectual and Developmental Disabilities
- Trauma-Informed Care for Clinical Providers
STATEWIDE IDD STRATEGIC PLAN
HHSC worked with stakeholders across Texas and identified a need to develop a comprehensive Statewide IDD Strategic Plan, given the unique challenges faced by people with IDD across the state’s human services systems. A Foundation of the Statewide IDD Strategic Plan was developed alongside the second edition of the Texas Statewide Behavioral Health Strategic Plan. The Foundation of the Statewide IDD Strategic Plan is the first phase in order to lay the groundwork for the full plan and includes an overview of the IDD population in Texas; statewide IDD gap survey results; and an IDD program inventory. Through the gap survey, behavioral health services were identified. Figure 54 shows the largest gap identified was enhanced services and service coordination when an individual has co-occurring IDD and behavioral health concerns. The Statewide IDD Strategic Plan is expected to be finalized by late 2020.
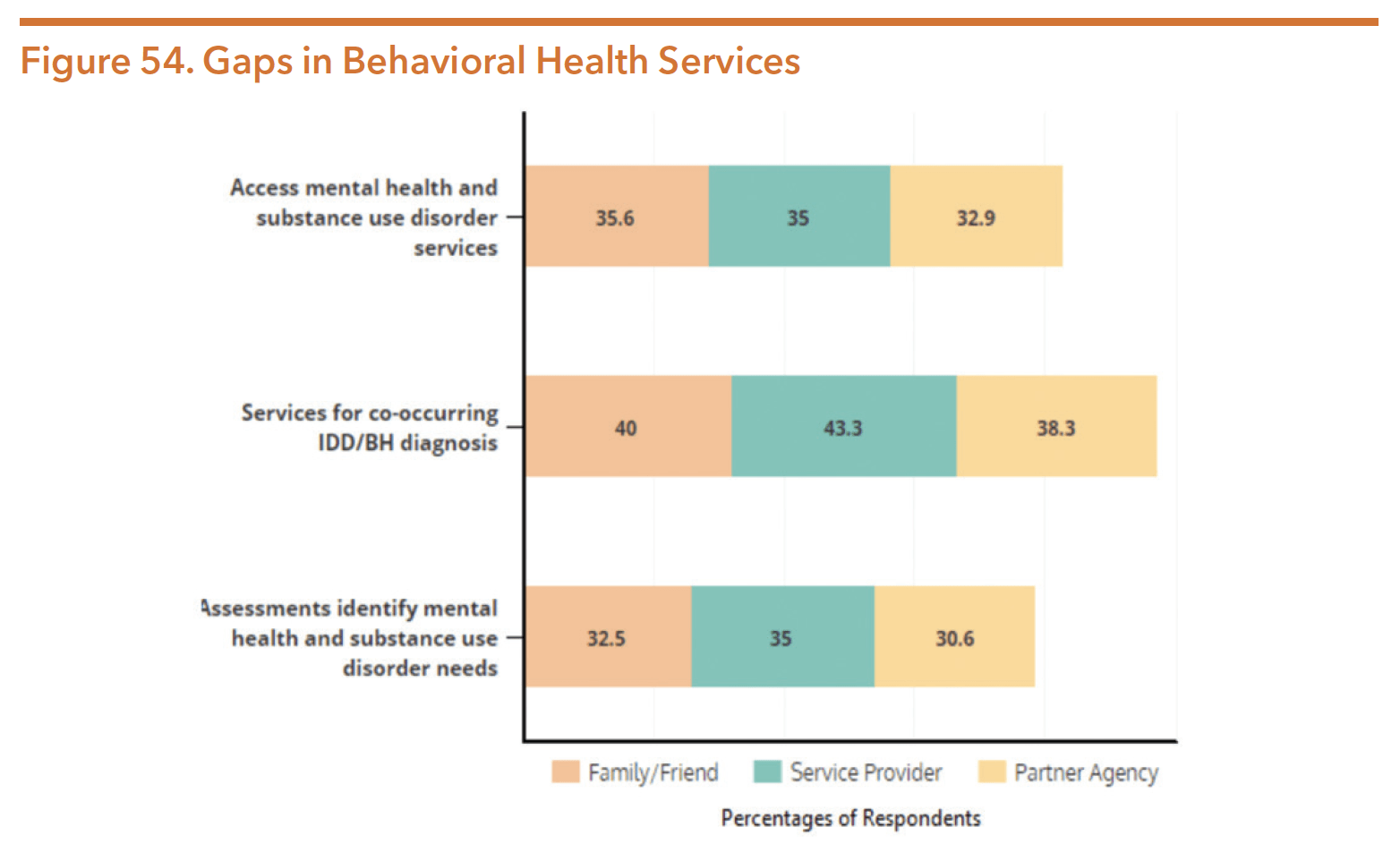
Source: Texas Health and Human Services, Statewide Behavioral Health Coordinating Council. (February 2019). Texas statewide behavioral health, fiscal years 2017-2021: Strategic plan update and the foundation for the IDD strategic plan. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2019/hb1-statewide-behv-hlth-idd-plan-feb-2019.pdf
PROGRAMS AND SERVICES FOR PEOPLE WITH DISABILITIES WHO HAVE CO-OCCURRING BEHAVIORAL HEALTH CONDITIONS
Prior to the 86th legislative session, HHSC identified that providing coordinated behavioral health care for individuals with disabilities was an important initiative for the state in their legislative appropriations request. HHSC requested an exceptional item for funding the establishment of new IDD community outpatient mental health services at local intellectual/developmental disability authorities (LIDDAs) to provide integrated physical and behavioral health services for people with IDD. Only a small fraction of the commission’s legislative exceptional item request to fund these community mental health services for individuals with IDD was actually funded.
Long-term Services and Supports (LTSS) programs serve populations that are aging, have physical disabilities, and have IDD, including those who have co-occurring behavioral health conditions. Services and supports are provided through a variety of community-based and institution-based programs. The services are funded through various federal and state funding sources.
Long-term Services and Supports Funding
Funding for LTSS programs and services comes from both the federal and state governments. These figures include funding for an array of LTSS services, both community-based and institutional care, and are not limited to funding for mental health services.
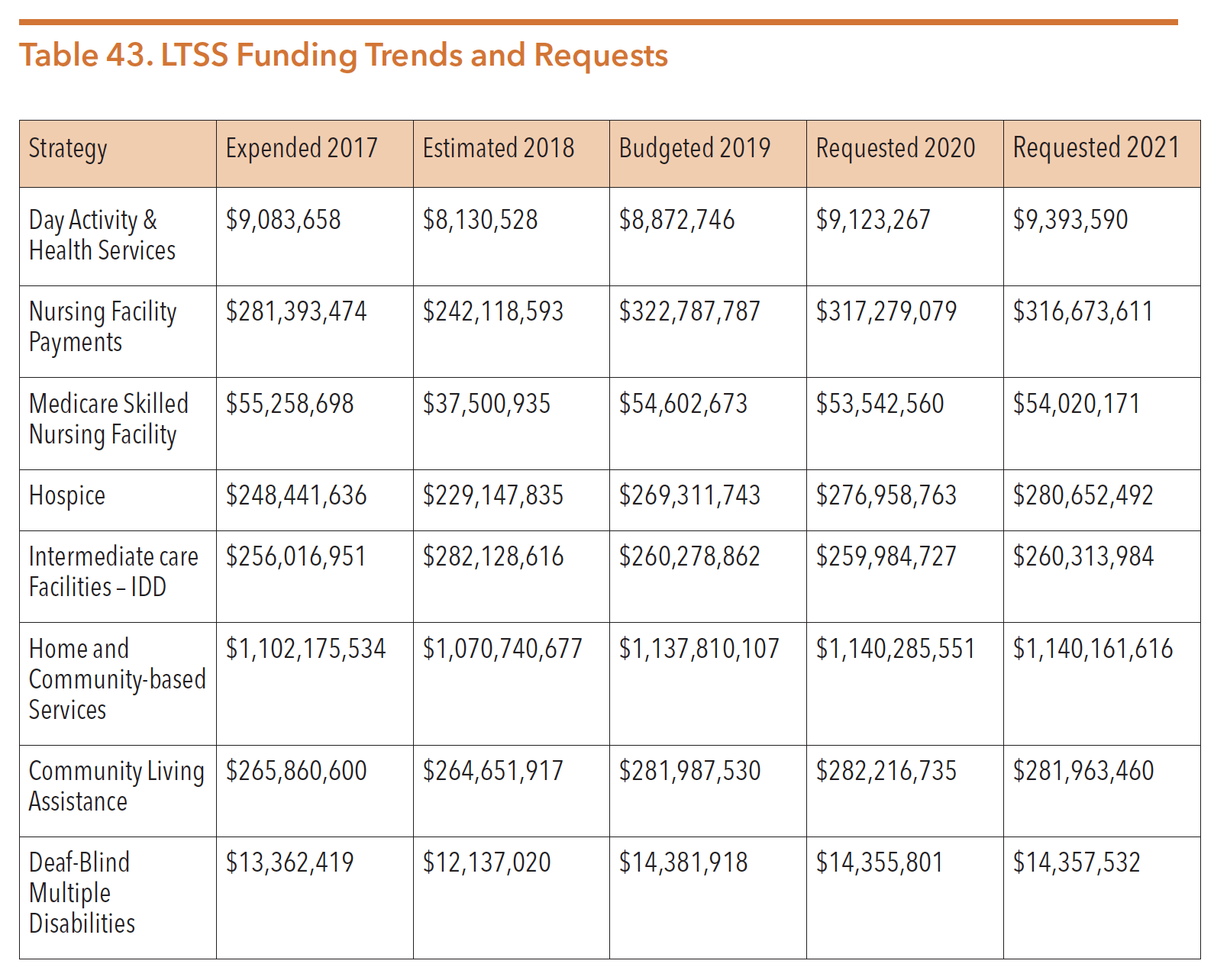
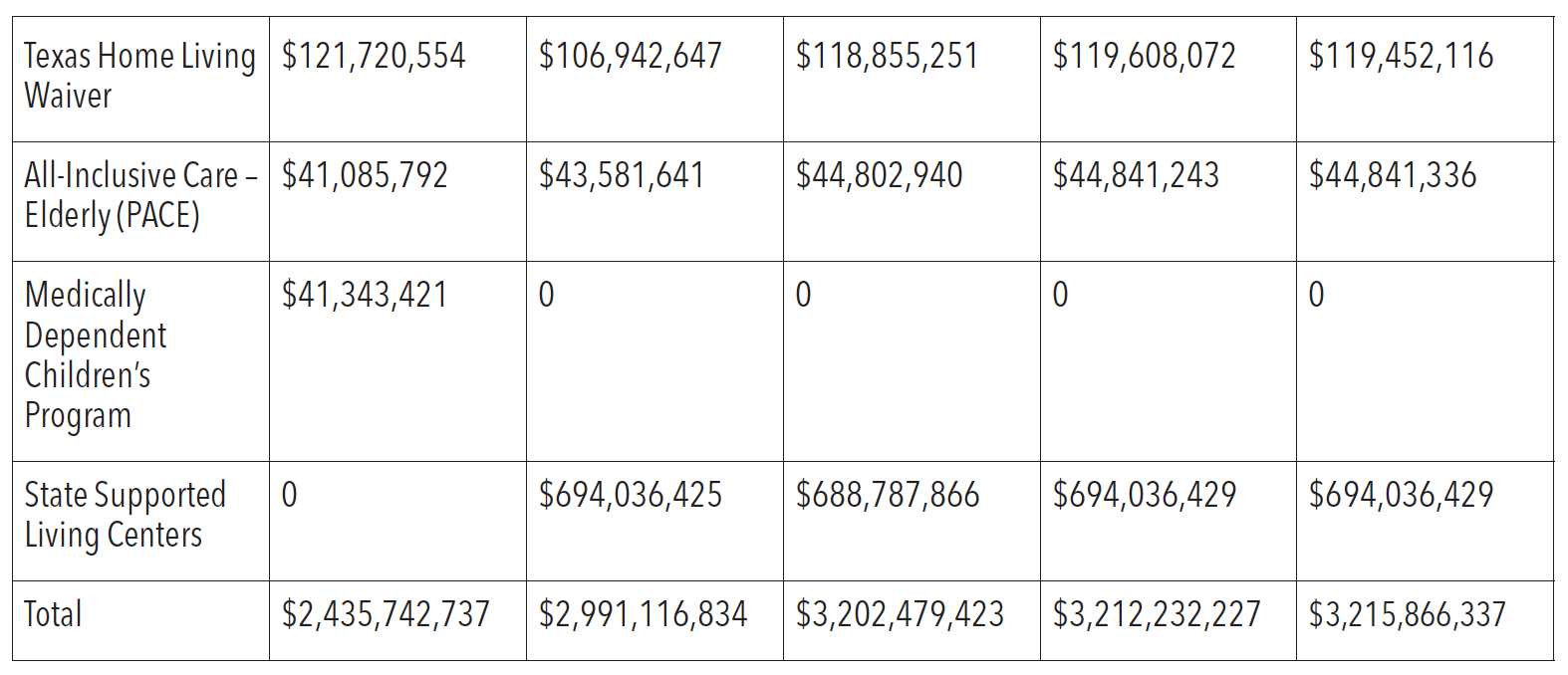
Source Legislative Budget Board. (2018). Health and Human Services Commission Legislative Appropriations Request, FY 2020-21. Retrieved from http://www.lbb.state.tx.us/Agency_Docs.aspx.
Note: The funding reflected in this table is included in the total Medicaid appropriation provided in the Medicaid section.Note: Data on costs for behavioral health services in these programs is unavailable.
In addition to Medicaid and Medicaid waiver services, HHSC is responsible for the administration of community LTSS. The majority of Texans with disabilities receive services in a community-based setting. Many of these programs provide needed services to people with disabilities and co-occurring behavioral health challenges. Older Texans meeting the medical criteria for nursing home services may also be eligible for community-based services funded by HHSC if they meet financial eligibility criteria. Some of the major community service programs are described below.
Medicaid 1915(c) Waiver Services
HHSC administers the 1915(c) Medicaid Home and Community-based Services waiver programs, which are designed to provide community supports and services to individuals eligible for institutional care (i.e., nursing facilities or intermediate care facilities). These waivers prevent the institutionalization of people with disabilities by providing appropriate community services and supports.
As opposed to institution-based care, access to these waiver services is not an entitlement and each program currently has a significant interest list. Legislative appropriations determine the number of people receiving services in these programs (i.e., funded waiver slots). The wait time for services varies by program but can be anywhere from one to fifteen years. Figure 55 provides the number of years percentages of individuals have been on a waitlist as of July 2020 for each program.
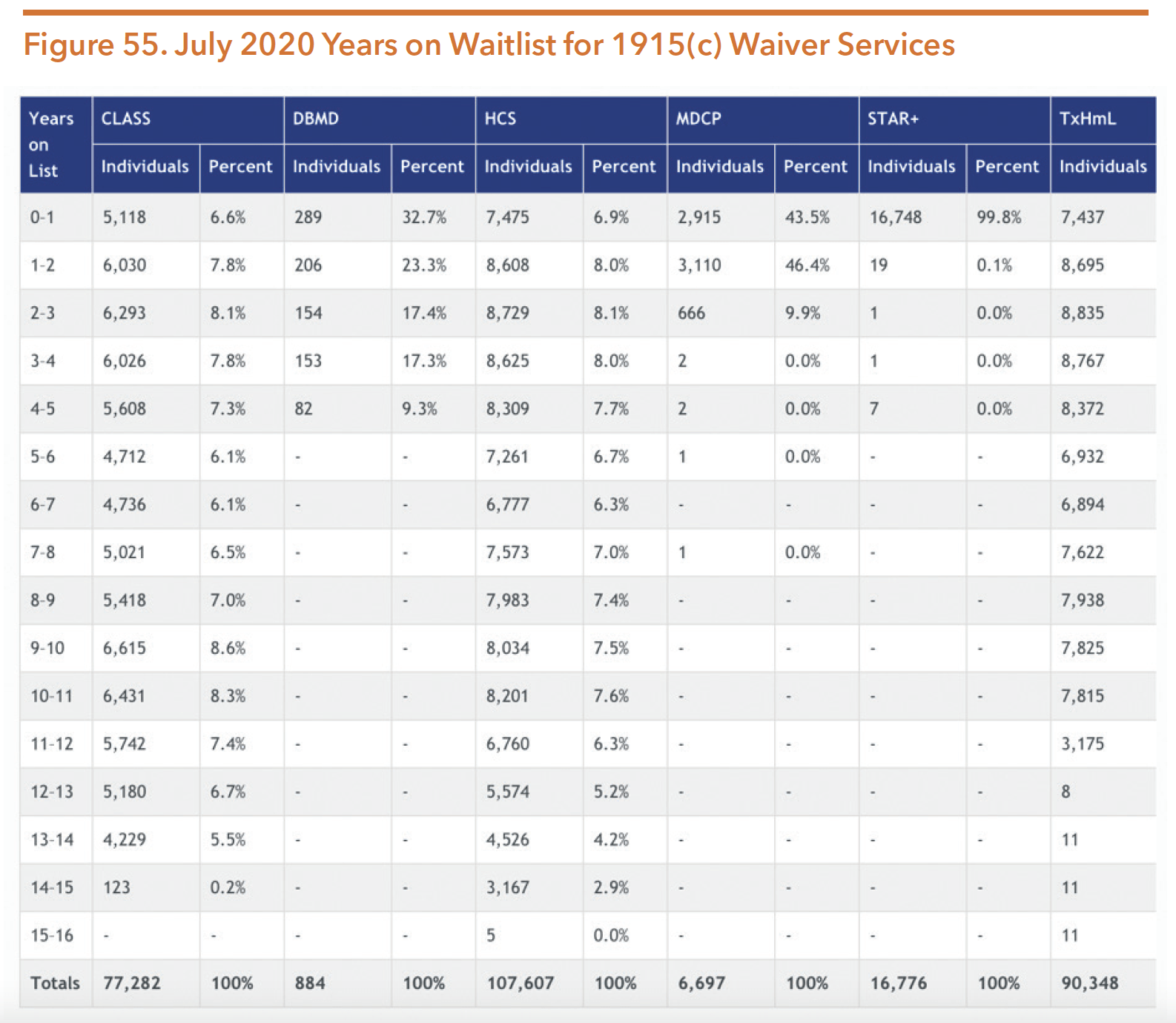
Source: Texas Health and Human Services. (2020). Interest list reduction. Retrieved from https://hhs.texas.gov/about-hhs/records-statistics/interest-list-reduction
Table 44 provides basic information about eligibility and services for the primary waivers for persons with intellectual and other developmental disabilities.
