Policy Brief: Integrated Health Care
Overview
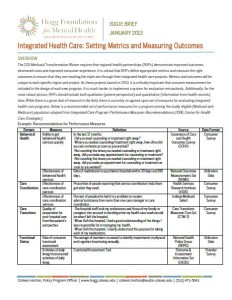
The 1115 Medicaid Transformation Waiver requires that regional health partnerships (RHPs) demonstrate improved outcomes, decreased costs and improved consumer experience. It is critical that RHPs define appropriate metrics and measure the right outcomes to ensure that they are reaching the triple aim through their integrated health care projects. Metrics and outcomes will be unique to each specific region and project. As these projects launch in 2013, it is critically important that outcome measurement be included in the design of each new program. It is much harder to implement a system for evaluation retroactively. Additionally, for the most robust picture, RHPs should include both qualitative (patient perspective) and quantitative (information from health records) data. While there is a great deal of research in the field, there is currently no agreed-upon set of measures for evaluating integrated health care programs. Below is a recommended set of performance measures for a program serving the dually eligible (Medicaid and Medicare) population adapted from Integrated Care Program: Performance Measures Recommendations (2006, Center for Health Care Strategies).