RWJF: A Multidimensional Framework
for Patient and Family Engagement
in Health and Health Care (click to enlarge)
A Robert Wood Johnson Foundation brief highlighted an area that does not get enough attention in the health care reform dialogue: patient engagement (PE). Yes, we talk about it. Our friends at the RWJF are sharing first-hand accounts and lessons learned from grantee organizations that successfully implemented patient engagement strategies.
The brief highlights that the most successful patient engagement programs require three essential components: transparency, engagement and collaboration.
- Transparency: Programs found that increased transparency helped patients understand the system and how it worked. The brief states “The groups have found that clear expectations, structured meetings and asking patients for feedback through meeting evaluations increases the satisfaction of both patients and clinicians.”
- Engagement: Patients involved in their own care do a much better job of effectively communicating their own needs, according to the brief. One grantee created a Patient and Public Engagement Council to give providers feedback and foster patient-physician relations.
- Collaboration: One grantee offered workshops to assist patients to learn management strategies for chronic conditions, such as diabetes, high cholesterol, heart conditions and obesity. “Initially, the program relied on word-of-mouth recommendations from enthusiastic alumni, public service announcements and newspaper articles to recruit attendees,” the brief states. “Those efforts didn’t go far enough, however, so program leaders began working with health care clinics to refer patients with chronic illnesses.”
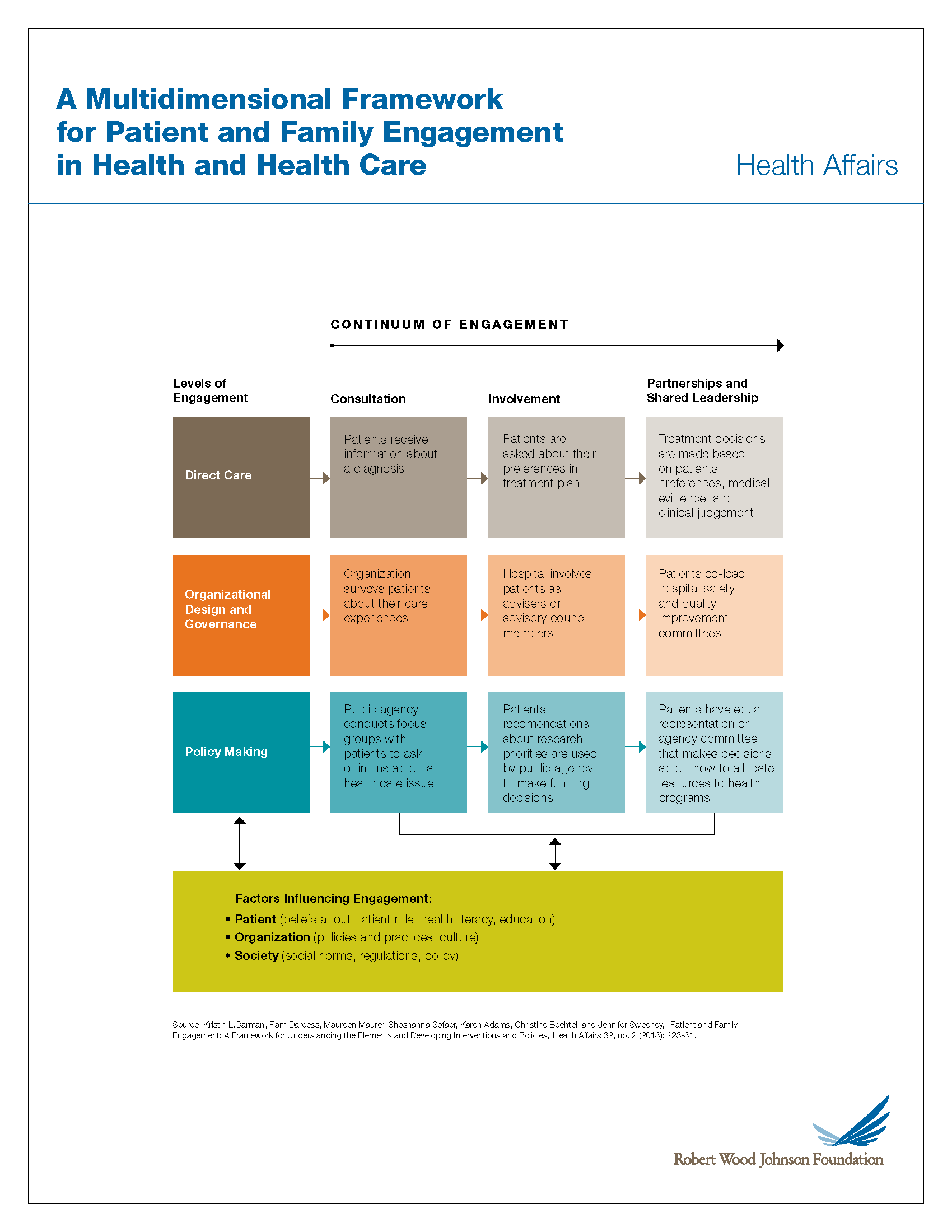
Patients tend to group in three levels of engagement, according to a framework developed by American Institutes for Research. There are first-level patients, who begin to engage in their own care; second-level patients, who actively give providers their important input and collaborate in their care; and third-level patients, who work to improve care delivery at the institutional and regulatory level. The framework illustrates how patient engagement can influence improved patient activation, organizational transformation and policy change, all leading to better health outcomes, better health care systems and healthier communities. Isn’t that the end game?
The implementation of this framework will be even more critical to mental health and behavioral health systems. Active engagement in treatment contributes to better health outcomes. This framework will help pave the road towards system reform, health and mental/behavioral health.
So all consumers of health and mental/behavior health care (reminder: we are all consumers of health care): GET ENGAGED! It’s one way to contribute to changing the health care system and making it truly patient centered and patient driven.