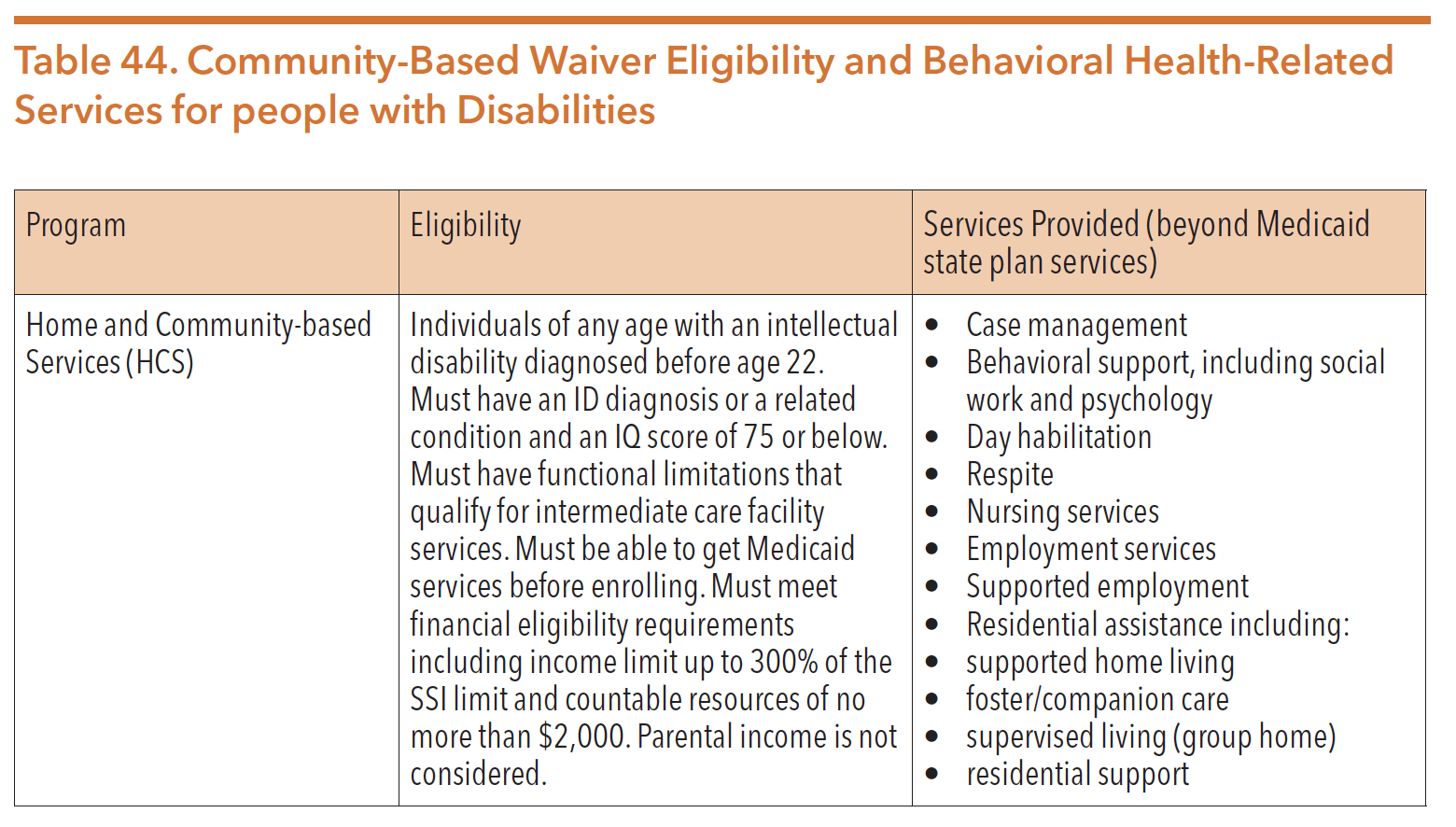
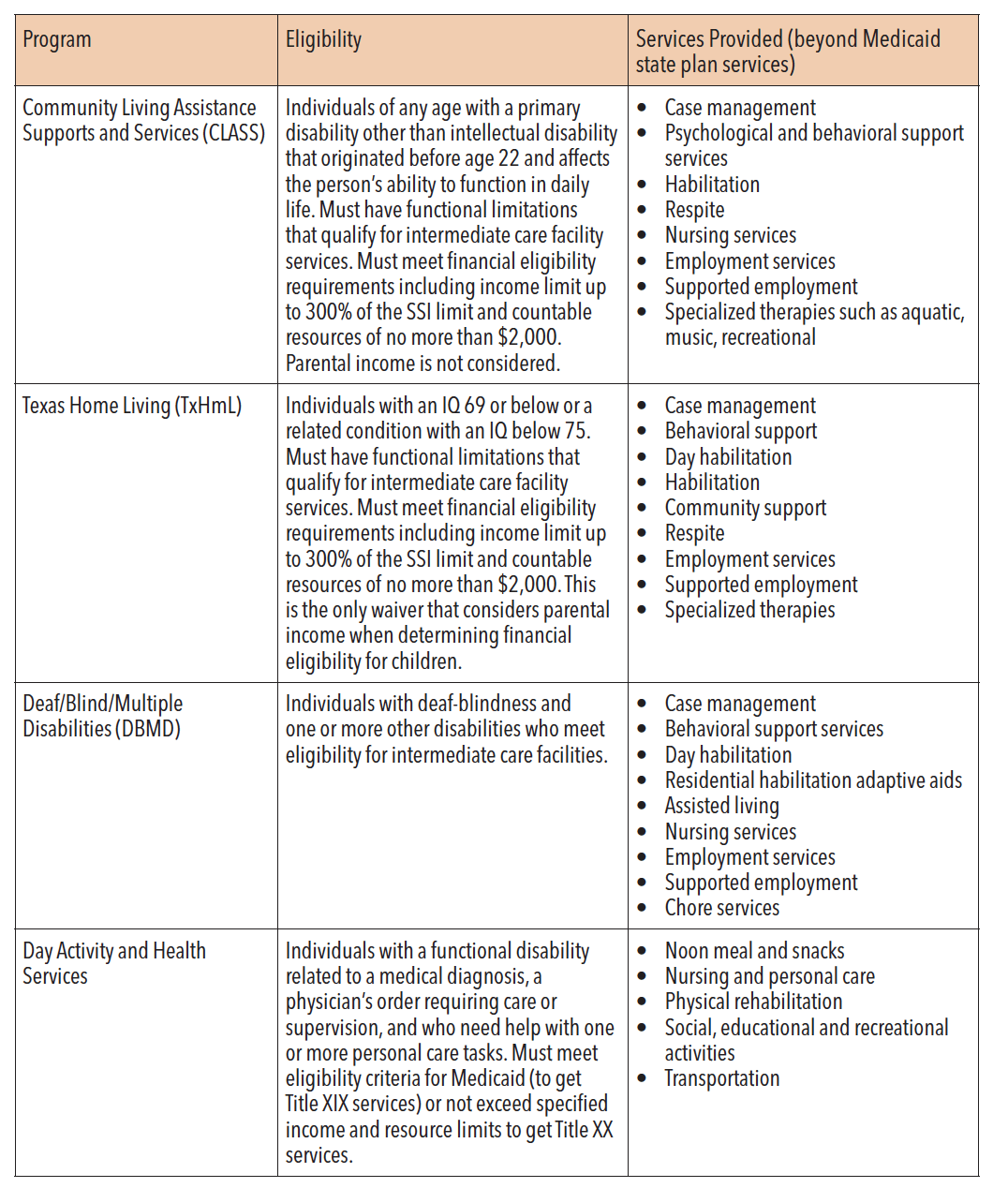
Sources: Texas Health and Human Services. (2017). Texas Long-Term Service and Supports (LTSS) Waiver Programs. Retrieved from https://hhs.texas.gov/sites/default/files//documents/doing-business-with-hhs/providers/resources/ltss-waivers.pdf
Navigate Life Texas. (n.d.). Waivers. Retrieved from https://www.navigatelifetexas.org/en/insurance-financial-help/texas-medicaid-waiver-programs-for-children-with-disabilities
Paying for Senior Care. (2018). Day Activity and Health Services (DAHS) Program: Texas Medicaid Adult Day Care. Retrieved from https://www.payingforseniorcare.com/adult-day-care/tx-dahs-program.html
As part of the 2020-21 biennial budget, the 86th Legislature passed Rider 20 directing HHSC to create a plan for slot enrollment and allocated $66,661,790 in All Funds, with $24,792,919 in General Revenue to expand community-based services. New waiver slots were allocated as follows:
- 1,320 HCS slots;
- 240 CLASS slots
- 8 DBMD slots; and
- 60 Medically Dependent Children Program slots.
Table 45. depicts HHSC’s planned slot enrollment for the 2020-21 biennium.
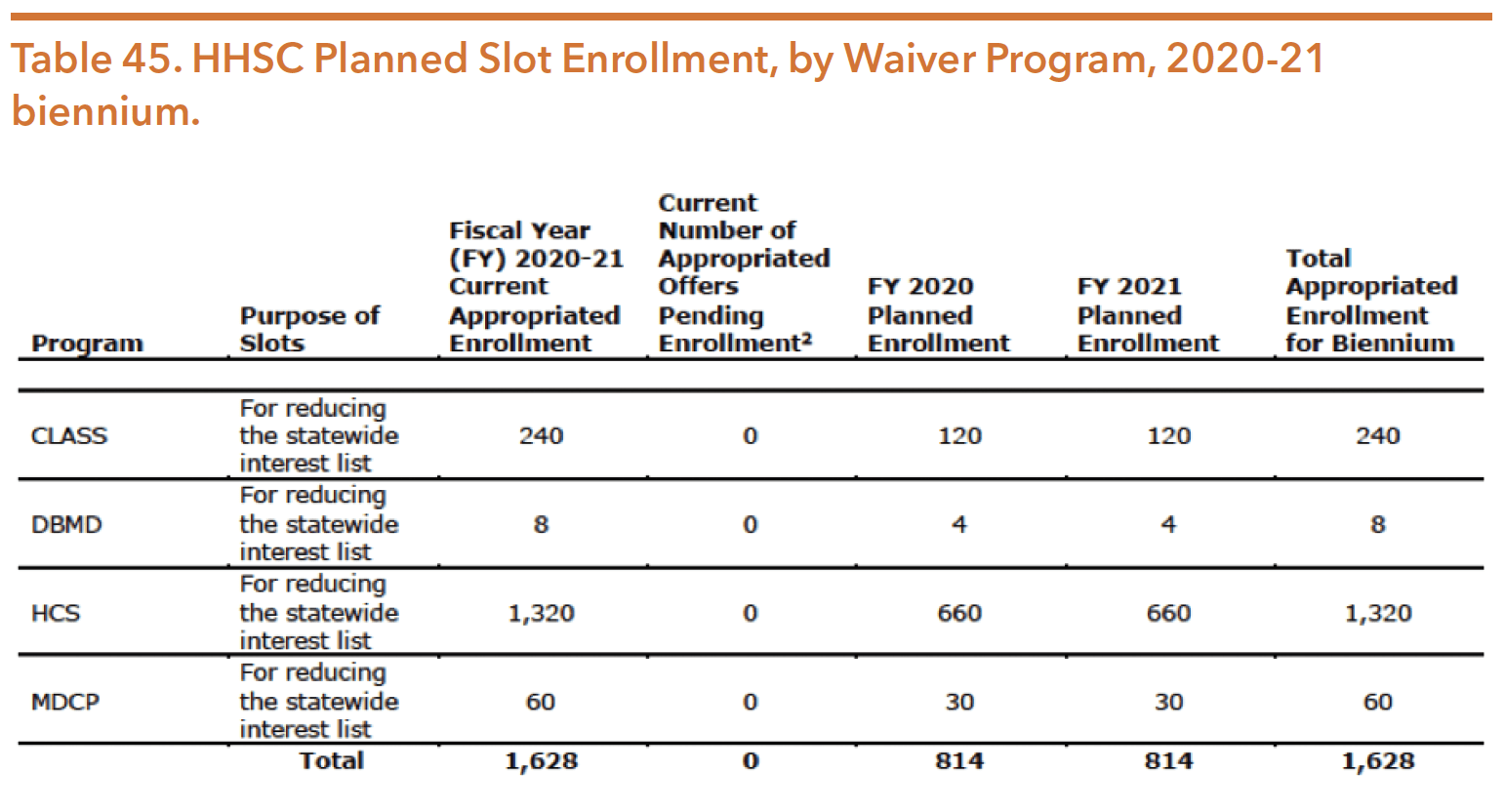
Source: Texas Health and Human Services. (October 2019). Waiver slot enrollment plan report. Retrieved from https://hhs.texas.gov/reports/2019/10/waiver-slot-enrollment-plan-report
The demand for community-based services and supports often outweighs available resources, and applicants’ names are placed on an interest list until services are available. However, some needs may be met through other programs until an applicant’s name comes to the top of the list. Senate Bill 1207 (86th, Perry/Krause) required HHSC to change what is considered in the enrollment process for the MDCP and DBMD programs. The legislation also required HHSC to permit an individual who is no longer eligible for MDCP to be placed either at the top of the MDCP interest list or be placed on another interest list using the date they originally applied for the MDCP interest list.
The 86th Texas Legislature also directed funds to be used to conduct a study of the interest or other waiting list for the HCS, CLASS, DBMD, MDCP, and TxHmL waivers, as well as STAR+PLUS. Figure 56 shows the waiting list reduction summary for July 2020. The total of interest list counts in the below table is a duplicated count. The unduplicated count across all six Interest Lists is 163,998. HHSC was directed to study interest lists and consider how other states are addressing these waitlists, policies impacting the lists, demographic data of individuals on the lists, and strategies HHSC could employ to eliminate the lists. The report from HHSC was submitted to the Legislative Budget Board (LBB) and the Governor in September 2020 and can be found at: https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/medicaid-waiver-programs-interest-list-study-sept-2020.pdf
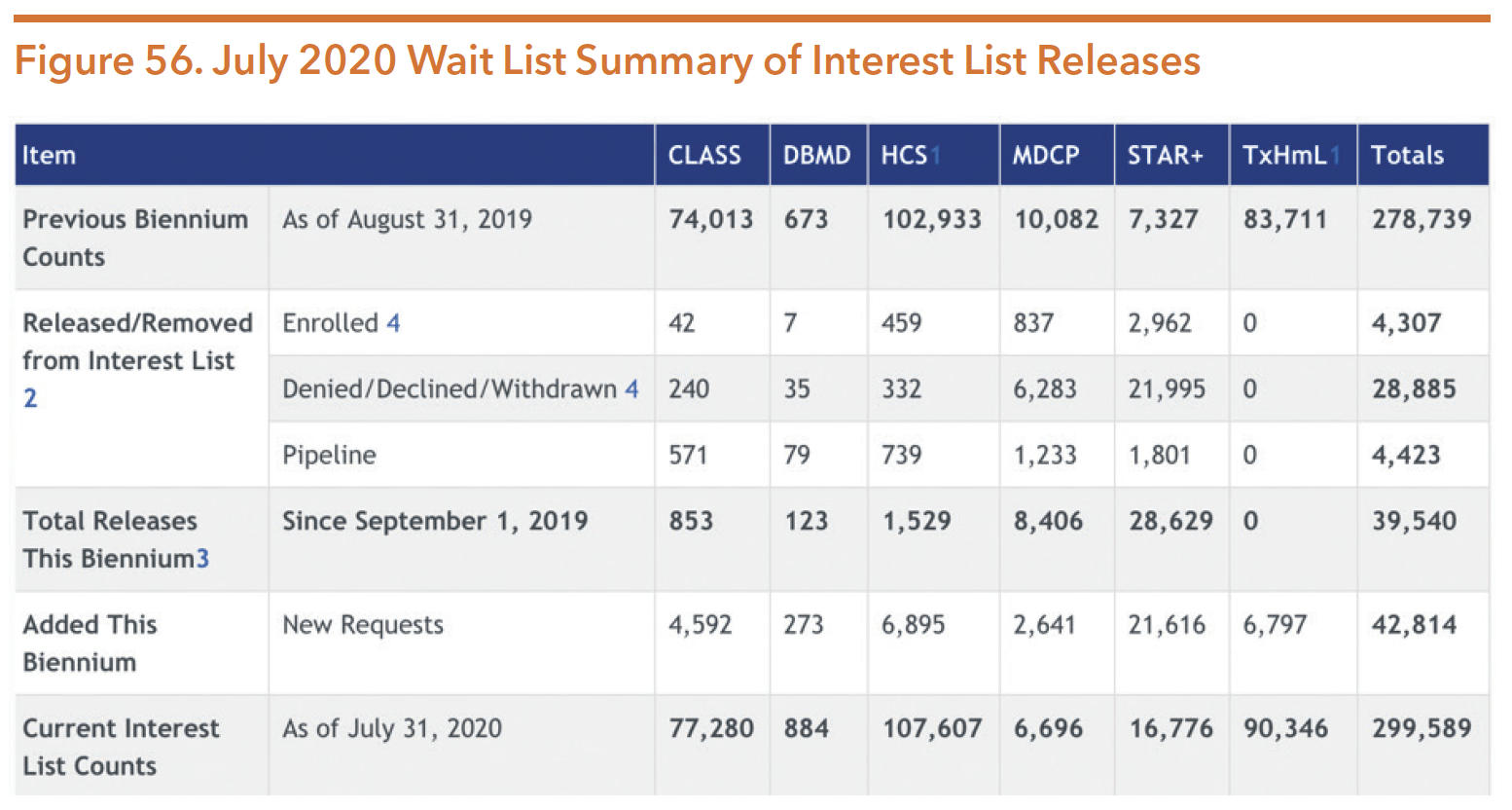
Source: Texas Health and Human Services. (2020). Interest list reduction. Retrieved from https://hhs.texas.gov/about-hhs/records-statistics/interest-list-reduction
Table 46 shows a three-year trend of each Medicaid 1915(c) waiver program serving individuals with a co-occurring mental health condition from FY 2013-2105. This was previously the most updated data However, in July 2020, the Behavioral Health Advisory Council requested an update and HHSC was able to provide data for 09/01/18 – 08/31/19 shown in Figure 57.
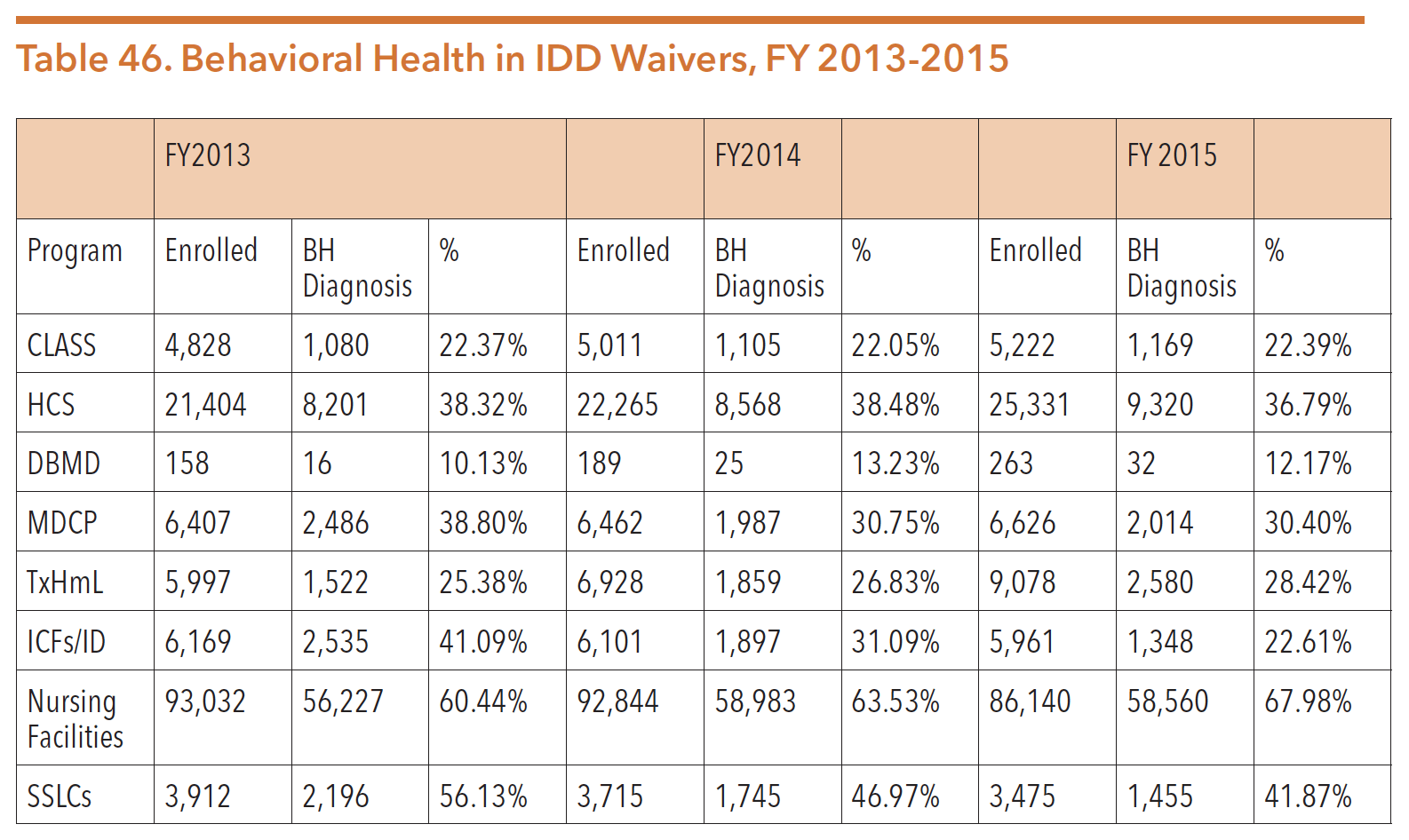
Source: Department of Aging and Disability Services. (2016, October 3). Data Request: People enrolled in DADS programs.
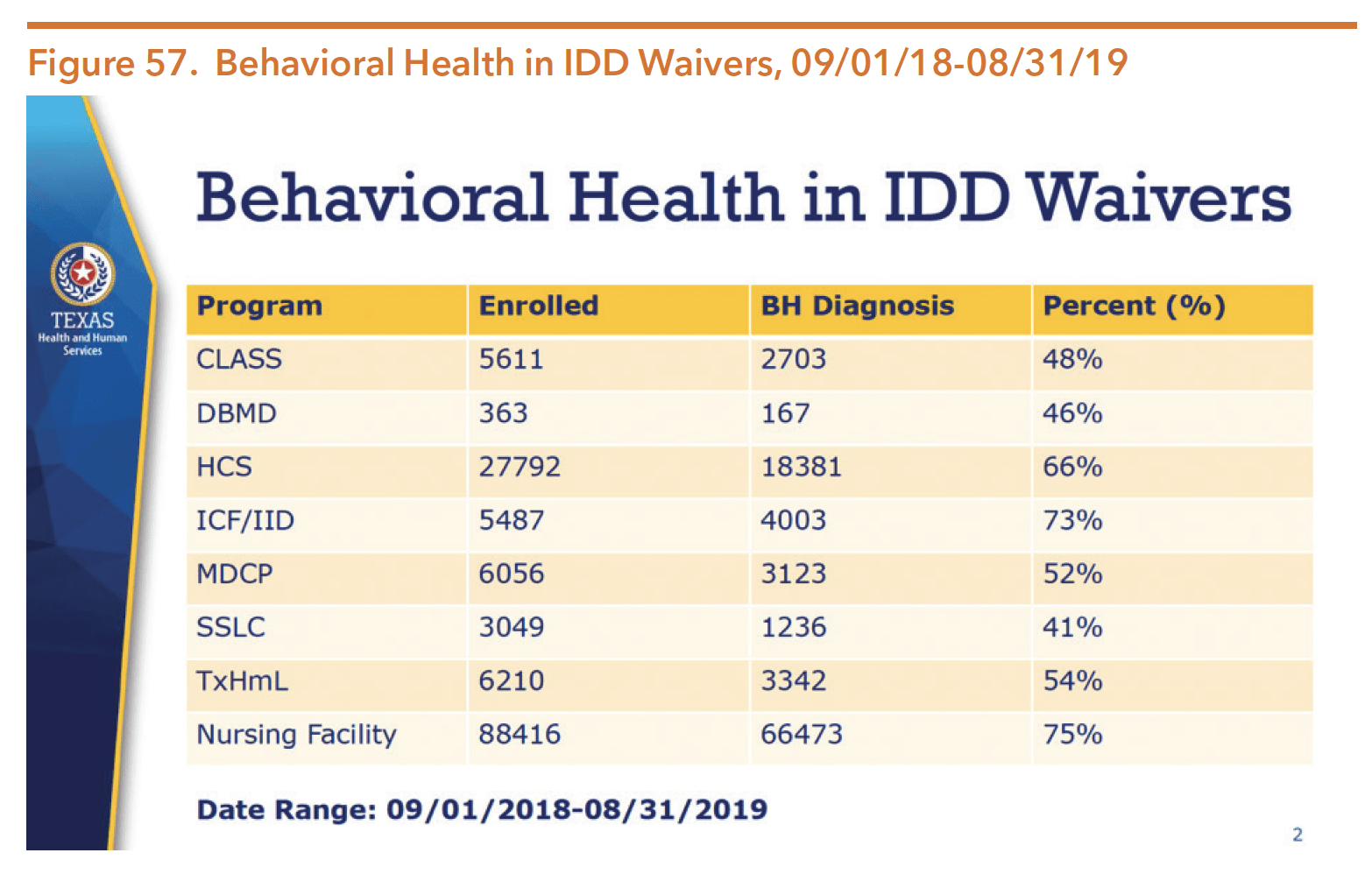
Source: Turner, H. (2020, October 9). Intellectual and developmental disabilities update to the Behavioral Health Advisory Committee. Texas Health and Human Services Commission.
Role of Local Intellectual and Developmental Disability Authorities in Connecting People to Waiver Services
There are 39 local intellectual and developmental disability authorities (LIDDAs) in Texas that cover all 254 counties to serve as the entry point for long-term services and support programs for people with IDDs, including those who also have co-occurring mental health conditions. While the LIDDAs may co-locate with LMHAs across the state, the two entities have separate administrative authorities. LIDDAs connect individuals with IDD to long-term services and supports, which include SSLCs, waiver programs, safety net services, and Community First Choice.
LIDDAs are responsible for program eligibility, waiver program enrollment, and determination of intellectual disability or a related condition as part of establishing the IDD priority population. Additional LIDDA responsibilities include developing service plans, providing targeted case management services, maintaining interest lists for IDD Medicaid waivers, conducting PASRR evaluations for persons with IDD seeking admission to a nursing facility, providing continuity of care, and completing Community Living Options Information Process (CLOIP) for persons residing in state supported living centers (SSLCs). LIDDAs are also responsible for permanency planning for individuals less than 22 years of age who live in intermediate care facilities, SSLCs, nursing facilities, and HCS group homes.
Health and Specialty Care System
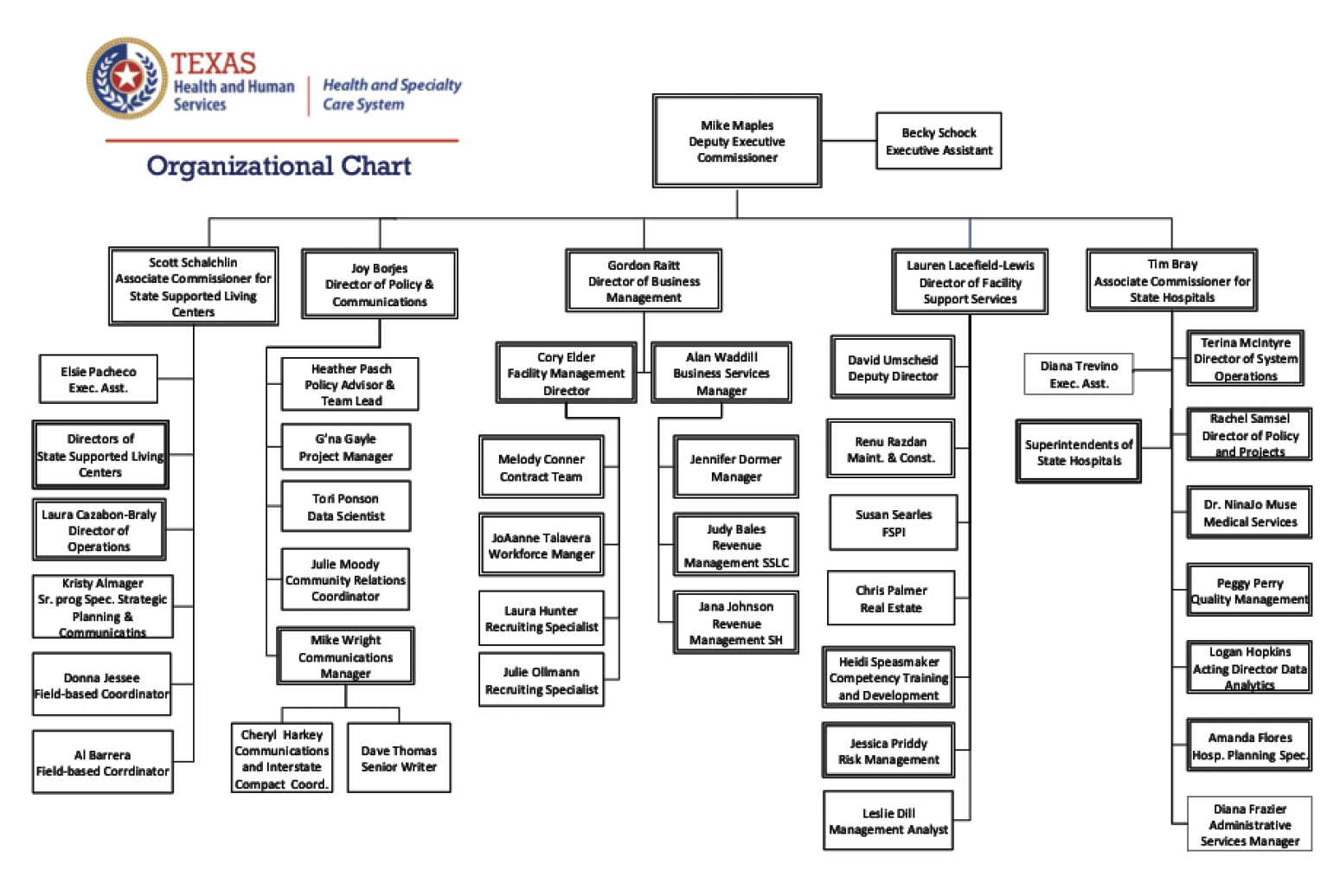
Source: Texas Health and Human Services Commission. (October 2020). Public Information Request, October 2020.
The Health and Specialty Care System, formerly known as the State Operated Facilities Division, is in charge of the state hospital system and state supported living centers (SSLCs). Both state hospitals and SSLCs serve as short or long-term inpatient or residential care options for people with serious mental illness or people with IDD.
INPATIENT SERVICES AND THE ADMISSIONS PROCESS
The state’s inpatient psychiatric services received priority attention during the 85th legislative session, generating significant interim activity. The momentum to improve and transform the state hospital system continued during the 86th legislative session. The 86th legislature partially funded $745 million for the construction and renovation for state hospitals, anticipating further funding during the FY 2022-23 biennium. For more information, see the State Hospital Redesign update in the Policy Environment section of this guide.
Inpatient mental health services are provided by state, community, and private hospitals to children, adolescents, and adults experiencing a psychiatric crisis due to mental illness. Inpatient hospitalization may be necessary for a period of time so that individuals can be closely monitored in order to:
- Provide accurate diagnosis and review of past diagnoses and treatment history;
- Adjust, stabilize, discontinue, or begin new medications;
- Provide intensive treatment during acute episodes during which a person’s mental health worsens; and/or,
- Assess or restore a person’s mental competency to stand trial.
As discussed earlier in this section, HHSC designates LMHAs/LBHAs as responsible for achieving continuity of care in meeting a person’s need for mental health services. Within this continuum of care, the state hospitals’ primary purpose is to stabilize people by providing inpatient mental health treatment. Each state hospital has a utilization management agreement with a partnering LMHA/LBHA that requires the LMHA/LBHA to screen all individuals seeking mental health services to determine if inpatient psychiatric services are required. If the screening and assessment determine that there is a need for inpatient psychiatric services, the LMHA/LBHA decides on the least restrictive treatment setting available, with the most restrictive setting of a state hospital considered the provider of last resort. When the LMHA has not screened and referred the individual for inpatient services, a hospital physician can determine if the person has an emergency psychiatric condition appropriate for admission to the state hospital.
Chapter 411 of the Texas Administrative Code defines inpatient mental health treatment as residential care provided in a hospital that includes medical services, nursing services, social services, therapeutic activities, and any other psychological services ordered by the treating physician. Specific services include:
- Diagnostic interviews;
- Structured therapeutic programming;
- Collaboration with appropriate courts and law enforcement;
- Suicide safety planning; and
- Discharge planning.
Currently, the Health and Human Services Commission manages three different waiting lists:
- Forensic – maximum security unit
- Forensic Clearinghouse – non-maximum security unit
- Civil – non-forensic adults, adolescents and children
There are two types of inpatient commitments in which individuals are provided comprehensive inpatient mental health services: civil and forensic.
During the 86th legislative session, SB 362 (Huffman/Price) was passed to address multiple issues related to civil, court-ordered mental health services. The bill:
- Reforms procedures relating to court-ordered outpatient and inpatient mental health services;
- Amends provisions relating to the early identification of a defendant suspected of having mental illness or an intellectual disability;
- “Adds a roadmap in the Code of Criminal Procedure for prosecutors and trial court judges” to release an individual with mental illness or IDD on bail after receiving an Article 16.22 report and transfer them to the appropriate court for court-ordered outpatient mental health services. The judge may only do this if the offense charged does not involve serious bodily injury.
- Allows the dismissal of the pending charges after the defendant complies with services requirement;
- Requires the Court of Criminal Appeals to ensure that judicial training related to court-ordered mental health services is provided at least once every year; and
- Requires an inpatient treatment facility administrator to assess the appropriateness of transferring the patient to outpatient mental health services not later than 30 days after the patient is committed to the facility, among other provisions.
Additionally, SB 362 amended the standard for outpatient commitment to a more provable standard. Previously, courts were required to find that an individuals’ mental health condition made it “impossible” for them to submit to voluntary outpatient treatment. Now, a court must find that the patient’s condition “significantly impairs” that ability.
Provisions relating to the early identification of a defendant suspected of having mental illness or an intellectual disability were also amended. The bill allows a trial court to release a defendant on bail and transfer the defendant to the appropriate court for court-ordered outpatient mental health services if the offense does not involve serious bodily injury. The bill also allows the dismissal of the underlying charges after the defendant complies with such treatment in certain circumstances.
CIVIL INPATIENT COMMITMENTS
Civil commitments to a state hospital can happen through a variety of entry points. Although voluntary admission is possible, the majority of civil patients are committed involuntarily. Generally, LMHAs screen referrals (from individuals and others in the community such as family members or law enforcement officials) to determine the best and least restrictive placement for services. If the LMHA does not screen the referral, the state hospital conducts an emergency psychiatric screening to determine whether admission is appropriate.
Voluntary admission is initiated by a request from a person at least 16 years old or a person responsible for a minor under age 18. The individual seeking admission must have “symptoms of mental illness” and would benefit from the services. If a person voluntarily admitted to a facility later requests discharge and the responsible physician believes the person meets the criteria for involuntary admission, the facility may file an application for emergency detention or court-ordered services.
Peace officers or the guardian of an adult can detain an individual involuntarily without a warrant and present them to the state hospital for screening. This process can also be initiated by other people who can file an application for a warrant with the county clerk or district attorney (DA) stating that the person is “mentally ill” and presents a substantial risk of serious harm to themselves or others that is imminent unless the person is immediately restrained. The application must have specific details supporting these statements. If the judge or magistrate reviewing the application finds that emergency detention is needed, the court will issue a mental health warrant and a peace officer will attempt to detain the individual and transport them to a facility. The individual must be examined by a physician within 12 hours (to provide a medical certificate for the court to determine if it should issue an order of protective custody) and can be detained for no more than 48 hours without a hearing on an order of protective custody.
An order of protective custody will be issued by the court if an examining physician states that the individual is a person with mental illness and presents a substantial risk of serious harm, or is experiencing substantial deterioration and cannot make a rational and informed decision to enter treatment, and cannot be at liberty while waiting for a judicial hearing on court-ordered services. Within 72 hours of detention under an order of protective custody, the court will hold a probable cause hearing for a more thorough review of the evidence supporting the order. The hearing for court-ordered inpatient services must occur within 14 days of the original filing. The hearing allows for testimony from the individual involved, medical experts, and other people in the individual’s life.
Court-ordered inpatient services may occur under an order for temporary commitment, not to exceed 45 days, or 90 days if the judge finds it necessary. After a jury trial or review by a judge, extended inpatient treatment must include a definitive time period not to exceed 12 months. Within that time period, a facility still must release a person if he or she no longer meets commitment criteria, even if the court mandated time period has not elapsed. Additionally, inpatient treatment facility administrators are required to assess the appropriateness of transferring the patient to outpatient mental health services no later than 30 days after the patient is committed to the facility.
FORENSIC COMMITMENTS
Justice-involved individuals needing forensic inpatient services are admitted to all the state hospitals. Individuals who require maximum security beds are admitted to either Rusk State Hospital or the Vernon Campus of North Texas State Hospital. Forensic commitments happen for two reasons:
- Individuals have been admitted to a hospital by judicial order because they have been determined incompetent to stand trial and are in need of competency restoration services so that they can better consult with legal counsel and understand the charges against them; or
- Individuals have been determined to be not guilty by reason of insanity and were ordered to a state hospital for a period of time not exceeding the maximum sentence length of the crime they committed.
Maximum vs. Non-Maximum Security Placements
Patients placed in maximum security commitments include individuals who are:
- Civilly committed and determined by professionals to be manifestly dangerous to self and/or others; or
- May have been charged with a violent felony offense involving an act, threat, or attempt of serious bodily injury.
As a result of SB 562 (86th, Zaffirini/Price), not all cases involving serious bodily injury, imminent threat of harm, or use of a deadly weapon are sent to a maximum security unit (MSU ). If an individual is charged with any of these offenses and in need of competency restoration, a court is required to enter an order committing the individuals to a facility designated by HHSC. MSUs are more expensive to operate than traditional state hospital units and a statewide shortage of MSU beds has contributed to the increasing waitlists for forensic beds in state hospitals. SB 562 streamlined the process of competency restoration so that individuals with mental illness who have been found incompetent to stand trial are less likely to wait in jail for long periods of time before receiving services. Additionally, SB 562 requires a determination of dangerousness prior to an individual being sent to an MSU after they have been found incompetent to stand trial.
Inpatient Care
FUNDING
The 86th Legislature appropriated over $890 million in all funds to operate the state hospital system for the 2020-21 biennium. An additional $270 million was appropriated for community hospital beds.
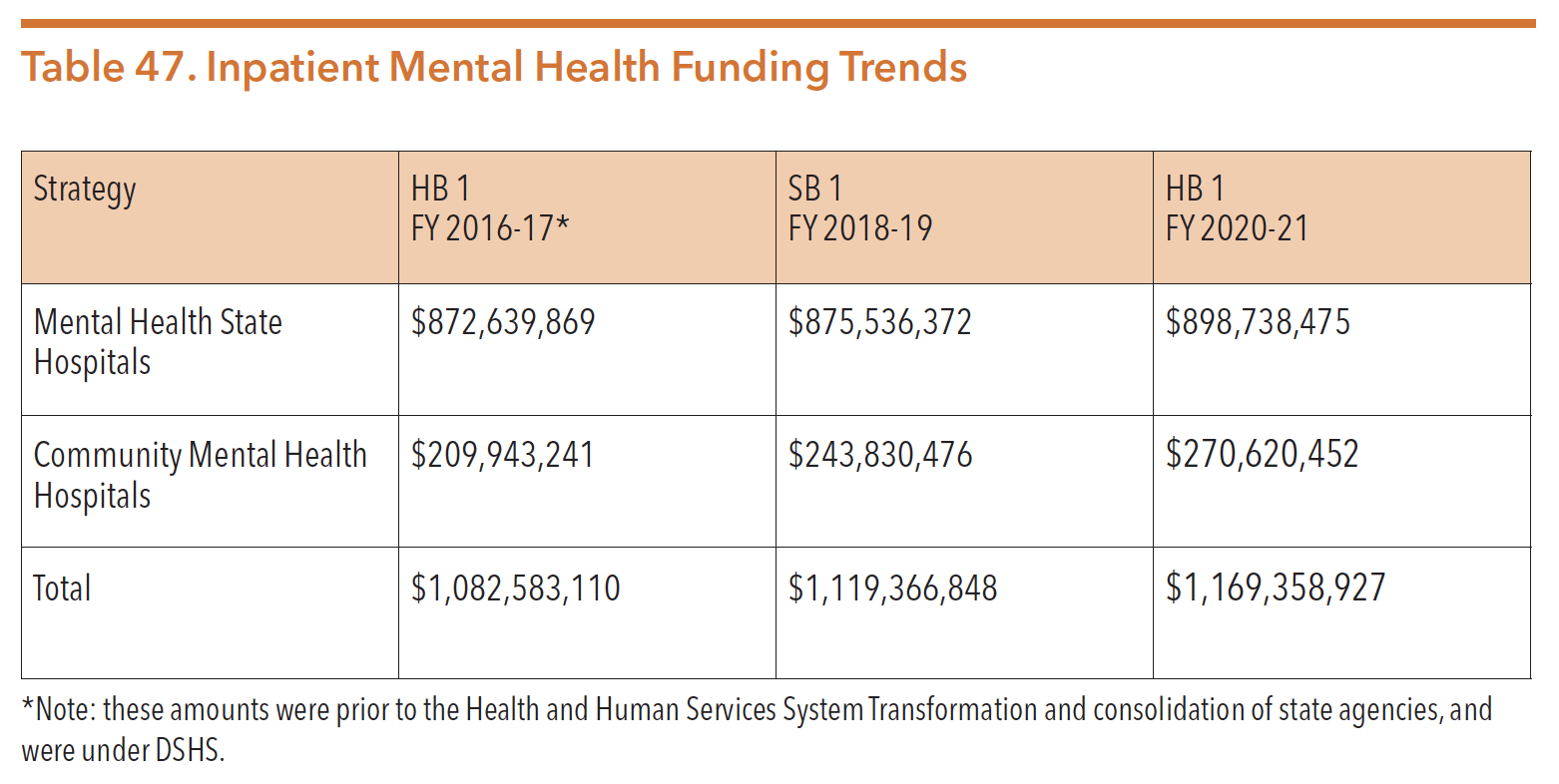
Sources: Texas Legislature Online (2019). H.B.1, General Appropriations Act, 86th Legislature, FY 2020-21. Retrieved from https://capitol.texas.gov/tlodocs/86R/billtext/pdf/HB00001F.pdf#navpanes=0
Texas Legislature Online (2017). S.B.1, General Appropriations Act, 85th Legislature, FY 2018-19. Retrieved from https://capitol.texas.gov/tlodocs/85R/billtext/pdf/SB00001F.pdf#navpanes=0
Texas Legislature Online (2015). H.B.1, General Appropriations Act, 84th Legislature, FY 2016-17. Retrieved from https://capitol.texas.gov/tlodocs/84R/billtext/pdf/HB00001F.pdf#navpanes=0
Legislative Appropriations Request, FY 2020-21. Retrieved from http://www.lbb.state.tx.us/Agency_Docs.aspx
STATE HOSPITALS
The State Hospital Services Department provides oversight of the ten state mental health hospitals and one psychiatric residential treatment facility for youth (the Waco Center for Youth) displayed in Figure 58. Each LMHA receives an allocation of state hospital resources to coordinate inpatient mental health services for residents of their specific state hospital service area.
Hospitals in Austin, Big Spring, El Paso, Rusk, San Antonio, Terrell, Wichita Falls and the Rio Grande Center in Harlingen provide services to both civil and forensic patients. The Vernon Campus of the North Texas State Hospital offers inpatient psychiatric services to both adults and adolescents needing a maximum-security facility, and the Kerrville State Hospital provides adult forensic inpatient services. The state also operates the Waco Center for Youth as an adolescent residential treatment facility.
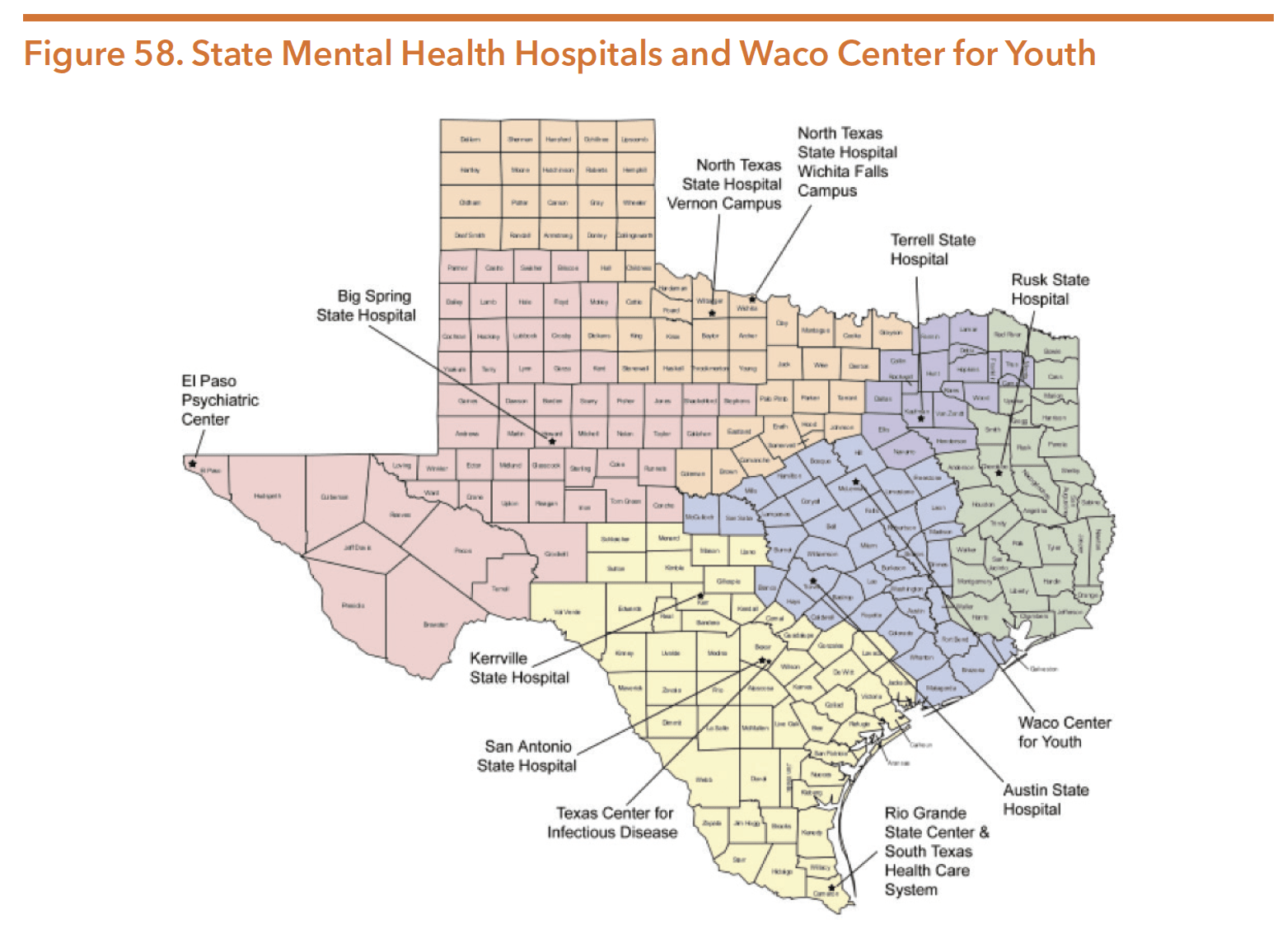
Source: Texas Department of State Health Services. (2016). Presentation to Select Committee on Mental Health: The Behavioral Health System [PowerPoint slides]. Retrieved from http://www.legis.state.tx.us/tlodocs/84R/handouts/C3822016021810001/5fc9614b-41a4-436e-9eba-67b14f00ad22.PDF
Capacity
As of September 30, 2020, there were a total of 2,263 state hospital beds in Texas. Table 48 shows the total number of beds at each of the state-operated psychiatric hospital facilities as of September 2020. These numbers do not include the community and private hospital beds in facilities that contract with HHSC. In FY 2020, the state hospital network is increasing its capacity by 5.5 percent (390 patients).
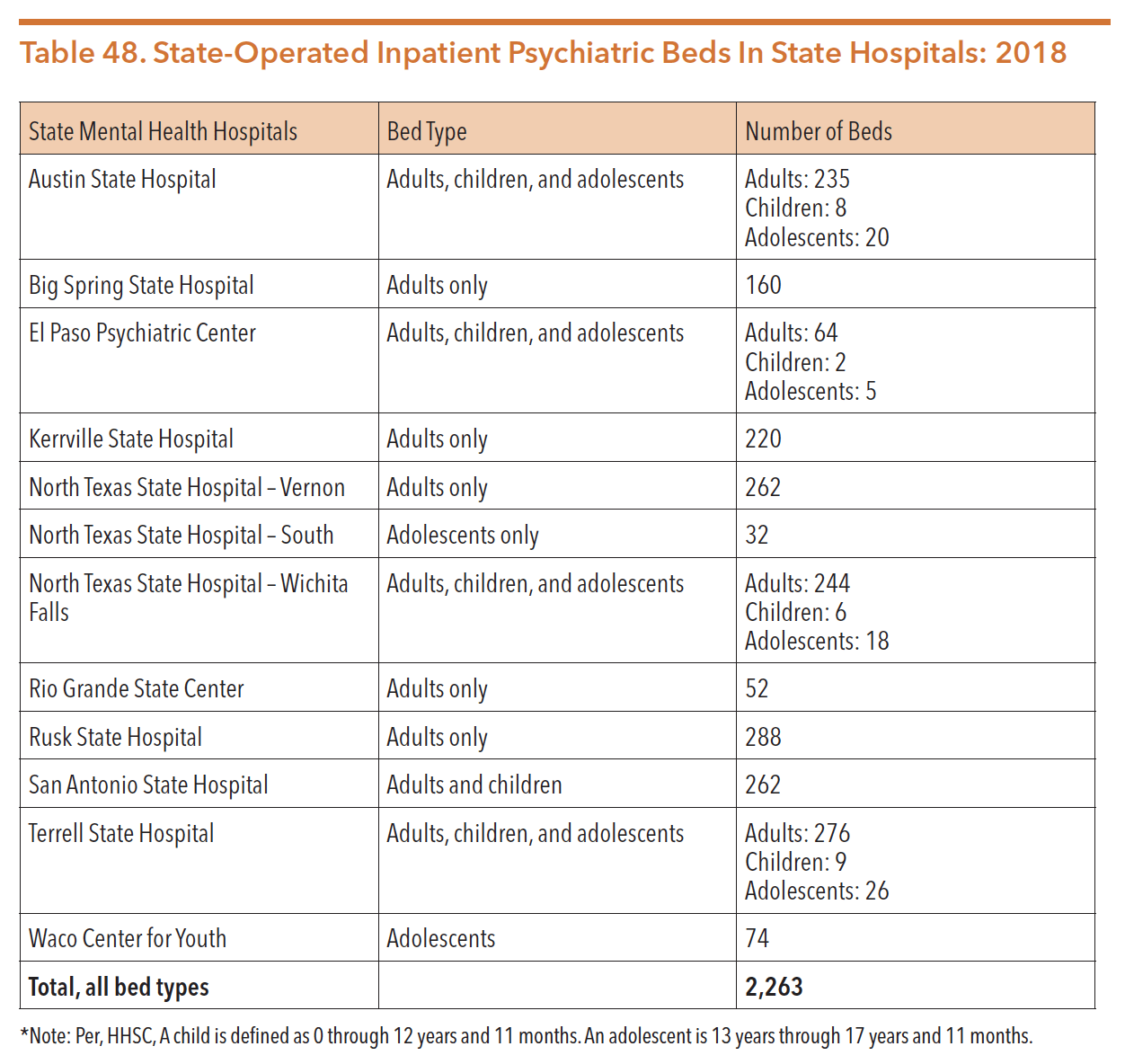
Source: Texas Health and Human Services Commission. Data request. Received from Rachel Samsel, October 1, 2020
Staffing and Functional Capacity of State Hospitals
It is important to note that a hospital’s functional capacity is typically lower than their total bed count when determining the number of psychiatric inpatient beds in state hospitals. Functional capacity is impacted for a number of reasons, including: high staff turnover, poor building designs, aging infrastructure, and increased resources and supervision needed for patients with complex medical and/or behavioral problems. As of September 2020, the state-operated hospital system as a whole had a functional capacity as follows:
Average daily census for FY 20 – 1,992
Number of beds available for children and adolescents – 200
Total number of maximum-security beds – 302
Staff turnover in state hospitals has been an issue across all positions; state hospitals have had particular difficulty with staffing shortages in skilled nursing positions. On top of the already-stressful work environment of state hospitals, salary caps for nurses working in state hospitals make it difficult for nurses to earn as much as they would in the private sector. The shortage of skilled nurses has a disproportionate impact on individuals with complex needs and individuals in maximum-security units because they require higher staff-to-client ratios and more frequent interventions to remain safe and healthy. Many available units and inpatient beds cannot be utilized for treatment because they do not have the proper staff skill sets and required staffing ratios in place. In FY 2017, general turnover was 36.34 percent, but specific positions, such as direct care workers, experienced even higher rates in part due to low wages. According to HHSC, some direct care workers are paid less than $13/hour. Psychiatric nursing assistants at the state hospitals have an annual turnover rate of 32.7 percent, with 43.8 percent of the entry level positions turning over annually.
HHSC was directed by the 86th Legislature to improve culture, recruitment, and retention efforts. HHSC was allotted additional funding for reducing turnover and vacancy rates at state hospitals and SSLCs by increasing direct care pay rates for targeted positions. Additionally, Rider 108 directs HHSC to evaluate compensation levels, turnover and vacancy rates and patterns, use of contractors and position type, and recruiting efforts at the state hospitals and SSLCs. Using the collected data, HHSC is required to develop recommendations to reduce turnover and vacancy rates, and submit a report to the LBB and the Governor’s Office by August 31, 2020.
Forensic Shift
In the last decade, the state hospital population shifted from mostly civil patients to a majority forensic patient population. In FY 2006, civil patients were 62.3 percent of the state hospital population. As of August 2019, only approximately 35 percent of all state hospitals patients were there through civil commitments. See Figure 59 below.
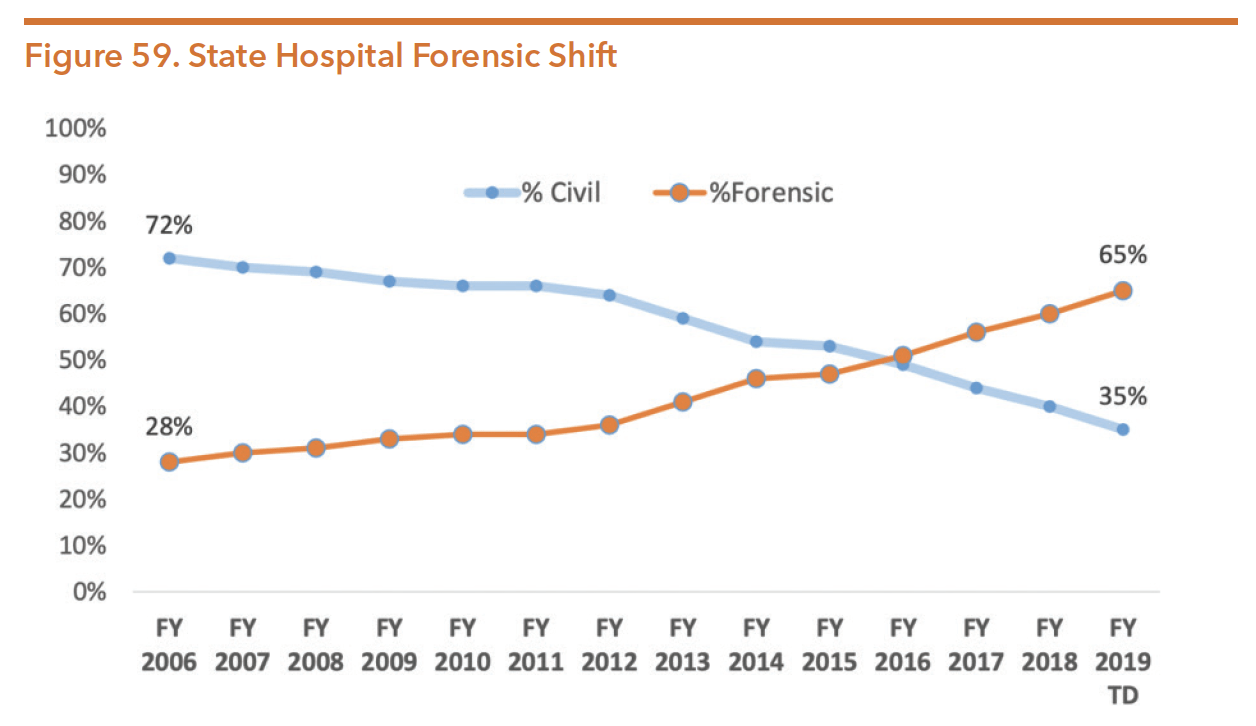
Source: Texas Health and Human Services, Statewide Behavioral Health Coordinating Council. (February 2019). Texas statewide behavioral health, fiscal years 2017-2021: Strategic plan update and the foundation for the IDD strategic plan. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2019/hb1-statewide-behv-hlth-idd-plan-feb-2019.pdf
The impact of a growing forensic population lead to less available capacity for all patients, increased waiting lists, and a changing focus for hospital staff. Waitlists for forensic beds increased steadily between FY 2006 and FY 2019. In December of 2018, there were 731 individuals on the wait list. By April 2020, the waitlist for all forensic beds had increased to 900, with 449 individuals on the waitlist for maximum security beds. Figure 60 outlines the forensic waitlist information for Texas state hospitals during the first two quarters of 2020.
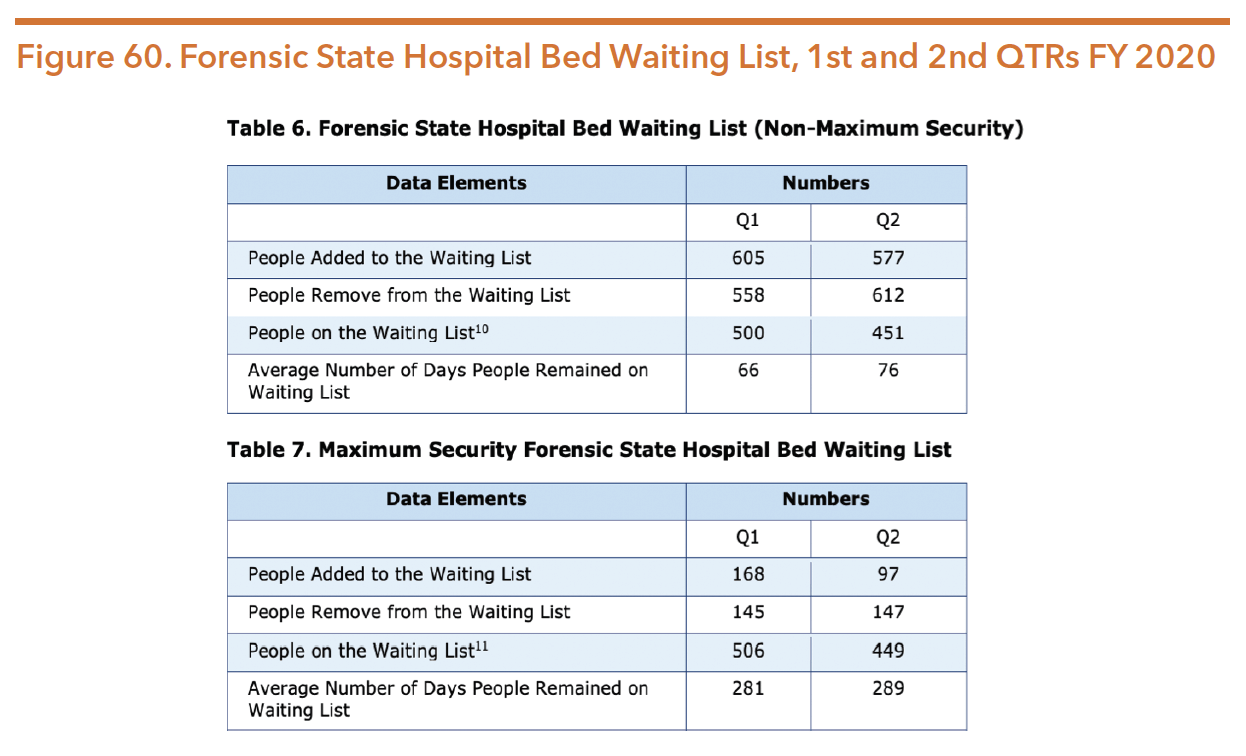
Source: Texas Health and Human Services Commission. (2020). Semi-annual reporting of waiting lists for mental health services. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/hb1-semi-annual-waiting-lists-mhs-april-2020.pdf
The shift to a majority of the state hospital beds serving forensic patients with longer lengths of stay compared to civil patients compounds the waiting list dilemma. Shown in Figure 61, forensic patients found incompetent to stand trial have an average length of almost 200 days which is significantly longer than the average of 80 days for civil patients. As patients stay in the hospital longer, there is less bed availability for new admissions. Almost 40 percent of individuals within the state hospital remain for one year or more shown in Figure 62.

Source: Maples, M., & Gaines, S. (Oct. 2019). Texas Health and Human Services presentation to the Joint Commission on Forensic Services. Retrieved from https://hhs.texas.gov/sites/default/files/documents/about-hhs/communications-events/meetings-events/jcafs/oct-2019-jcafs-agenda-item-4.pdf
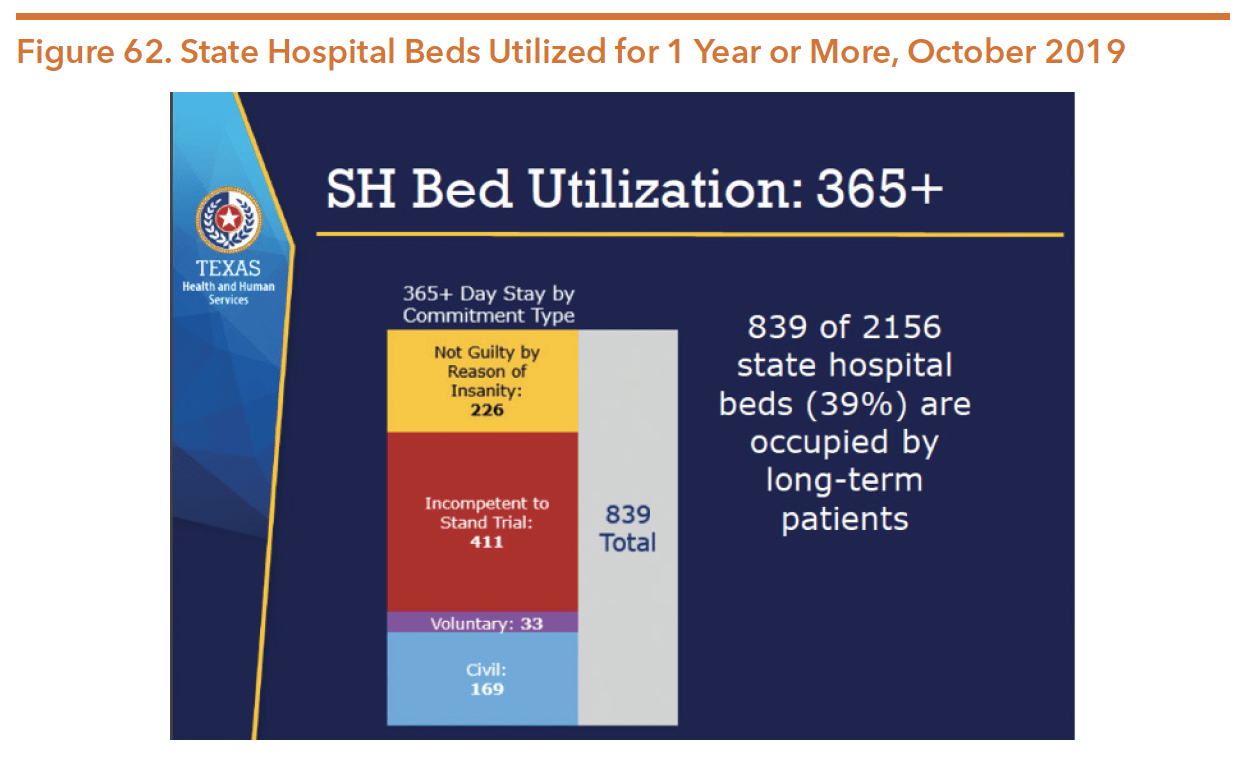
Source: Maples, M., & Gaines, S. (Oct. 2019). Texas Health and Human Services presentation to the Joint Commission on Forensic Services. Retrieved from https://hhs.texas.gov/sites/default/files/documents/about-hhs/communications-events/meetings-events/jcafs/oct-2019-jcafs-agenda-item-4.pdf
The shift to a larger forensic population and the longer lengths of stay in state-operated facilities has resulted in significant reductions in admissions. See Figure 63 below:
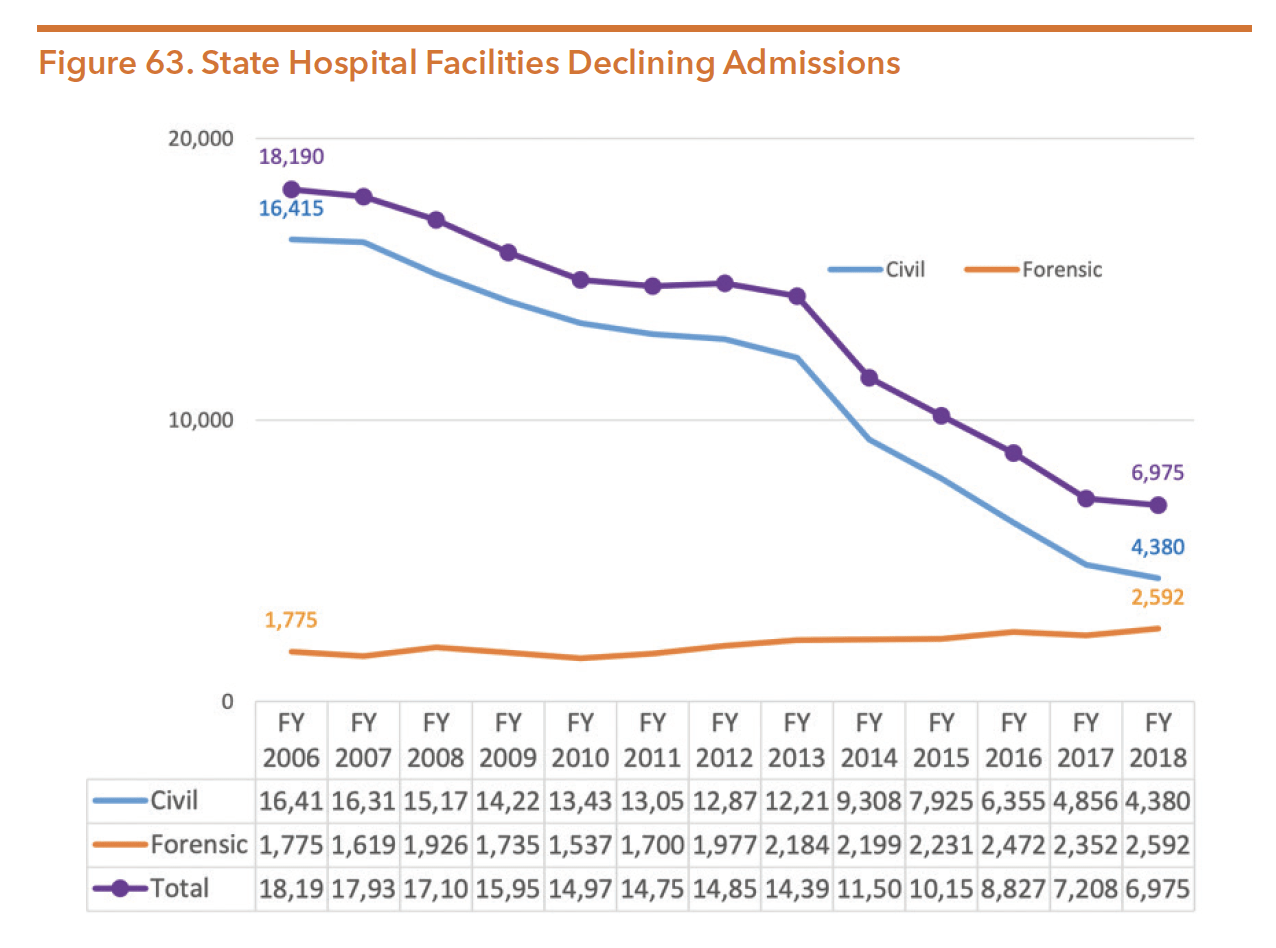
Source: Texas Health and Human Services, Statewide Behavioral Health Coordinating Council. (February 2019). Texas statewide behavioral health, fiscal years 2017-2021: Strategic plan update and the foundation for the IDD strategic plan. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2019/hb1-statewide-behv-hlth-idd-plan-feb-2019.pdf
State Hospitals Utilization and Costs
Despite a shortage of inpatient psychiatric beds, the average daily censuses of all hospitals are below their total funded capacities. This is partly because hospitals must retain some open bed capacity in case of emergencies, but also because staffing shortages and high turnover have made it difficult for many hospitals to utilize the total number of beds they have.
Whether due to an individual’s especially intensive mental health needs or their lack of access to community-based treatments and services, many individuals have trouble remaining in the community after discharging from a state hospital. Since inpatient hospitals serve as a safety net for many individuals who receive inadequate or no community-based treatment, the availability and quality of community-based services has a direct impact on inpatient hospital capacity.
Improvements to Aging State Hospital Infrastructure
In June 2016 Dr. David Lakey, the Chief Medical Officer for the UT Health System, identified the following key challenges present in the Texas mental health hospital system:
- Lack of facility capacity
- Hospitals are poorly designed for modern healthcare
- Current condition of hospitals
- Cost of replacing hospitals
- Increasing medical complexity of patients
- Lack of integration between physical and mental health
- Lack of strong partnerships with academia
- Rural facilities are frequently the sole “industry” of the local community
- Recruiting and retaining staff
- Increasing outside medical care costs
- Role in disproportionate share hospital funding
- Current mental health hospital system is underfunded.
The 85th legislature appropriated $300 million to HHS for the construction or significant repair of the state hospitals. In August 2017, HHS submitted a comprehensive plan for state hospital system transformation to the governor and the legislature, including a request to expend funds. On December 18, 2017, the Legislative Budget Board and the governor approved the use of $47.7 million for various projects. HHS started the projects in spring 2018. Phase I projects include: Rusk State Hospital, Kerrville State Hospital, Continuum of Care Campus in Houston, Austin State Hospital, and the San Antonio State Hospital. More information is available in the Policy Environment section of this Guide.
The 86th Texas Legislature took significant steps to address the infrastructure needs of the state hospital system. The following amounts were appropriated in SB 500 (86th, Nelson/Zerwas), the supplemental appropriations bill:
$165,000,000 – Begin construction of a new Austin State Hospital
$190,300,000 – Begin construction of a new San Antonio State Hospital
$ 90,054,363 – Construct replacement unit at Rusk State Hospital
Additional information on the state hospital redesign efforts are included in the Funding Section of this guide.
COMPETENCY RESTORATION SERVICES
A person charged with a crime who is found incompetent to stand trial (i.e., unable to competently understand court proceedings) must be restored to competency before the legal process can continue. In order to be considered competent to stand trial, that person must be able to consult with his or her defense lawyer and have a rational and factual understanding of the legal proceedings. Individuals determined to be incompetent, typically due to mental illness or an intellectual disability, may be placed into inpatient competency restoration programs, jail-based competency restoration programs, or outpatient competency restoration programs. Placement into these specialty programs is determined by a mixture of factors, including an individual’s clinical complexity, criminal history, and the safety risk they pose to the community and to other individuals placed in their program.
SB 562 (86th, Zaffirini/Price) intends to improve the competency restoration process by streamlining the process to reduce backlog for individuals who have been found incompetent to stand trial who are waiting in jail for services. The bill also required determination of dangerousness for an individual who has been found incompetent to stand trial upfront before a being sent to a maximum security unit (MSU).
Inpatient Competency Restoration
Individuals found incompetent to stand trial may be committed to a state hospital forensic unit to receive treatment in effort to restore their competency to stand trial. Before 2004, inpatient competency restoration was the only option for individuals found incompetent to stand trial. Recently there has been a steady and significant increase in the percentage of forensic commitments for inpatient competency restoration services. Because those commitments have a much longer average length of stay within state hospitals than civil or voluntary commitments, the average daily census for forensic patients has now surpassed that of civil patients. Individuals who are forensically committed to state hospitals have longer lengths of stay, averaging 199 days for forensic patients versus 80 days for civil patients.
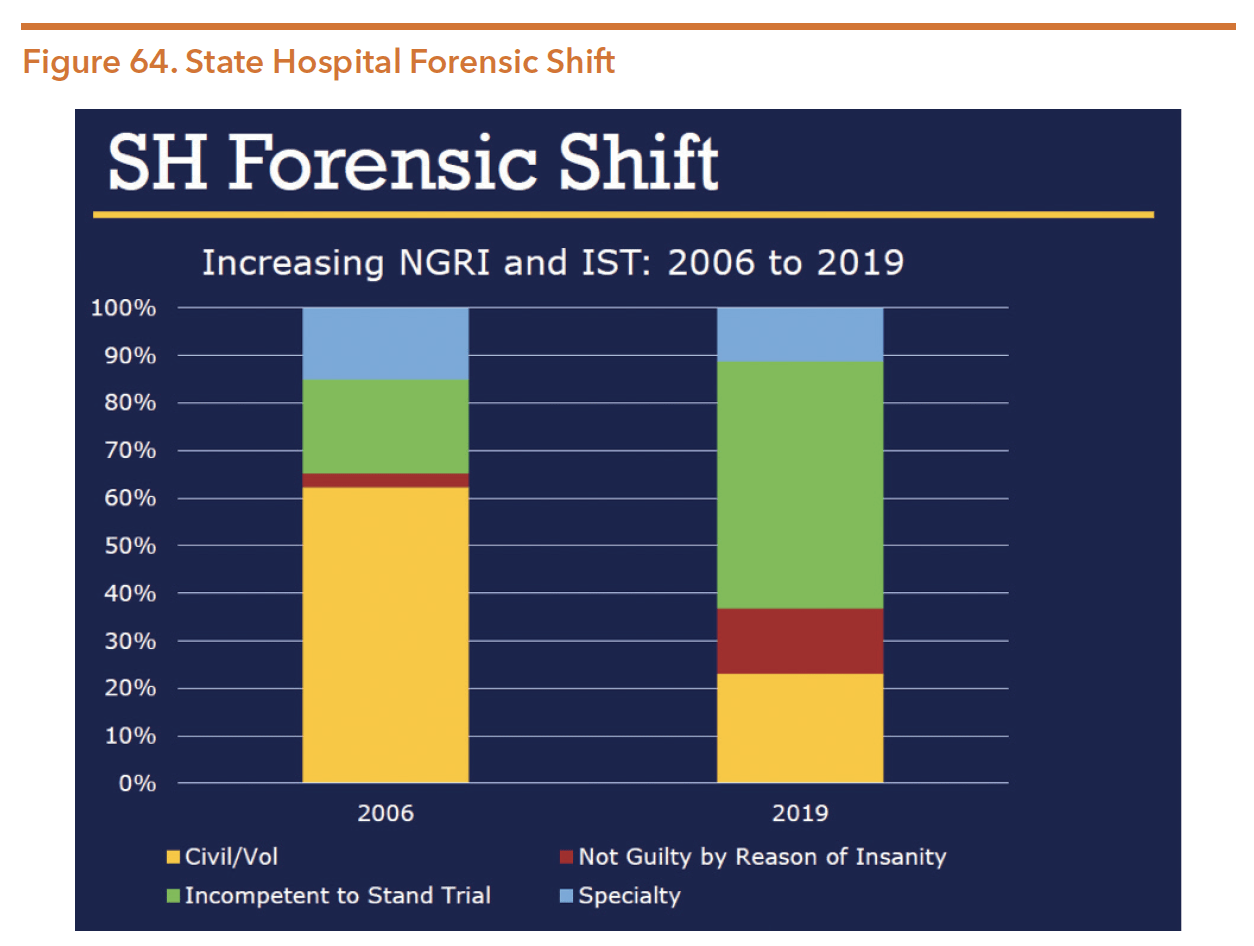
Source: Maples, M., & Gaines, S. (2019). Texas Health and Human Services presentation to the Joint Commission on Forensic Services. Retrieved from https://hhs.texas.gov/sites/default/files/documents/about-hhs/communications-events/meetings-events/jcafs/oct-2019-jcafs-agenda-item-4.pdf
Jail-Based Competency Restoration
SB 1475 (83rd, Duncan/Zerwas) created a jail-based competency restoration (JBCR) pilot program for individuals who otherwise would be committed to a mental health facility or residential care facility for inpatient competency restoration services.
In 2017, the HHSC JBCR pilot program report stated that the program experienced delays in implementation due to a “lack of strong interest in the procurement opportunity and a competitive pool; however, rules governing the provision of JBCR services were adopted in January 2016”. In 2019, SB 1326 (85th, Zaffirini/Price) passed to address a multitude of areas related to individuals with mental illness or IDD who are involved with the criminal justice system, including provisions to the JBCR program. More details on SB 1326 can be found in the Hogg Foundation 85th legislative Session summary: https://hogg.utexas.edu/wp-content/uploads/2017/08/UPDATED-Legislative-Summary_2017.pdf
Outpatient Competency Restoration
Outpatient competency restoration (OCR) is a process of providing community-based competency restoration services, including mental health and substance use treatment services and legal education training for individuals found incompetent to stand trial. The goal of OCR is to give individuals the resources and services they need to maintain a level of psychiatric stability and be able to understand the legal process so that they can proceed through the court system while remaining in the community. OCR programs can allow low-risk individuals with mental illness to avoid prolonged stays in jails or state hospitals, which are costly to local taxpayers and often have the result of exacerbating individuals’ mental illness.
The Texas Code of Criminal Procedures began allowing referrals to OCR programs in 2003. In 2007, the Code of Criminal Procedure 46B was amended to permit outpatient treatment. Texas initiated four outpatient competency restoration pilot programs in response to the growing number of forensic commitments in state psychiatric hospitals and was allocated $4 million each year to support expanding the number of OCR pilot sites. As of November 2019, there were 12 operating OCR sites.
Current Texas OCR sites include:
- Integral Care (Austin)
- Center for Health Care Services (San Antonio)
- MHMR Tarrant County (Fort Worth)
- Value Options-NorthSTAR (Dallas)-now North Texas Behavioral Health Authority
- Tri-County Behavioral Healthcare (Conroe)
- Behavioral Health Center Nueces County (Corpus Christi)
- Emergence Health Network (El Paso)
- Community Healthcore (Longview) StarCare Specialty Health System (Lubbock)
- Andrews Center Behavioral Healthcare System (Tyler)
- Heart of Texas Region MHMR Center (Waco)
- Central Counties Services (Belton)
Between 2010 and 2019, 1,723 individuals had been served in an OCR site for an average length of 176 days. Outcomes of OCR show that the majority of individuals either restored competency or have ultimately had their charges dismissed. HHSC’s outcome data is depicted in Figure 65.
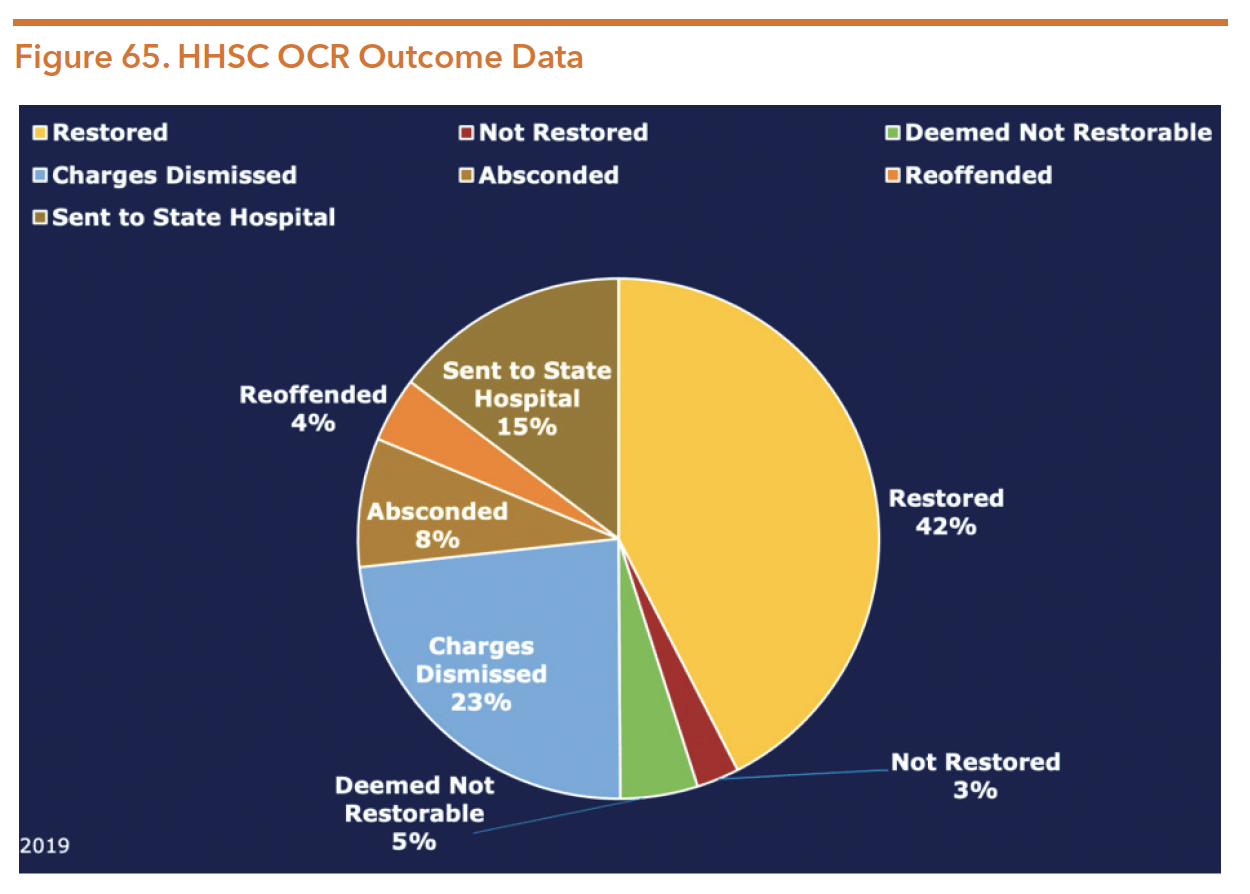
Source: Swan, L. and Pierre-Carr,L. (November 2019). Texas competency restoration: Outpatient and jail-based. Texas Health and Human Services presentation to the Judicial Summit on Mental Health. Retrieved from http://texasjcmh.gov/media/1751/ocr-and-jail-based-cr-combined-pp.pdf
In addition to avoiding the high cost of hospitalization, OCR can reduce overall costs to local communities and jails. Cost-savings are demonstrated through reducing the length of time individuals remain in jail and eliminating the cost of lengthy transportation to an available hospital bed. In 2015, the Hogg Foundation for Mental Health, in collaboration with the Department State Health Services, conducted an of OCR programs. The report found:
- A person’s likelihood of restoration increased with greater lengths of stay in an OCR program, up to a 21-week threshold;
- After the 21-week mark, longer lengths of stay were not associated with greater likelihood of restoration;
- Prior hospitalizations were shown to have a significant effect on a person’s likelihood to be restored to competency in an OCR program; and
- Individuals in OCR programs who had zero or one prior psychiatric hospitalizations were more likely to be successfully restored to competency than individuals who had two or three or more prior hospitalizations.
Figure 66 below shows some of the most important components of successful OCR programs.
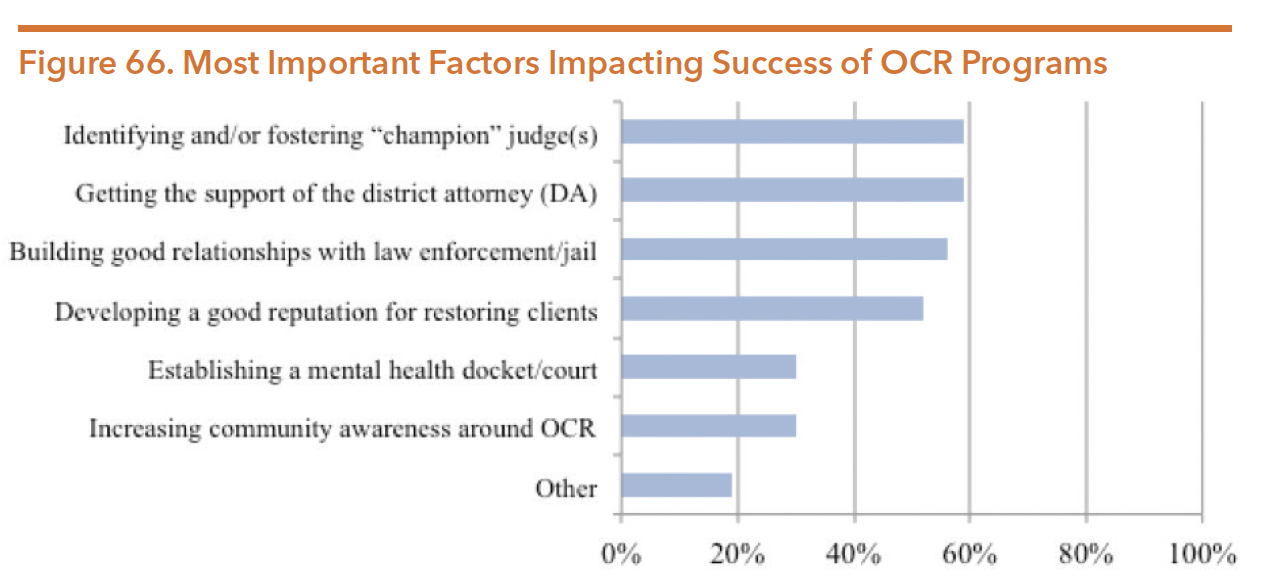
Source: Graziani, C., Guzmán, M.R., Mahometa, M, & Shafer, A. (July 2015). Texas outpatient competency restoration programs: Evaluation report. The Hogg Foundation for Mental Health and Department and State Health Services. Retrieved from http://www.tidc.texas.gov/media/57883/texas-outpatient-competency-restoration-programs-evaluation.pdf
More recent research on OCR programs across the country concluded that OCR programs have “promising outcomes in terms of high restoration rates, low program failure rates, and substantial cost savings.” OCR program evaluations in multiple states have shown a number of benefits to OCR, including:
- An average rate of 70 percent competency restoration (77 percent in Texas);
- An average of 149 days to be restored to competency (70 days in Texas); and
- Total cost of OCR averaged $215 per individual per day ($140 in Texas).
Between July 2018 and August 2019, a group of stakeholders met to develop standards and rules for governing the provision of OCR services in the Texas Administration Code. Workgroup members included judges, prosecutors and defense attorneys, OCR providers, policy and advocacy groups, as well as HHSC staff. OCR rules were drafted for:
- Eligibility and ineligibility criteria for admission
- Recommendation regarding OCR program admission
- General service requirements
- Assessment, reassessment, and court reporting
- Preparation for discharge
- Outcomes
- Written policies and procedures
- Staff member training
- Rights
- Compliance with statutes and rules
INSTITUTIONAL LONG-TERM SERVICES AND SUPPORTS
Persons with disabilities residing in institutional providers of long-term services and supports (LTSS) services, including skilled nursing facilities, privately operated intermediate care facilities, or large state-operated supported living centers (SSLCs), often experience co-occurring behavioral health conditions. Funding for these residential services is provided primarily through Medicaid. SSLCs are administered through the Health and Specialty Care System Division HHSC.
Table 49 presents information on the eligibility requirements and services provided by institutional providers of LTSS services.
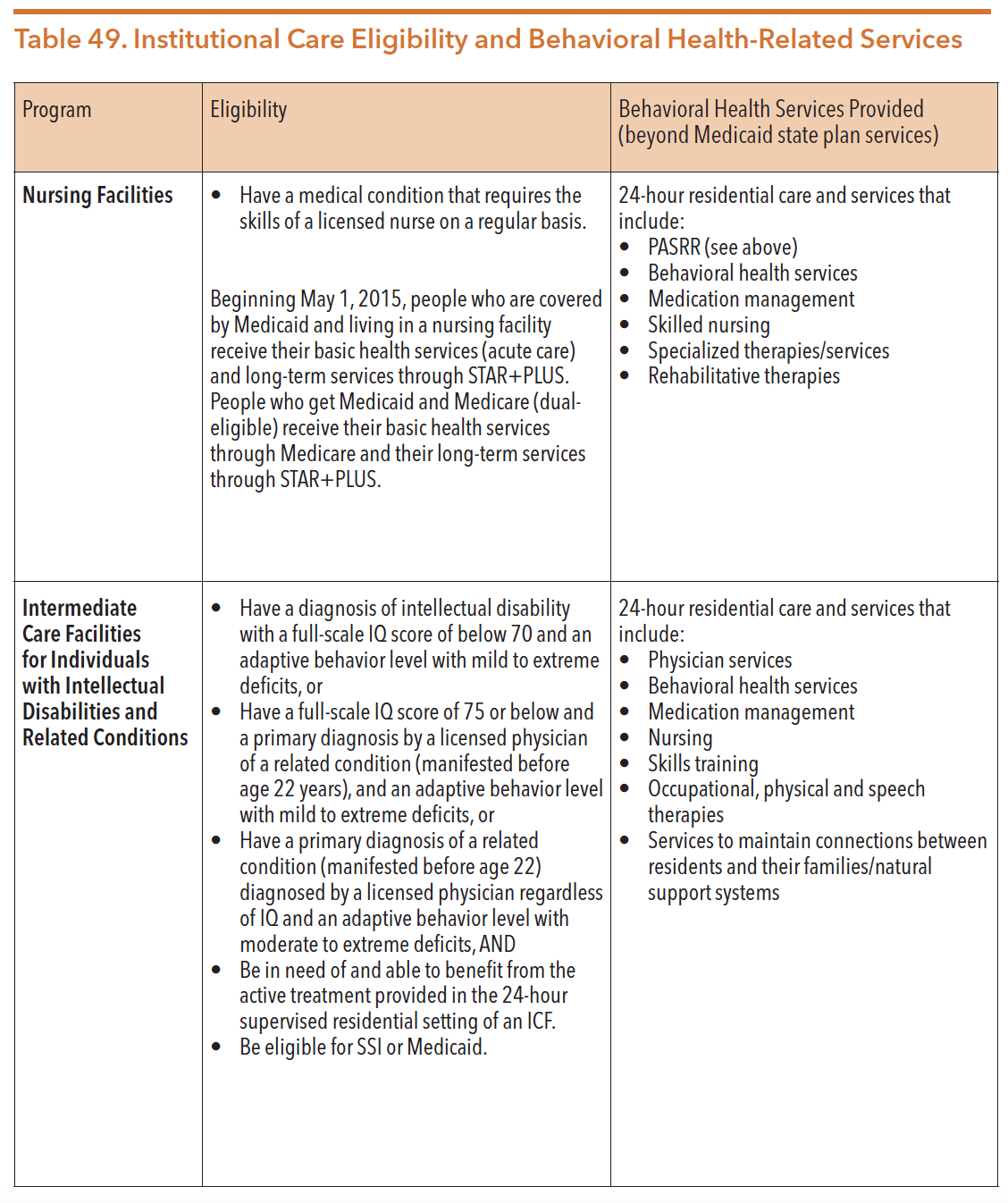
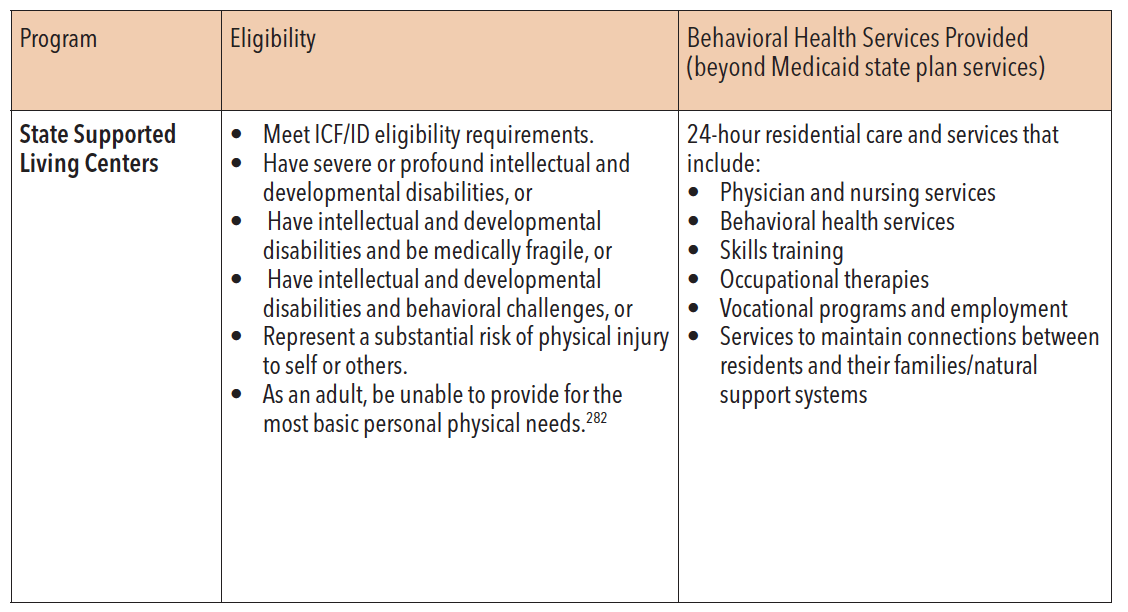
Source: Texas Department of Aging and Disability Services. (2015). Reference Guide 2015. Retrieved from http://dadscfo.dads.state.tx.us/ReferenceGuide/guides/FY15ReferenceGuide%28revised%29.pdf
Skilled Nursing Facilities
Texas nursing facilities provide institutional care for older Texans and people with disabilities whose medical condition requires skilled licensed nursing services. As of March 2020, there were 1,208 licensed nursing facilities in Texas. While Medicaid nursing facilities require medical necessity for admission, many individuals residing in nursing facilities also have co-occurring mental health conditions. In March 2015, nursing facility services were integrated into STAR+Plus, a Texas Medicaid managed care program that provides both acute care and long-term services and supports. Nursing facilities provide room and board, social services, medical supplies and equipment, over-the-counter drugs, and personal needs items. Skilled behavioral health services are provided by psychiatrists and other medical and behavioral health professionals.
In order to ensure that the mental health needs of nursing home residents are identified and addressed, the federal government mandates Preadmission Screening and Resident Review (PASRR) Level 1 screening prior to admission to a nursing facility. PASRR screening is intended to identify the following:
- Individuals who have a mental illness, an intellectual disability, or other developmental disability (also known as related conditions);
- The appropriateness of placement in the nursing facility; and
- Eligibility for specialized services.
In 2013, CMS directed Texas to make changes to the PASRR program. The three major changes included:
- Eliminating the role of nursing facilities in the PASRR evaluation determination process by introducing local authorities as the party that will complete the PASSR evaluation;
- Requiring specific, specialized services to be identified before nursing facility admission; and
- Requiring an automated communication to local authorities that is triggered when a Resident Review is required.
In February 2020, CMS announced its revision of the PASRR regulations. From February-April 2020, CMS accepted comment on the proposed rule changes. According to CMS, this proposed rule would “modernize the requirements for PASRR, currently referred to in regulation as Preadmission Screening and Annual Resident Review, by incorporating statutory changes, reflecting updates to diagnostic criteria for mental illness and intellectual disability, reducing duplicative requirements and other administrative burdens on State PASRR programs, and making the process more streamlined and person-centered.” Proposed changes include updating mental illness and ID definition, streamlining the screening process, allowing the use of telehealth, and emphasizing individual preference related to long-term services.
Community Intermediate Care Facilities (ICF)
The federal government gives states the option to include intermediate care facility (ICF) services in their Medicaid state plans. However, once a state chooses to include ICF services as a Medicaid benefit, those services become an entitlement to all individuals who meet eligibility criteria. Community-based ICFs can be licensed to provide residential and habilitation services to people with intellectual disabilities or other developmental disabilities, or related conditions. As of September 2020, there were 784 licensed ICFs in Texas, 70 are state owned/managed and 714 are privately owned. These facilities provide residential services similar to the SSLCs but can be privately owned and operated. Community ICF facilities vary in size from six beds to over 160 beds; most community-based ICFs are small, with eight or fewer beds.
State Supported Living Centers (SSLCs)
State supported living centers (SSLCs) are large institutions that provide 24-hour residential services for people with intellectual and developmental disabilities (IDD). Individuals seeking placement in an SSLC must meet both financial and functional eligibility requirements. Behavioral health treatment is a required service that must be provided by the facilities, as some residents have both a mental health condition in addition to an IDD. The SSLCs are licensed and certified ICFs owned and operated by the state. Approximately 58 percent of the SSLC operating funds come from the federal government, and 42 percent from state revenue and third-party revenue resources. SSLCs operate in 13 locations: Abilene, Austin, Brenham, Corpus Christi, Denton, El Paso, Lubbock, Lufkin, Mexia, Richmond, Rio Grande, San Angelo, and San Antonio. Abilene, Brenham, and Lufkin serve adult and children residents, while all other campuses serve only residents who are 18 years of age or older.
As of August 2019, 185 SSLC residents were alleged criminal offenders. Although many SSLCs serve a small number, 77 percent of alleged offenders reside at Mexia SSLC which has been designated by the legislature to provide forensic services, and 10 percent of alleged offenders reside at San Angelo State Supported Living Center.291 In FY 2019, over 2,900 individuals resided in these facilities. Approximately 62 percent of individuals served were diagnosed with a severe or profound intellectual disability, 69 percent were diagnosed with a behavioral health need, and over half (56 percent) had a co-occurring intellectual disability and mental health condition. The majority of residents have lived in an SSLC for more than a decade, with 58 percent residing in an SSLC for more than 15 years. Since FY 2015, individuals’ average length of stay has remained at almost 24 years.
Although the SSLC population has declined significantly over the past decade, any discussion related to closure or consolidation of facilities has been met with strong legislative opposition. There was significant debate around SSLCs during the 84th legislative session due to the DADS Sunset Recommendations to close six centers, including closing the Austin SSLC by September of 2017. The legislature ultimately voted to keep the Austin SSLC and all other SSLCs operational. In Texas, only the legislature can direct closure of an SSLC. In the 85th legislative session, Senator Hinojosa introduced a bill, SB 602, which would have required a commission to review each SSLC. The legislation would have given the commission authority to recommend which SSLCs should be consolidated or closed. The bill did not pass during the 85th legislative session. During the 86th legislative session, SB 1552 (Lucio/Hinojosa) was filed but failed to pass. The bill addressed recent Office of the Independent Ombudsman for SSLCs reports that have highlighted the lack of local and statewide training requirements for staff at these centers, as well as the benefits of specialized training for staff in supporting the needs of center residents. Additionally, SB 1552 would have required the executive commissioner of HHSC to develop processes and procedures required for SSLC staff to follow, and to develop specialized training for such staff.
Due to fixed costs and continued deterioration of aging facilities, the per person costs increased despite the overall census decline. According to a 2015 Sunset Commission final report, maintaining the large system of state-run facilities is costly, involving more than thousands of employees and a budget of $661.9 million a year.296 An HHSC report in 2018 revealed that delivering services in 2017 to a person in an SSLC cost an average $26,767 per month. The report also shows that SSLCs in Texas employ 11,496 people or full-time equivalents. Further, maintaining the SSLCs’ dilapidated infrastructure contributes to significant state costs.299 The 85th legislature appropriated approximately $80 million to help address infrastructure improvements and maintenance needs for SSLCs.
Figure 67 below shows the SSLC enrollment trend from FY10- FY19
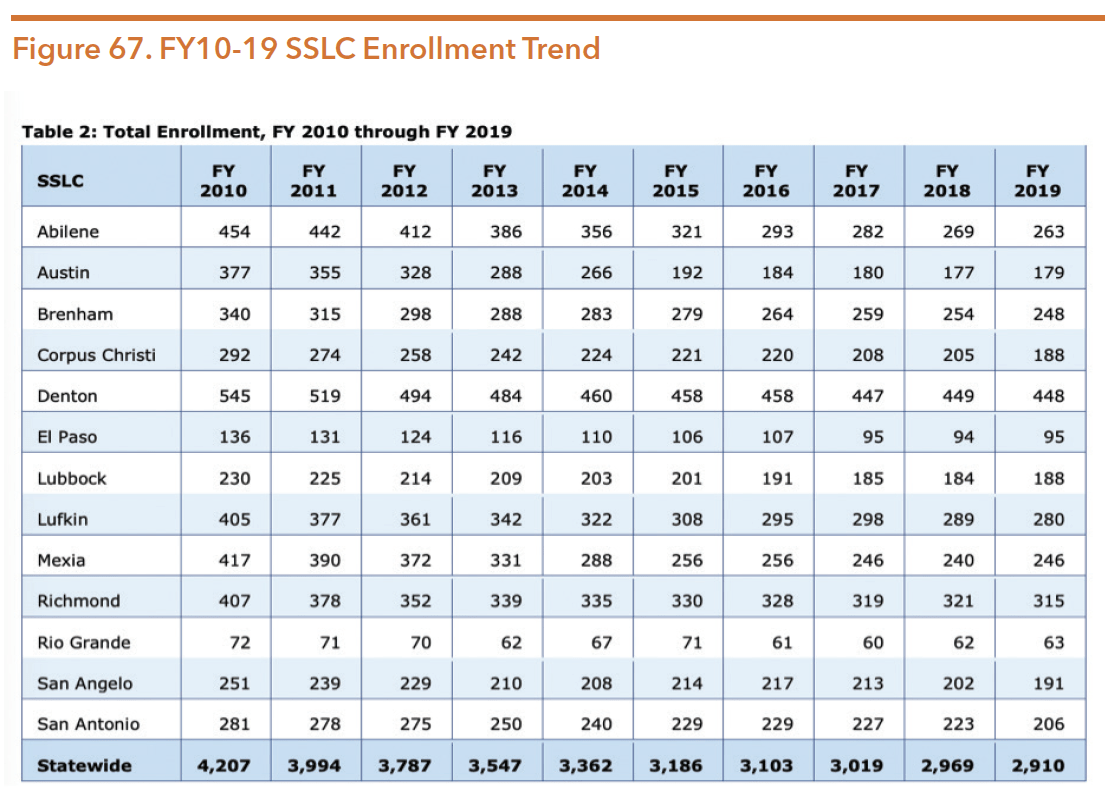
Source: Texas Health and Human Services Commission. (July 2020). Reimagining the future: A report on maximizing resources and long-term planning for state supported living centers. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/maximizing-resources-long-range-planning-sslc-july-2020.pdf?fbclid=IwAR2ca08kPGvWggsWw6-ZAfRP3nR-88pjEYcnyf8O9EzApjUCyDM6UUoIepA
As part of a 2009 settlement agreement with the U.S. Department of Justice over conditions at SSLCs, the state agreed to improve health, safety, and quality of care for residents. The agreement included increased access to psychiatric care and psychological services, as well as improved policies and practices to reduce the use of restraints. DADS was required by the 83rd legislature to submit a plan to achieve targeted improvements in services and supports for residents. Since the submission of this plan, DADS was abolished and all functions, including the operation of the SSLCs, were transferred to HHSC. Independent monitors were assigned in mid-2014 to visit and report on conditions at all 13 SSLCs.301 Despite the 2009 agreement, the November 2019 monitoring report for the Austin SSLC continued to identify deficiencies. Other monitoring reports in 2019 identified deficiencies at the SSLCs related to psychiatric and psychological services, including individual residents not progressing toward psychiatric goals and not maintaining psychiatric stability. However, reports indicated that when an individual was not making progress toward psychiatric goals revisions to treatment were made. Updated reports for all 13 SSLCs were released in 2019 as the centers continue to be evaluated by independent monitors every nine months.
HHSC implemented a new initiative in FY 2019 to help SSLCs increase compliance with the settlement agreement. Every year, members of the state office Quality Review Team (QRT) visit each center for three days to:
- Validate SSLC monitoring data;
- Identify best practices to share with other centers; and
- Provide feedback and technical assistance.
During the 86th legislature, Rider 110 was included in Article II of the 2020-21 state budget, directing HHSC to create Reimagining the Future: A Report on Maximizing Resources and Long-Range Planning for State Supported Living Centers. According to HHSC, “its purpose is to promote the development of a comprehensive, statewide approach toward long-range planning for SSLCs and maximize resources to support the continuum of care for people with IDD.” According to the report, transitions from SSLCs back to the community have decreased by 65 percent in the last ten years. Figure 68 and Figure 69 show the top obstacles to transition and referral. In partnership with stakeholder engagement, HHSC conducted an analysis of the overall strengths and opportunities for improvement. The report developed a list of objectives to accomplish:
- Enhance resident services and supports to support individualized care for people served by an SSLC;
- Strengthen employee services and supports to provide guidance in business practices that improve recruitment and retention of staff at SSLCs and compliment the agency’s values to create a workplace culture that is innovative, skilled, and diverse; and
- Expand community-based services and supports to align with the agency’s vision and mission and long-term objectives that promote independence and positive outcomes for people with IDD.
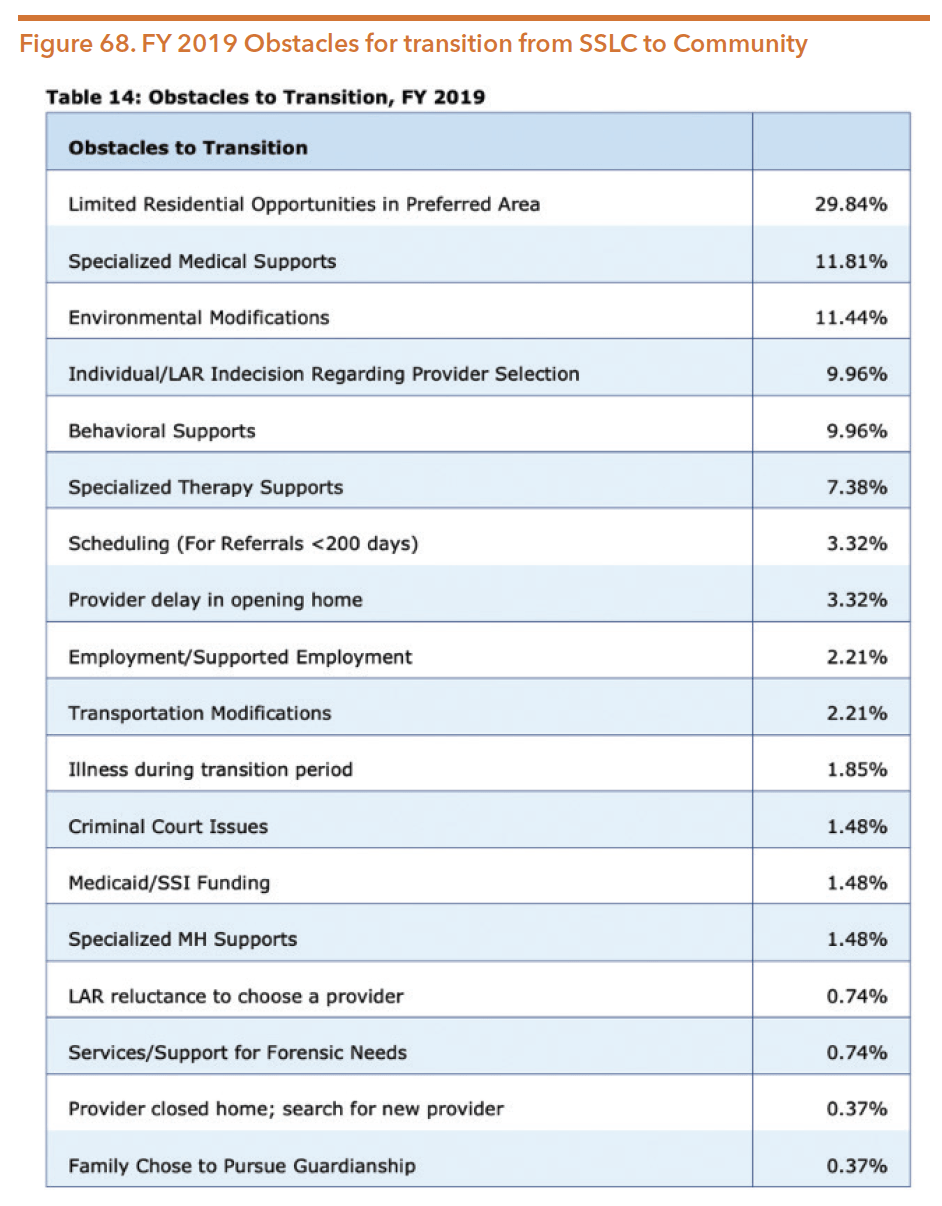
Source: Texas Health and Human Services Commission. (July 2020). Reimagining the future: A report on maximizing resources and long-term planning for state supported living centers. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/maximizing-resources-long-range-planning-sslc-july-2020.pdf?fbclid=IwAR2ca08kPGvWggsWw6-ZAfRP3nR-88pjEYcnyf8O9EzApjUCyDM6UUoIepA
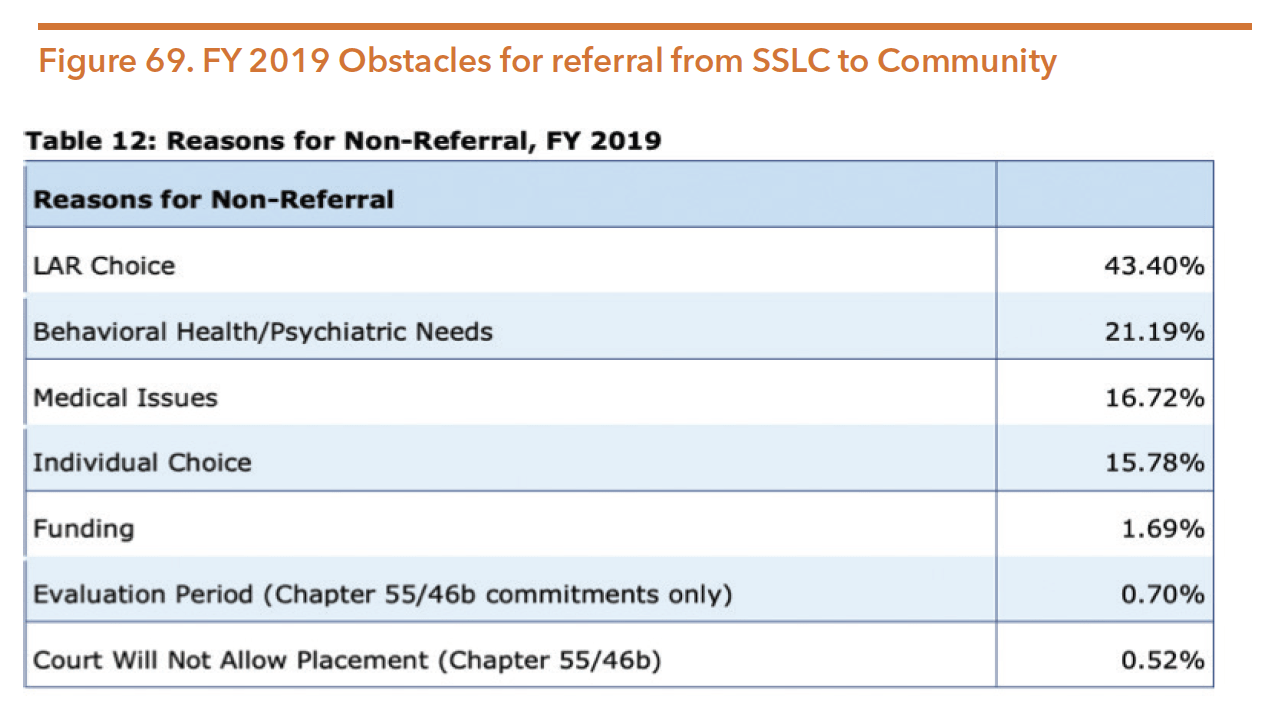
Note: “LAR” refers to legally authorized representative
Source: Texas Health and Human Services Commission. (July 2020). Reimagining the future: A report on maximizing resources and long-term planning for state supported living centers. Retrieved from https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2020/maximizing-resources-long-range-planning-sslc-july-2020.pdf?fbclid=IwAR2ca08kPGvWggsWw6-ZAfRP3nR-88pjEYcnyf8O9EzApjUCyDM6UUoIepA
INSTITUTIONS FOR MENTAL DISEASES EXCLUSION
The Institutions for Mental Diseases (IMD) exclusion in Section 1905(a)(B) of the Social Security Act defines an IMD as “a hospital, nursing facility, or other institution with more than 16 beds, that is primarily engaged in providing diagnosis, treatment, or care of persons with mental diseases, including medical attention, nursing care, and related services.” Until 2016, the Social Security Act excluded funding inpatient services for individuals between 21 and 64 years of age in IMDs. Since Medicaid was enacted in 1965, the intention of the IMD exclusion policy was to promote community services expansion and ensure the federal government did not have to assume financial responsibility for inpatient psychiatric care. The federal restriction on funding for inpatient hospital services resulted in state general revenue as the primary source of funds for state hospital services for adults between ages 22 and 64. Additionally, efforts to improve or expand public inpatient services are funded almost entirely by the state without federal matching.
On May 6, 2016, Medicaid managed care coverage rules regarding the IMD exclusion were entered into the Federal Register. The new rules permitted “Federal Financial Participation (FFP) for a full monthly capitation payment on behalf of an enrollee aged 21 to 64 who is a patient in an IMD,” so long as the individual elects to receive services in a public or private IMD and the IMD in question provides psychiatric inpatient care, substance use condition inpatient care, or behavioral health crisis residential services. Federal Financial Participation also only applies to short-term IMD stays of less than 15 days in one month, but stays can exceed the 15-day limit if the days are spread out over two months (e.g., 10 days at the end of July and 10 days at the beginning of August). Before this rule change, stand-alone psychiatric facilities could not deny admission to individuals referred to them. However, they also did not receive federal Medicaid match payments, creating the risk of lower quality care and premature discharge. The objective of the rule change was to mitigate the IMD exclusion and address shortages in short-term inpatient behavioral health treatment by providing more flexible financing options.
In recent years, the federal government has provided new mechanisms for states to finance IMD services for individuals between 21 and 64 years of age through Medicaid in certain situations. There are now four options for states to cover these services: Section 1115 demonstration waivers, managed care “in lieu of” authority, disproportionate share hospital payments, and the SUPPORT Act state plan option.
Section 1115 Demonstration Waivers
In November 2017, states were able to apply for an 1115 waiver to receive FFP for the continuum of services for substance use conditions, including services provided to Medicaid enrollees residing in residential treatment facilities typically ineligible due to the IMD exclusion. As part of this initiative, states need to indicate how inpatient and residential care will supplement and coordinate with community-based care in a robust continuum of care in the state. CMS guidance encourages states to maintain their current funding levels for a continuum of services, without reducing or diverting state spending on mental health and substance use treatment services as a result of available federal funding for services in IMDs. bAs of September 2020, 28 states had approved 1115 waivers, with an additional eight pending, to receive federal Medicaid dollars for SUD services in IMDs. As of September 2020, Texas was not one of the states with approved or pending waivers.
In November 2018, CMS issued guidance regarding opportunities to design innovative systems for adults with SMI and children with SED, allowing states to provide Medicaid coverage through Section 1115 waivers for short-term stays in IMDs as mandated by the 21st Century Cures Act. The waiver would require a statewide average length of state of 30 days, be budget neutral, and a commitment to continued funding of outpatient community-based mental health services. The goals of the waiver are to reduce individuals’ utilization and length of stay in emergency departments while waiting to receive services in a specialized setting, reduction of preventable admissions to acute care, improved crisis stabilization services, improved accessibility to community-based services, and improved care coordination and continuity of care. As of March 2020, four states had approved 1115 waivers, with an additional three pending, to receive federal Medicaid dollars for mental health services in IMDs. In February 2020, HHSC began assessing options and fiscal impacts of an SMI/SED 1115 waiver and expressed consideration of funding for the waiver through the exceptional item process.
Health, Developmental, and Independence Services
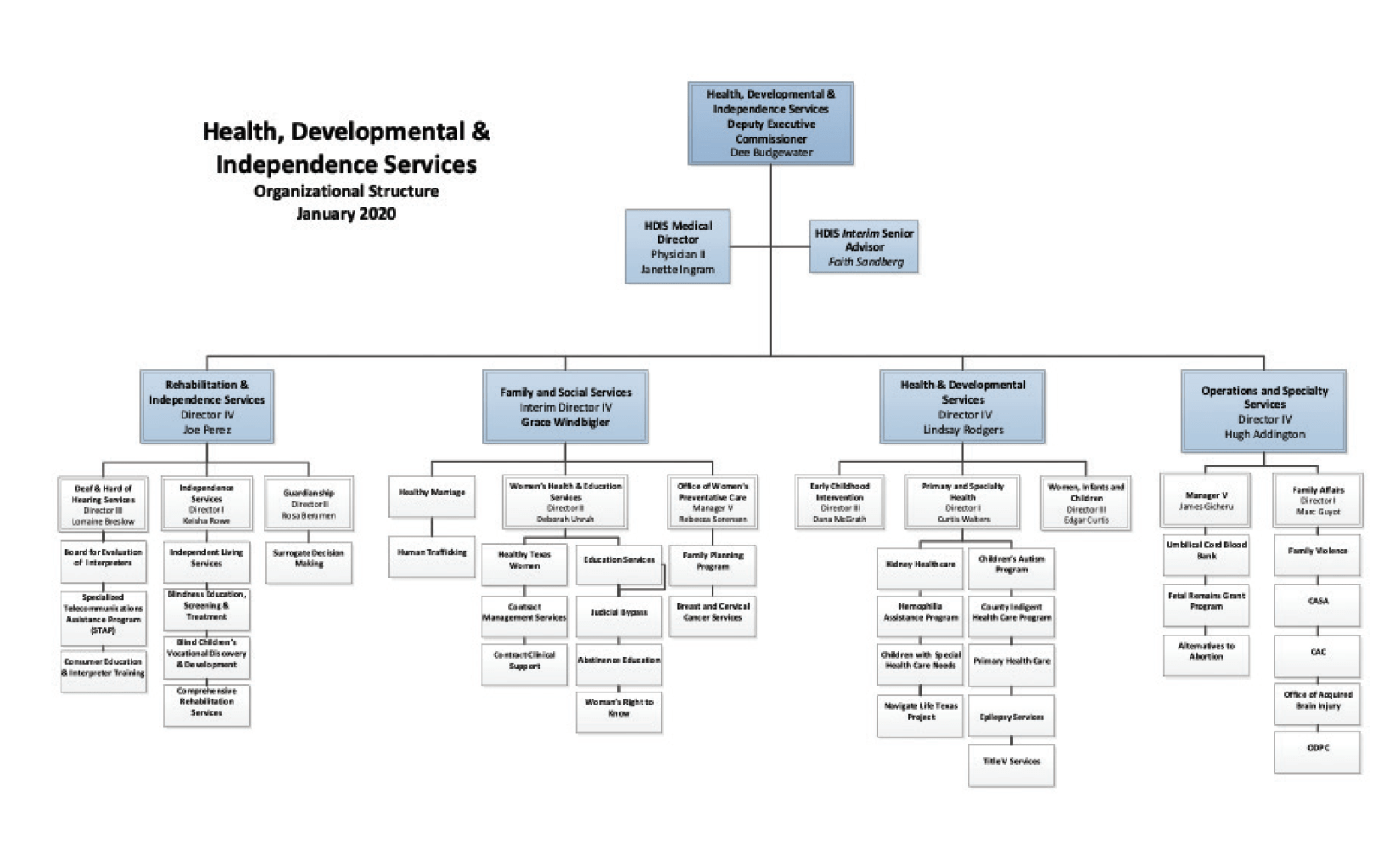
Source: Texas Health and Human Services Commission. (January 2020). Public Information Request, January 2020.
This division’s units include:
- Office of Disability Prevention for Children
- Rehabilitative & Social Services
- Health & Developmental Services
OFFICE OF DISABILITY PREVENTION FOR CHILDREN
The Office of Disability Prevention for Children (ODPC) was created after Governor Greg Abbott vetoed a bill that would have moved the Texas Office of Prevention of Developmental Disabilities (TOPDD) to the University of Texas. Since the legislation was vetoed and TOPDD was eliminated, the Office of Disability Prevention for Children (ODPC) was created within HHSC.
ODPC focuses on the prevention of certain disabilities in children from birth through 12 years of age. While certain disabilities may be prevented, it is important to note that some individuals cannot “prevent” their disability but are able to learn life skills and coping strategies to live a meaningful life within the community. ODPC has identified five focus areas to address through provider and public education, promotion of public policy, working with state agencies and stakeholders, development of long-term plans, and evaluating state efforts. These areas of focus include:
- Preventing disabilities caused by prenatal alcohol or substance exposure
- Preventing disabilities caused by maternal health issues during pregnancy
- Preventing acquired brain injury in children
- Early identification and diagnosis of disabilities to ensure early intervention and services
- Promoting mental health and wellness for children with an intellectual or developmental disability:
One of the initial projects of this office was to facilitate trainings using The Road to Recovery: Supporting Children with Intellectual Disabilities Who have Experience Trauma developed by the National Child Traumatic Stress Network and the Hogg Foundation for Mental Health.
REHABILITATIVE AND SOCIAL SERVICES UNIT
The Rehabilitative and Social Services Unit includes programs and services transferred from Department of Assistive and Rehabilitative Services (DARS) to HHSC. The programs in this unit that offer services to individuals living with mental health conditions include:
- Independent Living Services Programs
- Comprehensive Rehabilitation Services
- Guardianship
INDEPENDENT LIVING SERVICES PROGRAM
There are 30 independent living centers in Texas. As of August 2016, all independent living services were outsourced to and provided by centers for independent living (CILs) located across the state. A list of centers is available at http://www.ilru.org/ projects/cil-net/cil-center-and-association-directory-results/TX. The Independent Living Services Program is intended to promote self-sufficiency for individuals with a disability that results in substantial barriers in ability to live independently, including mental health and substance use conditions. Services within the Independent Living Program seek to provide the individual with “consumer control, peer support, self-help, self-determination, equal access and self-advocacy.”
The Independent Living Services Program partners with Centers for Independent Living (CILs) located around the state. These CILs are private, nonprofit, nonresidential centers that provide an array of independent living services. CILs partner with HHSC and community-based organizations and are funded either privately or with state and federal funds.
Eligibility
In order to be eligible for independent living services, an individual must be certified to the person’s ability to function independently in the family or community. There must also be a reasonable expectation that assistance will result in the person’s ability to function more independently.
Independent living core services include:
- Information and referrals
- Independent Living skills training
- Counseling
- Advocacy
- Transition services
Additional services available from CILs that have contracted with HHSC to provide may include:
- Counseling
- Orientation and mobility
- Recreation and socialization
- Rehabilitation technologies
- Examinations
COMPREHENSIVE REHABILITATION SERVICES
The Comprehensive Rehabilitation Services program serves people 15 years and older who have experienced traumatic brain injuries and/or traumatic spinal cord injuries. The program is intended to ensure that consumers who have traumatic brain injuries (TBIs) and/or spinal cord injuries (SCIs) receive individualized services to improve their functioning within their homes and communities to promote independence.
The following are basic statistics available relating to the CRS program for FY 2019:
- Number of individuals serviced –740
- Number of new applications received – 401
- Number of successful case closures – 116
- Average monthly cost per individual –$2,686
- Traumatic Brain Injury – 379 individuals
- Spinal Cord Injury – 333 individuals
- Both TBI and SCI – 28
GUARDIANSHIP PROGRAM
The Guardianship Services program provides guardianship services to youth aging out of conservatorship referred by DFPS as having a continued need for a guardian, or by a court under limited circumstances as described in the Estate Code. The court appointment of guardianship over an individual is intended to provide protection for adults whom the courts deem incapacitated. Often guardianship is appropriate and works as intended, ensuring guardians effectively manage the affairs of older adults and people with disabilities fairly, honestly, and appropriately. Guardianship profoundly limits a person’s decision-making rights and therefore must be considered carefully. Guardianship may include, but is not limited to, overseeing services, arranging for community or institutional placement, managing estates, and making medical decisions.
The purpose of the guardianship program under Human Resources Code Section 161.101 is to provide guardianship services to:
- Incapacitated children upon reaching the age of 18 who have been in CPS conservatorship and appear to meet the adult definition of incapacity;
- Incapacitated adults age 65 or older, or between the ages of 18-65 with a disability, who were referred by APS following an investigation in which abuse, neglect (including self-neglect), or exploitation was confirmed, and no other means of protecting the person is available and there is some indication the individual lacks capacity; and
- Incapacitated individuals referred directly to the program by a court with probate authority under certain criteria established in statute or rule.
In order for HHSC to provide guardianship services, less restrictive alternatives must not be available; an appropriate and qualified alternate guardian must not be available and willing to serve; the individual under guardianship must have resources available to fund the services, including long-term care; and there must be an expectation that guardianship will meet the person’s needs.
During the 86th legislative session, the following bills passed related to the guardianship process in Texas:
- SB 31 (Zaffarini/Smithee) directed the Office of Court Administration of the Texas Judicial System to establish and maintain a guardianship abuse, fraud, and exploitation deterrence program designed to provide additional resources and assistance to courts that have jurisdiction over guardianship proceedings.325
- SB 536 (Zaffirini/Murr) and SB 667 (Zaffirini/Thompson) both passed but were ultimately vetoed by the Governor.
- SB 536 would have created a system of regional specialized courts with jurisdiction over guardianship proceedings and protective services proceedings to be served by associate judges appointed by the presiding judge of each administrative judicial region. The Governor’s veto stated that the bill was “misguided in its attempt to a create an expensive new system,” and the legislature needs to “find a better way to address the issue.”
- SB 667 would have revised and updated provisions governing probate and guardianship matters, and procedures for persons who are incapacitated or have a mental illness. Additionally, it would have authorized the commissioners’ court of a county to create an office of public guardian to provide certain guardianship services to incapacitated persons or enter into an agreement with a person operating a nonprofit guardianship program or private professional guardianship program to act as a public guardian for such purposes. The Governor’s veto stated that while the bill made improvements to the probate and guardianship process, the creation of new public guardianship offices controlled by counties was unnecessary because “private attorneys are capable of handling these cases without the expense of this new bureaucracy.”
Health and Developmental Services
EARLY CHILDHOOD INTERVENTION (ECI) SERVICES
Early interventions have the potential to mitigate the impact of developmental delays that can lead to later physical, cognitive, and behavioral challenges. Providing Early Childhood Intervention (ECI) services to families and children at an early stage in development can reduce the cost of special needs services later in the child’s life, as well as enable families to provide support to their special needs children and counter environmental risk factors.
ECI is authorized by Part C of the Individuals with Disabilities Education Act. Part C is a federal grant program that assists states in operating a statewide early intervention program for infants and toddlers ages zero to three. State general revenue funds are required to draw down federal funding for ECI programs. Direct state appropriations for ECI in Texas decreased 11 percent from $166 million in FY 2011 to $148 million in FY 2018. Prior to the 86th legislative session, HHSC requested an increase of $72.6 million for ECI. While the legislature decided to fund a partial increase of $31 million, the increase was the largest in many years.
In 2019, Texas lawmakers also attempted to pass legislation that would have improved access to ECI services. HB 12 (Davis), and similarly SB 2225 (Zaffirini), would have created an ECI telehealth pilot program, required some health plans to cover specified ECI services that are Medicaid-reimbursable, and created a provider ombudsman in the HHSC. HB 1635 (Miller) and SB 1956 (Zaffirini) would have extended insurance coverage to require most private insurance companies to cover certain ECI services. However, these legislative actions did not pass.331 The COVID- 19 pandemic created some flexibility in ECI services provided remotely through telehealth, although HHSC has not indicated any long-term continuation of this method.
A Child’s Journey through ECI
Getting Started
1. Referral
2. First Visit
3. Evaluation and Assessment
Next Steps: ECI Services
Individualized Family Service Plan (IFSP) Meeting and Individualized Family Service Plan Development (must be written within 45 days of the ECI referral)
5. ECI Service Delivery Begins (within 28 days of signing the IFSP)
6. Review of Child’s Progress (occurs regularly, but family can request at any time)
Future Steps: Leaving ECI
7. Children must transition out of ECI by their third birthday (or when deemed no longer necessary; transition planning should begin after age 2)
Source: Texas Health and Human Services. (n.d.). ECI parent handbook. Retrieved from http://www.mhmrtc.org/Portals/0/PDF/ECI_Document_ParentHandbook_English.pdf
Eligibility
To determine eligibility for ECI services, a team of at least two professionals from different disciplines performs a comprehensive evaluation of a child’s abilities. Generally, eligibility is determined by a child meeting at least one of following three criteria:
- Medically diagnosed condition: Children with medical diagnoses that are likely to cause developmental delays and have a need for services. For a list of diagnoses that qualify for ECI see https://diagsearch.hhsc.state.tx.us/
- Auditory or visual impairments: Children with auditory or visual impairments as defined by the Texas Education Agency (TEA).
- Developmental delays: Children with developmental delays of at least 25 percent that affect function in one or more areas of development (social emotional, self-help, communication, motor functions, or cognitive skills).
An ECI team evaluates a child for developmental delay using the Battelle Developmental Inventory, 2nd edition. If the child qualifies for services, a team identifies the family’s daily routine and the child’s strengths and needs. Based on the results of this evaluation, ECI professionals and the child’s family work as a team to develop an individualized family service plan. The plan may include a range of services such as evaluation, service planning, family counseling, therapy services (such as occupational, physical, and speech therapy), nutrition services, and psychological and social work services. The services provided are meant to be family-centered and be provided in familiar settings.
Services, Utilization, and Costs
Eligible children can participate in ECI regardless of their income level and certain ECI services are free of charge, including evaluation and assessment, case management, IFSP development, and translation and interpreter services.336 ECI is a cost share program, meaning that families with the ability to pay are expected to contribute financially to the cost of services. Children on Medicaid or in foster care or kinship care receive all ECI services free of charge. State regulations require ECI to collect payment through the child’s private or public health insurance or charge up to a maximum amount. Some families pay for ECI services on a sliding scale basis. Family income, family size, the child’s foster care status, and public and private health insurance are taken into account when arriving at a maximum monthly charge for ECI services. Families will not be turned away due to an inability to pay.337 In FY 2019, 60,596 children of the 88,195 children referred received comprehensive ECI services.338 Table 50 provides data on recipients of ECI services.
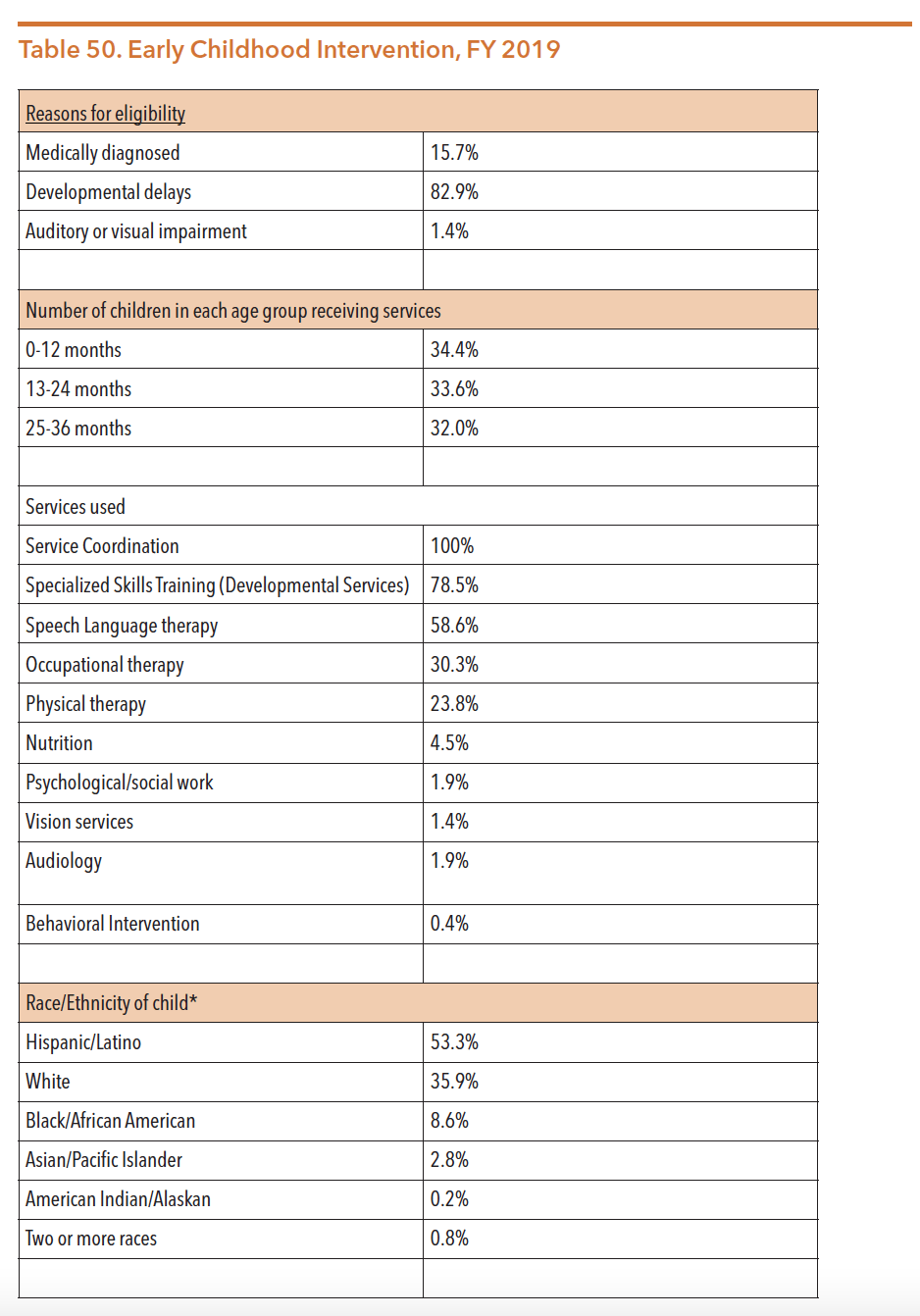
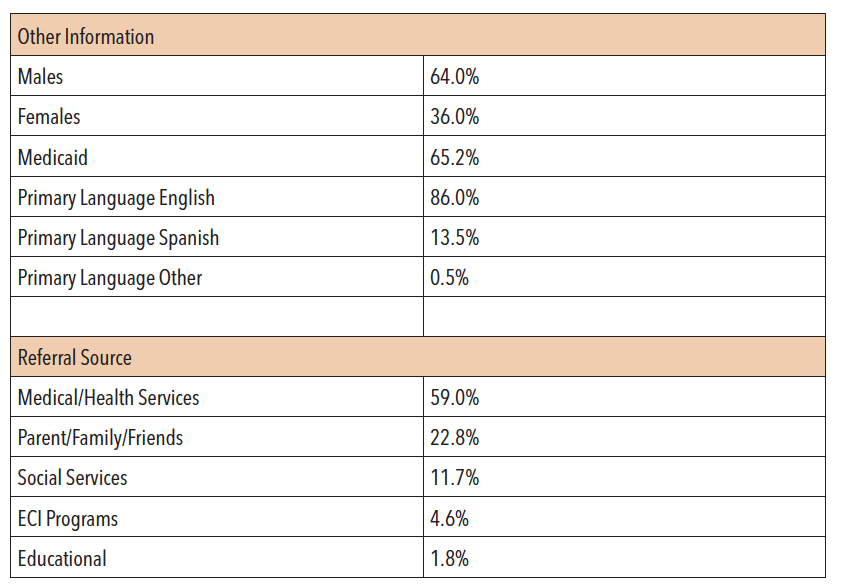
Source: Texas Health and Human Services Commission (2020). ECI data & reports. https://hhs.texas.gov/doing-business-hhs/provider-portals/assistive-services-providers/early-childhood-intervention-eci-programs/eci-data-reports
AUTISM PROGRAM
The following description was captured from the HHSC website (retrieved from https://hhs.texas.gov/services/disability/autism:
Autism spectrum disorder (ASD) is the fastest growing serious, developmental disability, affecting an estimated 1 out of 59 children in the United States. With this number growing at a significant rate, there continues to be an unmet need for services. The Health and Human Services Autism Program champions excellence in the delivery of services for families of children with autism. Services are provided through grant contracts with local community agencies and organizations that provide applied behavioral analysis (ABA) and other positive behavior support strategies. The program helps improve the quality of life for children on the autism spectrum and their families.
The Autism Program started as a pilot project in FY 2008 and was intended to extend treatment services, including applied behavior analysis (ABA), to children ages 3 through 8 with a diagnosis on the autism spectrum. On September 1, 2014, rules were adopted with two ABA services for children: comprehensive ABA services for children aged 3 through 5 years and focused ABA services for children aged 3 through 15 years. Other changes included parent participation, child attendance, and additional staff training requirements. The Comprehensive ABA treatment services were phased out during the 2016-2017 biennium and no longer existed after August 31, 2017. During the 86th legislature, over $14 million for FY 20-21 was allocated for ABA treatment services. However, those funds were directed to only be available for children enrolled in the focused program. Additionally, Rider 32 stated that if HHSC moved forward with adding intensive behavioral intervention (IBI) as a Medicaid benefit for persons under age 20 with a diagnosis of Autism spectrum condition, funds would be allowable to reimburse for provision of IBI services.
Table 51 provides data on the number of children served, the average cost per child, and the number of program sites in Texas.
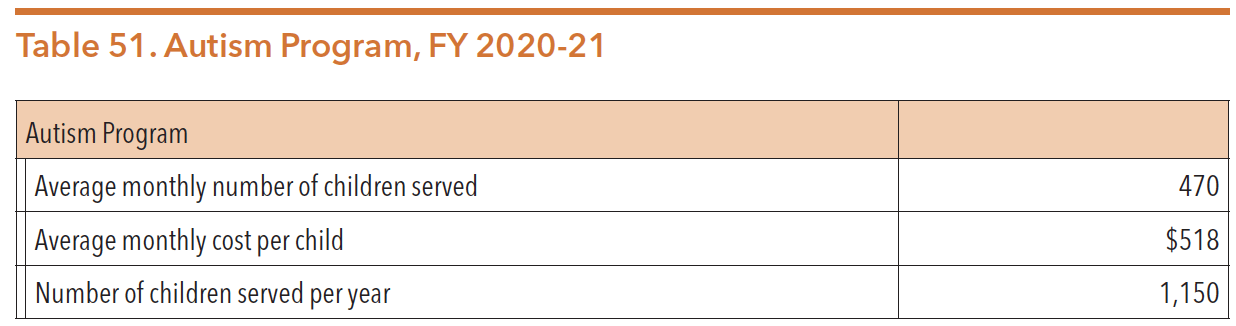
Source: Texas Legislature Online (2019). H.B.1, General Appropriations Act, 86th Legislature, FY 2020-21. Retrieved from https://capitol.texas.gov/tlodocs/86R/billtext/pdf/HB00001F.pdf#navpanes=0
Access and Eligibility Services
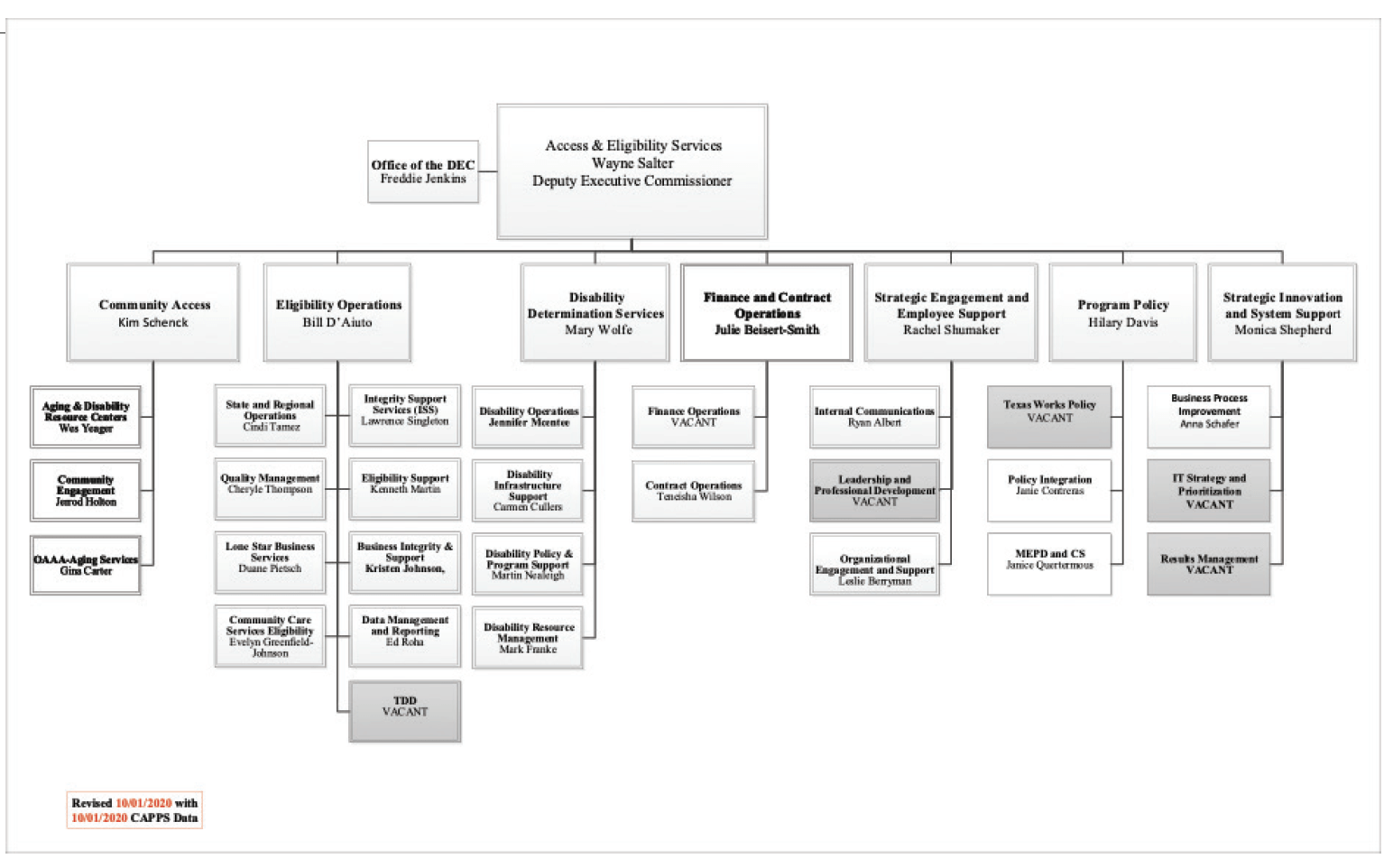
Source: Texas Health and Human Services Commission. (October 2020). Public Information Request, October 2020.
Individuals living with mental health and substance use conditions are often eligible for federal disability benefits. However, accessing those benefits can be a challenging and confusing process. While Supplemental Security Income (SSI) and Social Security Disability Insurance (SSDI) are federally funded programs, disability determination for these services is conducted by the state through contracts with the federal government. Responsibility for disability determination is housed in the Access & Eligibility Services Division of HHSC.
In addition to conducting disability determination reviews for federal benefits, the division also partners with community organizations that assist low-income families applying for basic services such as obtaining food subsidies, temporary assistance to needy families, and Medicaid and CHIP services. With the assistance of Regional Community Relations specialists, communities work to improve access to the Medicaid and CHIP services often needed by individuals living with serious mental illness or children/youth with SED. A directory of these Regional Partnership Specialists can be found at https://hhs.texas.gov/about-hhs/community-engagement/office-community-access-services.
DISABILITY DETERMINATION SERVICES
The disability decision-making process begins when an individual files an application for benefits. Determination is then made if the applicant meets the nonmedical requirements for benefits, such as age and work credits. If those requirements are met, the application is sent to the Disability Determination Services (DDS) office. The DDS then decides whether an individual is disabled under Social Security law. The definition of disability under Social Security differs from other disability programs and does not pay benefits for partial or short-term disability. Section 223(d)(1) of the Social Security Act defines disability as an:
- A – Inability to engage in any substantial gainful activity by reason of any medically determinable physical or mental impairment which can be expected to result in death or which has lasted or can be expected to last for a continuous period of not less than 12 months, or
- B – In the case of an individual who has attained the age of 55 and is blind (within the meaning of blindness as defined in section 216(i)(1)), inability by reason of such blindness to engage in substantial gainful activity requiring skills or abilities comparable to those of any gainful activity in which the individual has previously engaged with some regularity and over a substantial period of time.
Benefits are available for both adults and children who meet eligibility include Social Security Disability Income (SSDI) and SSI. Both SSI and SSDI are cash assistance programs administered by the federal Social Security Administration (SSA). HHSC staff makes the initial disability determination for Texans applying for SSDI and/or SSI. Assistance applying for these cash assistance programs can be found at https://www.ssa.gov/disability/determination.htm.
Some people with serious mental health conditions will qualify for either SSDI or SSI. Qualifying for both SSDI and SSI benefits at the same time is called “concurrent benefits,” according to the Social Security Administration. While concurrent benefits are not common, they are possible if an individual worked enough at some point in his or her life to have the required number of work credits.
SOCIAL SECURITY DISABILITY INSURANCE
SSDI is governed by rules set out in Title II of the Social Security Act and covers workers age 18 to 65 who have a disability, widows/widowers of workers with a disability, and adult children (with a disability) of workers with sufficient work histories.344 People become eligible for SSDI throughout their working lives by paying social security taxes.345 Approval for SSDI payments results in eligibility for Medicare coverage after a two-year waiting period.
SUPPLEMENTAL SECURITY INCOME
SSI is governed by rules set out in Title XVI of the Social Security Act. SSI provides monthly stipends to qualifying low-income adults who have a disability, are blind, or are over the age of 65. Additionally, an individual must meet additional requirements including having limited resources and cannot be in a government-funded hospital or prison. Children who have a disability or are blind may also qualify for SSI when they are not married nor head of a household, under the age of 18, or under the age of 22 while regularly attending school. Unlike SSDI, SSI is not based on an individual’s work history. The monthly maximum amounts for 2020 are $783 for an eligible individual and $1,175 for an eligible individual with an eligible spouse. Once approved for SSI, participants are eligible for Medicaid. According to the Social Security Administration, in January 2019 approximately 7.97 million individuals were receiving SSI benefits in the U.S, a decrease of 98,000 recipients from 2018. It is estimated that by 2043, the number of recipients will be closer to 8.7 million.
People who disagree with their SSI or SSDI determination have a legal right to appeal the decision online or in writing. There are four levels of appeal:
- Reconsideration: Another disability examiner and medical team reviews the case to determine if the decision was proper. Claimants may submit additional evidence to support their case.
- Administrative Hearing: Claimants may present witnesses and evidence at a formal, private hearing with an administrative law judge.
- Social Security Appeals Council Hearing: Reviews decisions by judges at the administrative hearing level.
- U.S. Federal District Court: A hearing at the federal court level; very few cases reach this level.
According to a report by the SSA that tracked SSDI outcomes from 2008-2017, the number of applicants who were granted awards upon initial review averaged 22 percent. Of those who appealed their denial, 2 percent of applicants were subsequently granted benefits at the reconsideration state and 9 percent through a hearing.
ELIGIBILITY
Eligibility for both SSDI and SSI is conditioned on the determination that an individual has a disability that prevents his or her ability to work. Like serious physical conditions, mental health conditions can be considered a disability and may allow an individual to access SSDI or SSI cash benefits if they meet other eligibility criteria. Initial disability determinations are made by disability officers within the DDS Division.
According to a 2019 report by the SSA, mental health conditions constituted about one-quarter of the national SSDI diagnoses in 2018. Disability determinations for SSDI on the basis of a mental health condition are categorized as:
- Neurocognitive conditions
- Schizophrenia spectrum and other psychotic conditions
- Depressive, bipolar and related conditions
- Intellectual disability
- Anxiety and obsessive-compulsive conditions
- Somatic symptom and related conditions
- Personality and impulse-control conditions
- Autism Spectrum conditions
- Neurodevelopmental conditions
- Eating disorders
- Trauma-and-stressor related conditions
Each of these categories includes a set of criteria that must be satisfied in order to qualify for SSDI. Monthly benefits for SSDI are dependent on the social security earnings record of the worker. There is no minimum SSDI monthly benefit; the monthly maximum benefit depends on the age at which a worker left the workforce due to his or her disability. The SSA makes the final admission decision on eligibility after consideration of a more exhaustive set of eligibility criteria.360 To be eligible for SSI, adults and children must meet strict financial and functional criteria in addition to having a disability (including mental health conditions).361
Additional information on eligibility criteria and how to apply is available on the Social Security website at http://www.ssa.gov.